Weight Gain Mechanism: How Medications, Metabolism, and Health Conditions Interact
When your body gains weight, it’s rarely just about eating too much or moving too little. The weight gain mechanism, the biological process by which the body stores excess energy as fat. Also known as energy balance disruption, it’s influenced by hormones, metabolism, stress, and yes—medications. Many people don’t realize that common drugs for depression, diabetes, high blood pressure, and even allergies can quietly shift your body’s fat storage system. This isn’t laziness. It’s biology.
Take insulin, a hormone therapy used to manage blood sugar in type 1 and type 2 diabetes. It helps cells absorb glucose, but it also tells your body to store extra energy as fat. That’s why some people gain weight when they start insulin—it’s not overeating, it’s the drug doing its job too well. Then there’s antidepressants, medications that alter brain chemicals to improve mood. Drugs like amitriptyline or paroxetine can increase appetite and slow metabolism. You might not feel hungrier, but your body starts holding onto calories differently. Even corticosteroids, anti-inflammatory drugs often used for asthma or autoimmune conditions, cause fluid retention and increased fat deposition around the abdomen. These aren’t side effects you can ignore—they’re part of how the drug works.
It’s not just drugs. Conditions like hypothyroidism, polycystic ovary syndrome (PCOS), and chronic stress trigger hormonal shifts that directly affect how your body stores fat. Cortisol, the stress hormone, tells your body to hoard energy—especially around your midsection. When you combine this with medication-induced changes, the weight gain becomes layered. Some people gain 10 pounds in months without changing their diet. That’s not weakness. That’s physiology.
What you’ll find in the posts below are real-world insights into how specific medications trigger these changes, what alternatives exist, and how to work with your doctor to manage weight without stopping treatment. You’ll see how medication-induced weight gain is tracked, reported, and sometimes avoided with smarter choices. There’s no magic fix, but there are clear steps—backed by FDA reports, clinical studies, and patient experiences—that help you understand what’s really happening inside your body.
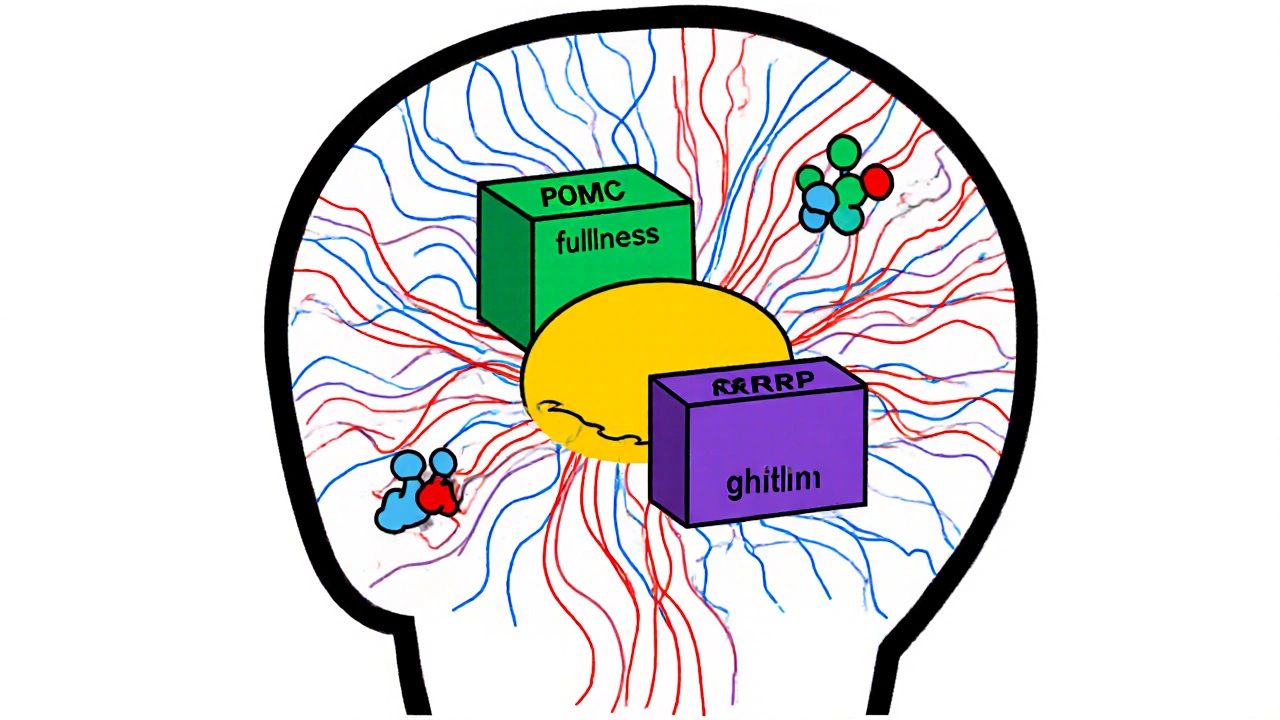
Obesity is not just about eating too much-it's a disease of broken hunger signals and metabolic dysfunction. Learn how leptin resistance, brain pathways, and hormones like ghrelin and insulin drive weight gain and make weight loss so hard.