Vertigo: What It Is and How to Manage It
When dealing with Vertigo, a sensation that the world is spinning or moving while you stay still. Also known as spinning dizziness, it often pops up during daily activities and can be unsettling. Vertigo isn’t a disease itself; it’s a symptom that points to an underlying issue in the balance system. One of the most common companions is dizziness, which describes a broader range of light‑headed feelings. Another closely linked condition is Ménière's disease, a disorder of the inner ear that causes episodes of intense vertigo, hearing loss, and ringing in the ears. Finally, vestibular migraine can trigger vertigo attacks even without a headache, showing how headaches and balance problems often intersect.
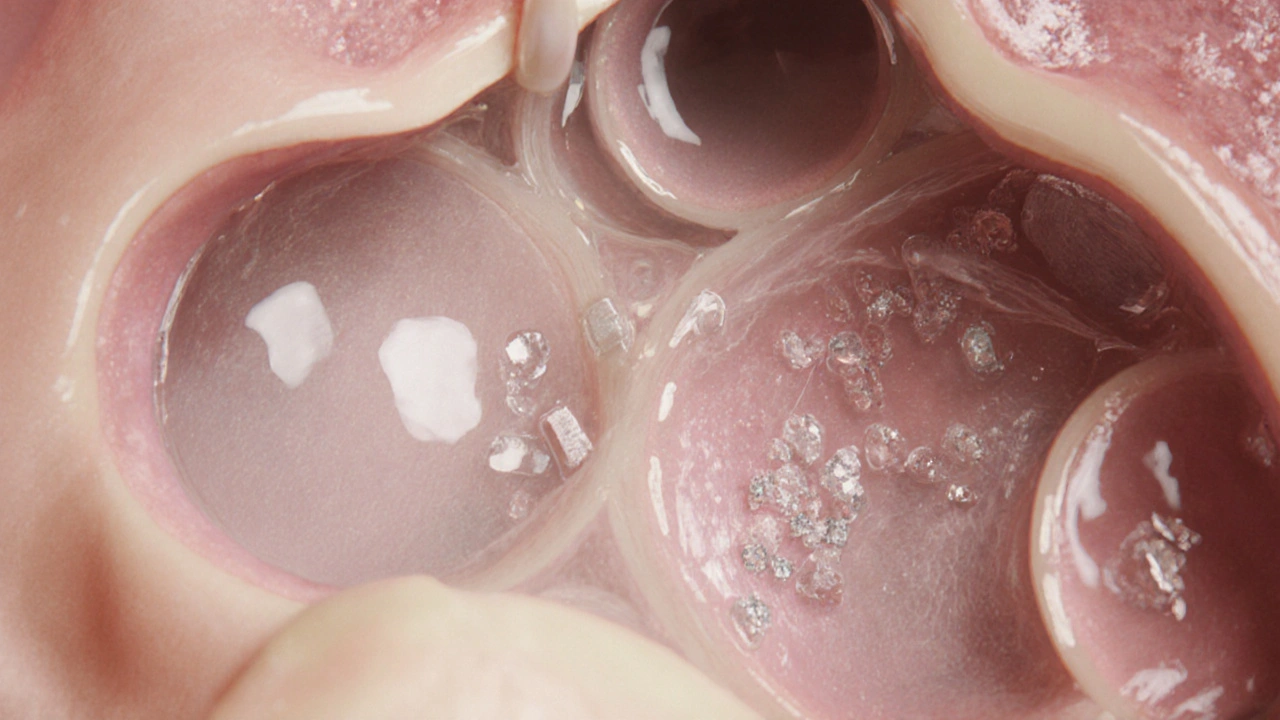
Vertigo encompasses several subtypes, each with its own trigger. The most frequent cause is a problem in the inner ear, where tiny fluid‑filled canals help the brain sense motion. When those canals send mixed signals, you get that spinning feeling. Inner‑ear infections, ear‑wax buildup, or inflammation can all start the cascade. Another major source is the brain’s vestibular pathways; strokes, multiple sclerosis, or brain tumors can disrupt signals and produce vertigo. Even certain medications—like high‑dose antibiotics or antihistamines—can tip the balance by affecting the inner‑ear fluid or nerve signals.
How to Tell What’s Behind Your Vertigo
Diagnosing vertigo means matching symptoms to possible causes. Doctors start by asking when the sensation began, how long it lasts, and whether it’s triggered by head movement. They’ll look for associated signs such as ringing in the ears (tinnitus), hearing loss, nausea, or headaches. Simple tests like the Dix‑Hallpike maneuver help spot benign paroxysmal positional vertigo (BPPV), a common type caused by displaced calcium crystals in the ear. If the test is positive, a quick series of head movements can often settle the crystals and stop the spinning. For more complex cases, an audiogram checks hearing, while MRI scans examine the brain’s balance centers.
Once the origin is clear, treatment follows a predictable pattern: address the cause, relieve symptoms, and prevent recurrence. For BPPV, canalith repositioning exercises like the Epley maneuver are first‑line and work in minutes. If Ménière's disease is the culprit, doctors may prescribe a low‑salt diet, diuretics, and sometimes intratympanic steroid injections to control fluid buildup. Vestibular migraine often responds to migraine preventatives such as beta‑blockers or CGRP inhibitors, plus lifestyle tweaks like regular sleep and stress management. When vertigo stems from medication side effects, adjusting the dose or switching drugs can end the problem.
Medications that directly target vertigo also exist. Antihistamines such as meclizine calm the inner‑ear signals, while anticholinergics like scopolamine work on the brain’s nausea centers. Betahistine, a histamine analogue, improves blood flow in the inner ear and is popular in Europe for Ménière's disease. Steroids, either oral or injected into the ear, reduce inflammation that might be irritating the vestibular nerve. It’s worth noting that these drugs often provide short‑term relief; long‑term management relies on treating the underlying condition and using physical therapy to retrain balance.
Physical therapy, especially vestibular rehabilitation, is a game‑changer for many people. A therapist guides you through specific head and eye movements that help the brain re‑learn balance cues. Over weeks, the brain compensates for the faulty ear signals, reducing vertigo frequency and severity. Home exercises—like focusing on a fixed point while moving the head—can keep the progress going. Even simple balance drills, such as standing on one foot or walking heel‑to‑toe, boost confidence and cut fall risk.
Beyond medical steps, everyday habits can lessen vertigo attacks. Staying well‑hydrated prevents low blood pressure, which can trigger dizziness. Eating small, regular meals stops blood‑sugar dips that sometimes cause light‑headedness. Reducing caffeine and alcohol intake avoids dehydration and inner‑ear irritation. When you feel an attack coming, sit or lie down, keep your eyes open, and focus on a stationary object. This technique, called “visual fixation,” helps the brain override mismatched signals and can stop the spinning faster.
Vertigo isn’t just a physical issue; it can shake confidence and limit activities. Knowing when it’s safe to drive, climb stairs, or work out is essential. Many doctors advise a short period of observation after a severe spell—usually 24 hours—before returning to high‑risk tasks. If you experience sudden, severe vertigo with double vision, chest pain, or difficulty speaking, seek emergency care; those signs may point to a stroke or other serious condition.
All of this information sets the stage for the articles below. Below you’ll find detailed guides on specific medications, side‑effect profiles, and practical tips that match the range of vertigo causes we’ve outlined. Whether you’re looking for a quick fix for BPPV, a deep dive into Ménière's disease treatments, or ways to manage vestibular migraine, the collection has you covered.
Learn what vertigo is, its main causes, key symptoms, and proven treatments. Get clear steps to diagnose, manage, and prevent spinning sensations.