Key Takeaways
- Vertigo is a spinning sensation caused by inner‑ear or brain issues.
- Benign Paroxysmal Positional Vertigo, Meniere’s disease, vestibular migraine and vestibular neuritis account for most cases.
- Typical symptoms include dizziness, nausea, balance loss, and ringing in the ears.
- Simple repositioning maneuvers, medication, and vestibular rehab can clear most episodes.
- Seek urgent care if symptoms are sudden, severe, or accompanied by vision loss or weakness.
What Exactly Is Vertigo?
When we talk about Vertigo is a sense of spinning or that the room is moving, usually caused by a disturbance in the inner ear or brain pathways that control balance. It isn’t the same as general dizziness; it feels like the world is actually turning around you.
How the Balance System Works
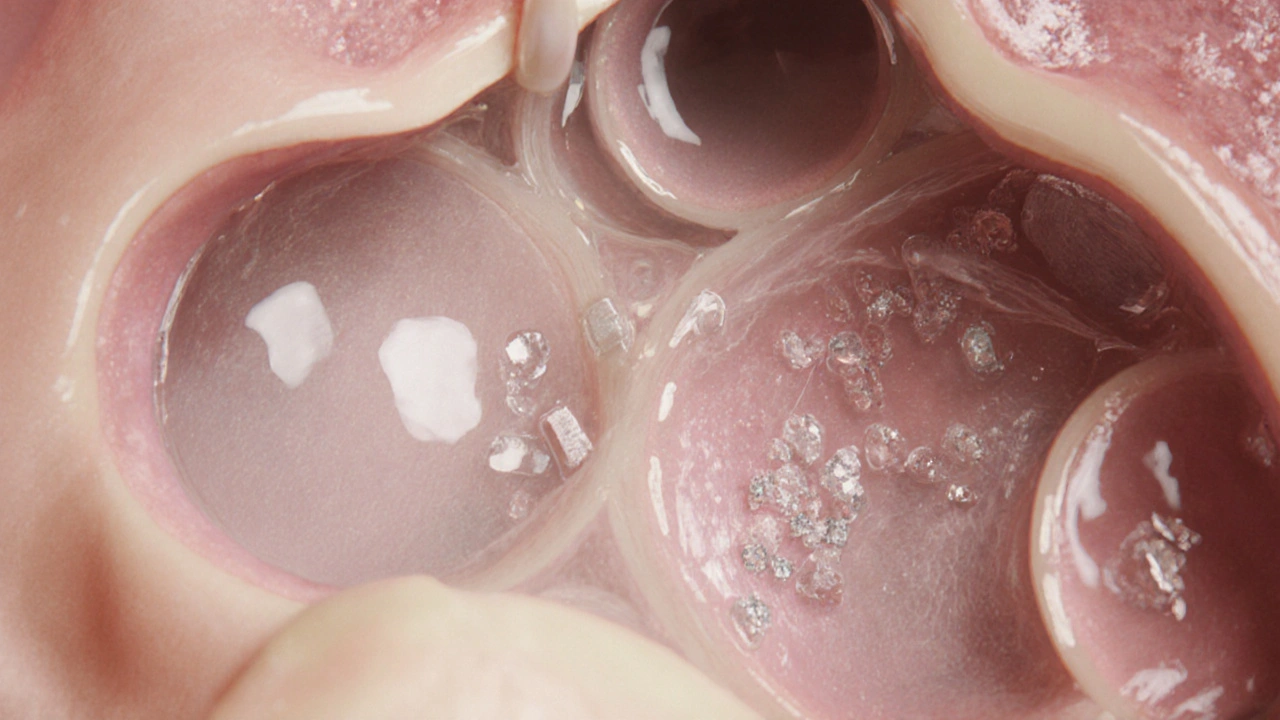
The body’s balance center lives in the inner ear, a fluid‑filled maze that sends motion signals to the brain through the vestibular nerve. Tiny crystals sit on hair‑like sensors; when they shift, the brain interprets the movement. If these crystals move out of place or the fluid leaks, the brain receives mixed messages, and vertigo erupts.
Common Causes of Vertigo
Most vertigo cases fall into a handful of well‑studied conditions. Below is a quick snapshot of the big players.
| Condition | Typical Cause | Episode Duration | Common Associated Symptoms | First‑Line Treatment |
|---|---|---|---|---|
| Benign Paroxysmal Positional Vertigo (BPPV) | Displaced calcium crystals in the semicircular canals | Seconds to minutes | Brief spinning when lying down or looking up, nausea | Epley or Semont repositioning maneuver |
| Meniere’s disease | Fluid buildup in the inner ear (endolymphatic hydrops) | 20 minutes to several hours | Low‑frequency hearing loss, ringing (tinnitus), ear fullness | Low‑salt diet, diuretics, vestibular suppressant meds |
| Vestibular migraine | Migraine‑related changes in blood flow to vestibular pathways | Minutes to days | Headache, light/noise sensitivity, visual aura | migraine prophylaxis (beta‑blockers, topiramate) and vestibular rehab |
| Vestibular neuritis | Inflammation of the vestibular nerve, often viral | Days to weeks | Constant dizziness, imbalance, mild nausea, no hearing loss | Corticosteroids, anti‑nausea meds, vestibular rehab |
Recognizing Vertigo Symptoms
Symptoms can vary, but most people notice a few key signs:
- Spinning or swaying sensation, especially when moving the head.
- Feeling off‑balance while standing or walking.
- Nausea or vomiting.
- Ringing in the ear (tinnitus) or a feeling of ear fullness.
- Blurred vision or trouble focusing.
If any of these appear suddenly, it’s wise to pause activities that could be dangerous-driving, operating heavy machinery, or climbing stairs.
When to Seek Medical Help
Most vertigo episodes resolve with simple at‑home maneuvers. However, urgent care is needed if you notice:
- Severe headache that awakens you at night.
- Vision loss, double vision, or drooping facial muscles.
- Weakness or numbness in arms or legs.
- Sudden hearing loss or constant ringing.
- Symptoms that last longer than a week without improvement.
These signs could point to a stroke, brain tumor, or other serious condition, and a prompt evaluation can be lifesaving.
How Doctors Diagnose Vertigo
The diagnostic process usually starts with a detailed history and physical exam. An audiologistspecialist who tests hearing and balance function may perform:
- Head‑impulse test - checking eye movements as the head is turned quickly.
- Romberg and tandem‑walk tests - assessing balance with eyes closed.
- Dix‑Hallpike maneuver - provoking BPPV by moving the head into specific positions.
Imaging like MRI may be ordered if neurological issues are suspected. Blood work can rule out infections or autoimmune causes.

Treatment Options
Effective treatment hinges on the underlying cause.
Repositioning Maneuvers
For BPPV, the Epley or Semont maneuvers guide displaced crystals back into their proper canal. A trained physical therapistwho specializes in vestibular rehabilitation can teach you the steps, and many patients feel better after a single session.
Medication
When the cause is inflammation (vestibular neuritis) or excess fluid (Meniere’s), doctors may prescribe:
- Corticosteroids - to dampen nerve swelling.
- Diuretics - to reduce inner‑ear fluid buildup.
- Vestibular suppressants (meclizine, ondansetron) - to control severe nausea and spinning.
- Migraine preventatives - for vestibular migraine.
Vestibular Rehabilitation Therapy (VRT)
VRT is a series of customized exercises that help the brain relearn balance cues. It’s useful for chronic cases, especially after vestibular neuritis or when BPPV recurs.
Lifestyle Adjustments
Simple habits can reduce the frequency of attacks:
- Limit salty foods and caffeine.
- Stay hydrated - dehydration can trigger dizziness.
- Avoid rapid head movements; rise slowly from lying or seated positions.
- Use a night‑light if darkness worsens your symptoms.
Preventing Future Episodes
While not all vertigo is preventable, you can lower risk by:
- Managing stress - chronic stress can flare vestibular migraine.
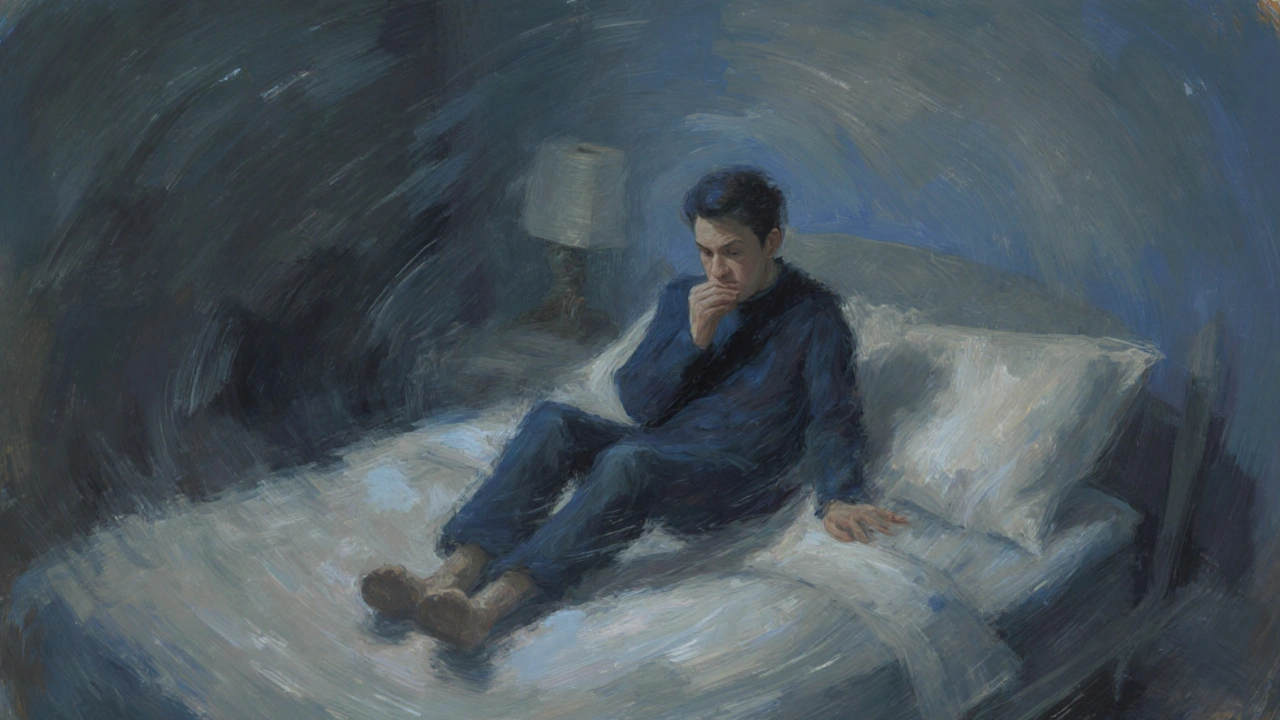
- Ensuring good sleep hygiene - sleep deprivation impacts balance pathways.
- Regular ear check‑ups if you have a history of Meniere’s or BPPV.
- Practicing balance‑enhancing activities like yoga or tai chi.
Quick Self‑Check: Is It Vertigo?
Ask yourself these three questions:
- Do I feel like the room is spinning, not just myself?
- Does the sensation worsen with head movement or when I lie down?
- Do I have accompanying ear symptoms (tinnitus, fullness) or a headache?
If you answered yes to most, it’s likely vertigo and you should consider the steps above.
Frequently Asked Questions
Can vertigo be a sign of something serious?
Yes. While most cases are benign, sudden, severe vertigo with weakness, vision loss, or speech difficulties may indicate a stroke or brain tumor. Seek emergency care if you notice these red‑flag symptoms.
What’s the difference between vertigo and dizziness?
Vertigo is the false sensation that you or your surroundings are spinning. Dizziness is a broader term that includes light‑headedness, faintness, or loss of balance without the spinning feeling.
How many times can I do the Epley maneuver at home?
Most people see relief after one to three attempts. If symptoms persist after three tries, schedule an appointment with a physical therapist or ENT specialist.
Is medication always needed for vertigo?
No. Many cases, especially BPPV, respond to repositioning maneuvers alone. Medications are generally reserved for severe nausea, inflammation, or migraine‑related vertigo.
Can lifestyle changes really help?
Absolutely. Reducing salt, staying hydrated, managing stress, and practicing balance exercises can lessen the frequency and intensity of attacks, especially for Meniere’s disease and vestibular migraine.
Comments (18)
Patrick McVicker
October 12, 2025 AT 02:57
Cheers for the clear rundown – the Epley trick really does the job! 😊
Liliana Phera
October 15, 2025 AT 00:24
Vertigo, in its relentless spin, serves as a stark reminder of how fragile our sensory equilibrium truly is.
When the inner ear sends mixed messages, the brain scrambles to reconcile reality, leading to that unsettling sensation of the world rotating.
It is not merely a nuisance; it can dismantle one's confidence in simple movements like standing up or turning the head.
One must recognize that underlying causes range from displaced otoconia in BPPV to the fluid overload of Meniere’s disease, each demanding distinct interventions.
The Epley maneuver, though simple, epitomizes how a precise physical technique can restore order where pharmaceuticals fall short.
Yet, for vestibular migraines, the pathology is rooted in neurovascular dysregulation, calling for prophylactic migraine therapies rather than repositioning.
Inflammation of the vestibular nerve, as seen in vestibular neuritis, betrays viral triggers, and corticosteroids may mitigate the swelling.
Critically, red‑flag symptoms like sudden vision loss, facial droop, or limb weakness cannot be ignored-they herald cerebrovascular emergencies.
Prompt neuroimaging in such scenarios distinguishes peripheral vertigo from central stroke, a distinction that can be life‑saving.
Patients often underestimate the psychological toll: chronic dizziness fuels anxiety, which in turn exacerbates vestibular imbalance-a vicious feedback loop.
Lifestyle nuances, such as limiting sodium, staying hydrated, and managing stress, wield measurable influence on attack frequency.
Balance training through vestibular rehabilitation re‑educates the central nervous system, fostering neuroplastic compensation.
Healthcare providers should adopt a systematic approach: detailed history, targeted bedside maneuvers like Dix‑Hallpike, and judicious use of imaging when central signs emerge.
Education empowers sufferers to execute maneuvers at home, reducing emergency visits and healthcare costs.
Ultimately, mastering vertigo hinges on integrating precise diagnostics, tailored therapy, and patient education into a cohesive care plan.
Dean Briggs
October 17, 2025 AT 21:50
Having lived through several BPPV episodes, I can attest that the repositioning maneuvers are surprisingly effective when performed correctly.
The key is to move the head slowly and follow the prescribed sequence without rushing, otherwise the dislodged crystals may simply wander back.
After a successful Epley, many report immediate relief, yet a few may need a repeat session within a few days.
In cases of vestibular neuritis, the lingering imbalance often feels like a constant, low‑grade spinning, not the sudden bursts of BPPV.
Corticosteroids, when started early, can accelerate recovery, but they’re not a magic bullet; vestibular rehab remains essential.
Meniere’s patients, on the other hand, benefit from low‑salt diets and diuretics to manage fluid buildup, though attacks can still strike unpredictably.
For vestibular migraine, the overlap with typical migraine triggers-stress, caffeine, hormonal shifts-means preventive meds plus lifestyle tweaks are indispensable.
Overall, a nuanced understanding of each etiology empowers patients to choose the right strategy rather than resorting to blanket medication.
Sadie Speid
October 20, 2025 AT 19:17
Great summary – balance exercises have truly changed my recovery timeline.
Sue Ross
October 23, 2025 AT 16:44
When you consider the underlying mechanisms described, it becomes clear why targeted rehab is more beneficial than a one‑size‑fits‑all pill regimen.
Rohinii Pradhan
October 26, 2025 AT 13:10
While the overview is generally accurate, it would be prudent to differentiate more precisely between peripheral and central causes, as the therapeutic algorithms diverge significantly.
Anna-Lisa Hagley
October 29, 2025 AT 10:37
The article glosses over the fact that many patients misattribute mild dizziness to vertigo, leading to unnecessary interventions.
A Walton Smith
November 1, 2025 AT 08:04
Fine info but too much fluff.
Theunis Oliphant
November 4, 2025 AT 05:30
One cannot help but observe the superficial treatment of a condition that, in its complexity, demands a more scholarly exposition.
India Digerida Para Occidente
November 7, 2025 AT 02:57
Indeed, the intricacies of vestibular physiology merit a deeper dive than the cursory bullet points provided.
Andrew Stevenson
November 10, 2025 AT 00:24
From a clinical standpoint, incorporating vestibular‑evoked myogenic potentials can refine diagnostic accuracy, especially in ambiguous presentations.
Kate Taylor
November 12, 2025 AT 21:50
Appreciate the practical tips; reminding patients to rise slowly can prevent a cascade of falls.
Hannah Mae
November 15, 2025 AT 19:17
Honestly, the advice feels generic – anyone could've written that.
Iván Cañas
November 18, 2025 AT 16:44
While informal language helps accessibility, a balanced tone would serve both lay readers and clinicians better.
Jen Basay
November 21, 2025 AT 14:10
Good points, especially on when to seek urgent care.
Hannah M
November 24, 2025 AT 11:37
Love the clear steps! 👍🌀
Poorni Joth
November 27, 2025 AT 09:04
People need to stop playing down vertigo as "just dizziness"; it's a serious health signal that deserves respect.
Yareli Gonzalez
November 30, 2025 AT 06:30
Stay consistent with rehab exercises and you’ll notice steady improvement over time.