Statin Muscle Pain: What You Need to Know
When dealing with statin muscle pain, many people wonder if they should quit their cholesterol medication. statin muscle pain, muscle soreness or weakness linked to statin drugs that lower cholesterol. Also known as statin‑induced myopathy, it can range from mild aches to serious muscle damage. The condition encompasses any new muscle discomfort that appears after starting a statin, and it requires careful monitoring of blood work. Relatedly, statins, prescription medicines that reduce LDL cholesterol levels are among the most widely prescribed drugs for heart health. Another key player is muscle pain, a symptom that can signal many conditions, including drug side effects. In rare cases, the pain escalates to rhabdomyolysis, a severe breakdown of muscle tissue that can damage kidneys. Understanding how these entities interact helps you decide whether to adjust dosage, switch drugs, or simply add a vitamin D supplement. Below, we break down the most common triggers, how doctors check for problems, and what you can do at home to stay safe.
Why the Pain Starts and How Doctors Spot It
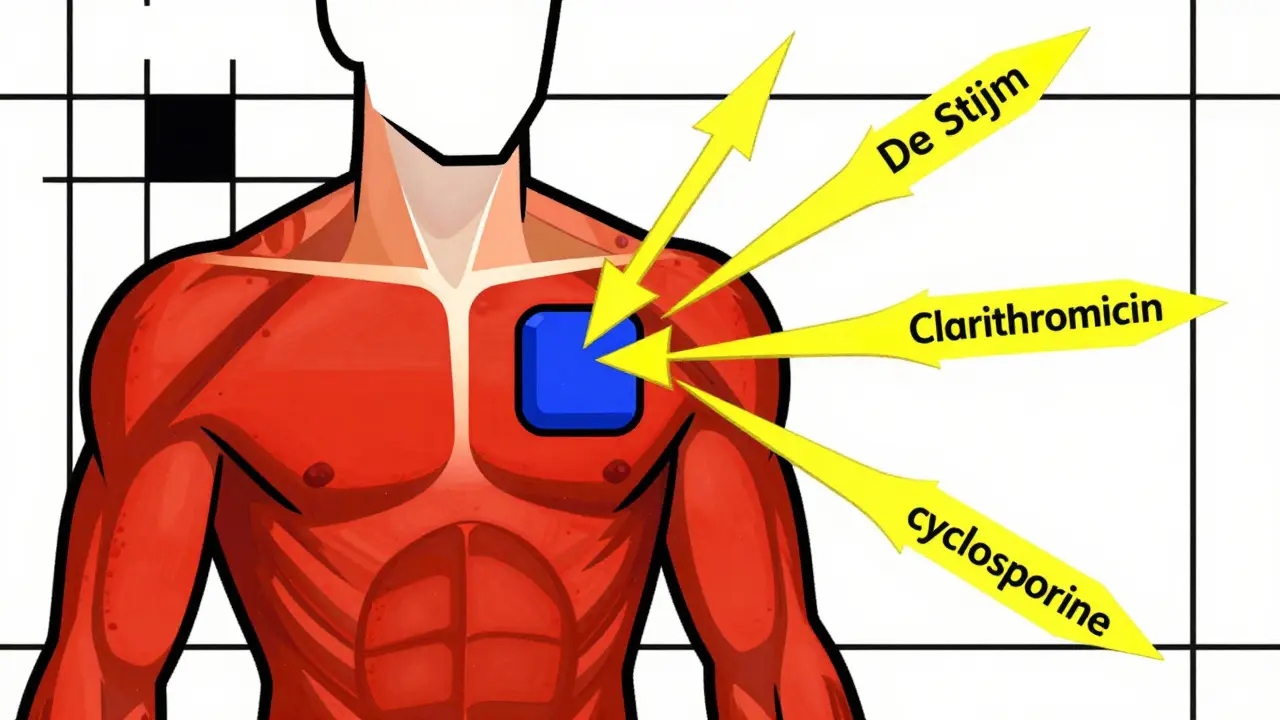
Statins work by blocking an enzyme called HMG‑CoA reductase, which lowers the amount of cholesterol your liver makes. That same pathway also helps produce muscle cell energy, so some people experience a drop in muscle strength. Risk factors include high statin doses, older age, kidney disease, and interactions with medications like fibrates or certain antibiotics. When the muscle fibers are stressed, an enzyme called creatine kinase (CK) leaks into the bloodstream. Doctors usually order a CK test if you report new aches or weakness. A CK level more than ten times the normal range signals possible rhabdomyolysis, while a modest rise may point to milder myopathy. The semantic link here is clear: statin therapy requires CK monitoring, and elevated CK influences the decision to keep or change the drug. If your CK is normal but you still feel sore, your provider might try a lower‑dose statin, switch to a different statin (some are less likely to cause pain), or add a non‑statin cholesterol‑lowering option like ezetimibe.
Beyond labs, paying attention to the pattern of pain is vital. Statin muscle pain usually shows up a few weeks after starting or increasing the dose, and it often affects larger muscle groups like the thighs, calves, or shoulders. The discomfort is often described as a dull ache, heaviness, or a sensation of “tightness.” True rhabdomyolysis, however, brings sharp pain, visible muscle swelling, dark‑colored urine, and fatigue. If any of those red flags appear, seek medical care immediately; untreated rhabdomyolysis can lead to kidney failure. Lifestyle tweaks can also reduce the odds of pain. Staying hydrated, avoiding intense exercise right after a dose, and ensuring adequate intake of vitamin D and magnesium have all been shown to ease muscle symptoms for many patients.
Putting it all together, the collection of articles below gives you a roadmap for handling statin muscle pain without sacrificing heart‑health benefits. You’ll find practical advice on how to talk to your doctor about dosage changes, what lab tests to expect, and natural ways to support muscle health. Whether you’re just starting a statin or have been dealing with aches for months, the insights here aim to help you keep cholesterol under control while minimizing uncomfortable side effects. Dive in to learn the next steps you can take today.
Statins reduce heart disease risk, but certain medications can trigger dangerous muscle damage. Learn which drug combinations raise myopathy risk, who’s most vulnerable, and how to stay safe without giving up statin benefits.
Learn why statins cause muscle aches, who’s at risk, and step‑by‑step ways to diagnose, treat, and prevent pain while staying heart‑healthy.