Statin Muscle Pain Risk Calculator
Your Risk Assessment
This tool helps you understand your risk of statin-associated muscle symptoms based on factors discussed in the article. Remember: this is not a medical diagnosis and should be discussed with your healthcare provider.
Your Risk Assessment Results
Your Risk Score: 0
Personalized Recommendations
What This Means
If you’ve started a cholesterol‑lowering pill and suddenly feel a sore ache in your thighs or shoulders, you’re not alone. statin muscle pain is the most common complaint that pushes patients to question whether they should stay on therapy. This guide walks you through why the pain happens, who’s most at risk, how doctors figure out if the statin is the culprit, and what practical steps you can take without jeopardizing heart health.
What Are Statins and How Do They Work?
Statins are a class of prescription drugs that block an enzyme called HMG‑CoA reductase, the main player in cholesterol production in the liver. By lowering low‑density lipoprotein (LDL) cholesterol, statins cut the risk of heart attacks and strokes by roughly 25‑35% in large clinical trials such as the Heart Protection Study and the JUPITER trial.
Since the FDA approved lovastatin in 1987, more than 32 million Americans fill a statin prescription each year. The benefits are clear, but the side‑effect profile, especially muscle‑related issues, often raises eyebrows.
Understanding Statin‑Associated Muscle Symptoms (SAMS)
Statin‑associated muscle symptoms (SAMS) is an umbrella term that covers four overlapping conditions:
- Myalgia - muscle pain without a rise in creatine kinase (CK).
- Myopathy - muscle weakness with mild CK elevation.
- Myositis - inflammation of muscle tissue, often with higher CK.
- Rhabdomyolysis - severe breakdown of muscle fibers, CK >10× ULN, risk of kidney injury.
In controlled trials, true myopathy or rhabdomyolysis occurs in less than 0.5 per 10,000 patient‑years. Real‑world surveys, however, show that 15‑20 % of patients report some form of myalgia within the first few months of therapy.
How Common Is the Problem?
Discrepancies between trial data and everyday practice are striking. The Mayo Clinic notes an incidence of 5 % or lower when comparing statin‑treated groups to placebo, yet WebMD cites up to 30 % of users complaining of muscle aches. A key driver is the “nocebo effect”: a 2017 Lancet study found that patients warned about muscle pain were 40 % more likely to report it.
Women, older adults, and people with smaller body frames tend to report symptoms more often. For example, Harvard Health reports that women experience myalgias 15‑20 % of the time, compared with roughly half that rate in men.
Who Is Most at Risk?
The following factors raise the odds of muscle discomfort on statins:
- Age ≥ 80 years - risk ↑ 30 %.
- Female gender and body weight < 100 lb - risk ↑ 25 %.
- Pre‑existing muscle disease, hypothyroidism, or liver/kidney impairment - risk ↑ 35‑40 %.
- Concurrent drugs that interfere with statin metabolism (e.g., fibrates, cyclosporine, macrolide antibiotics) - risk ↑ 30‑50 %.
- High‑intensity statin regimens (atorvastatin 40‑80 mg, rosuvastatin 20‑40 mg) - risk ↑ 15 % compared with moderate‑intensity doses.
Knowing these risk factors helps clinicians decide whether a dose reduction or a switch to a lower‑risk statin is appropriate.

How Doctors Diagnose the Source of the Pain
The first step is a thorough clinical interview: ask when the pain started, which muscles are involved, and whether the symptoms are symmetric. Then, a baseline lab test for Creatine Kinase (CK) measures muscle injury. Normal CK varies by lab, but most use an upper limit of around 190 U/L. Values greater than 5× ULN (≈ 950 U/L) suggest a statin‑related problem that warrants temporary discontinuation; >10× ULN signals possible rhabdomyolysis and requires urgent medical care.
If CK is normal, doctors may try a “statin holiday” - stopping the drug for 4‑6 weeks to see if symptoms fade. If they improve, a rechallenge with a lower dose or a different statin can confirm causality.
Management Strategies (Step‑by‑Step)
Below is a practical roadmap you can discuss with your physician:
- Confirm the symptom. Document pain location, intensity (0‑10 scale), and timing.
- Check CK levels. If >5× ULN, stop the statin immediately and hydrate.
- Statin holiday. Take a 4‑6 week break. If pain resolves, you’ve likely identified the drug as the trigger.
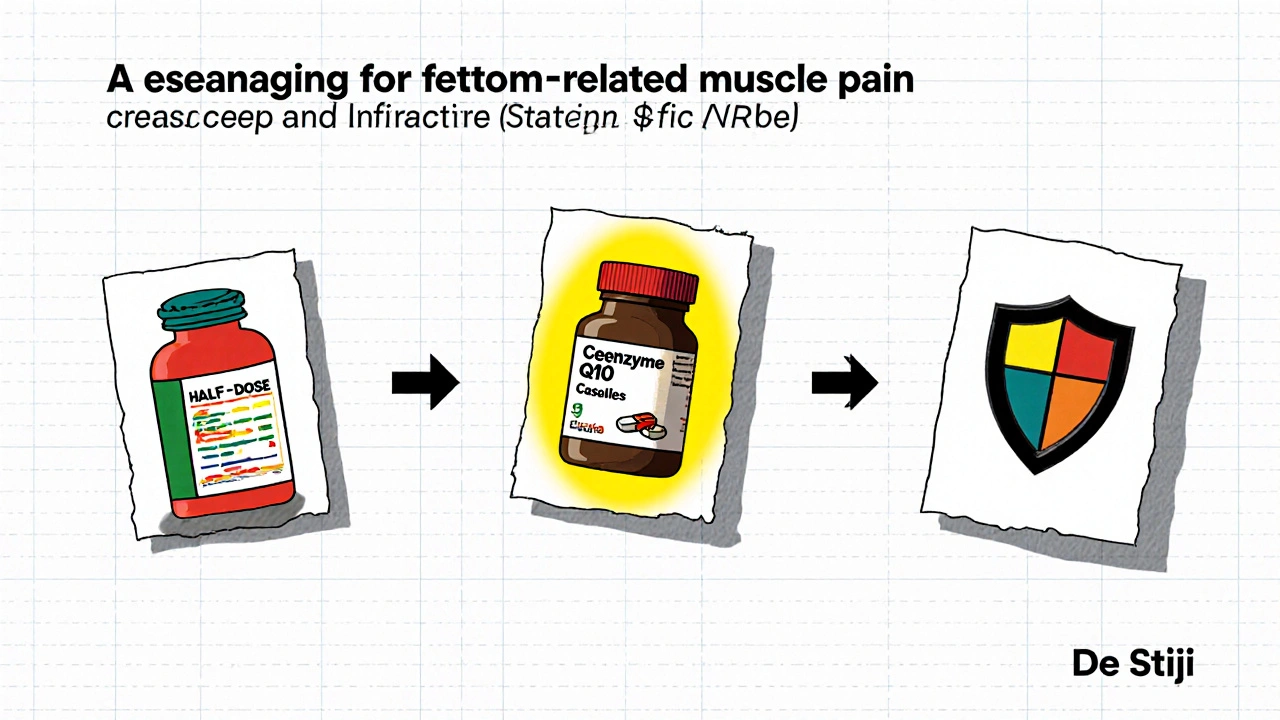
- Rechallenge. Restart at half the original dose or switch to a lower‑risk statin (e.g., pravastatin or fluvastatin). Monitor CK after 2 weeks.
- Consider adjuncts. Some patients feel relief with Coenzyme Q10, a mitochondrial supplement. Evidence is mixed, but a 2018 Atherosclerosis study showed a 30 % symptom reduction in 45 % of participants.
- Non‑statin alternatives. If symptoms persist, options include Ezetimibe (adds ~2 % LDL reduction) or PCSK9 inhibitors like alirocumab and evolocumab (30‑60 % LDL drop). They’re pricey-roughly $5,000 / year versus $4‑30 / month for generic statins.
Never stop a statin without a clinician’s guidance; abrupt discontinuation can raise cardiovascular risk by 25‑50 % within two years.
Comparing Common Statins and Myopathy Risk
| Statin | Usual Dose (mg) | Intensity | Avg. Myopathy Rate* | Typical Cost (generic) |
|---|---|---|---|---|
| Atorvastatin | 10‑80 | High | ~0.6 % | $4‑15 /month |
| Rosuvastatin | 5‑40 | High | ~0.7 % | $5‑20 /month |
| Pravastatin | 10‑40 | Moderate | ~0.2 % | $4‑12 /month |
| Fluvastatin | 20‑80 | Moderate | ~0.15 % | $4‑10 /month |
*Rates come from pooled analysis of the SEARCH and JUPITER trials. Individual risk varies with age, gender, and drug interactions.
When to Seek Immediate Care
If you notice any of the following, call emergency services or visit the ER right away:
- Severe muscle pain that limits walking.
- Dark‑colored urine (possible myoglobinuria).
- CK >10 × ULN or rapid rise on repeat labs.
- Fever, swelling, or weakness that spreads.
These signs point toward rhabdomyolysis, a medical emergency that can cause kidney failure.
Key Takeaways Checklist
- Statins lower LDL and cut heart‑attack risk, but muscle aches are the most reported side effect.
- Real‑world myalgia rates hover around 15‑20 %; severe muscle damage is rare.
- Risk climbs with age, female gender, low body weight, high‑intensity dosing, and interacting meds.
- CK testing, a statin holiday, and a low‑dose rechallenge are the core diagnostic steps.
- If pain persists, consider switching to pravastatin or fluvastatin, trying CoQ10, or moving to non‑statin lipid‑lowering agents.
Frequently Asked Questions
Can I take a lower dose of the same statin and still get heart protection?
Yes. Moderate‑intensity doses still lower LDL by 30‑50 % and preserve most of the cardiovascular benefit while reducing muscle‑pain risk for many patients.
Is Coenzyme Q10 worth trying?
The evidence is mixed. Some small trials show modest symptom relief, but large meta‑analyses find no statistically significant benefit. It may be tried on a case‑by‑case basis.
What’s the difference between myalgia and myopathy?
Myalgia is pain without a rise in CK. Myopathy includes muscle weakness with a mild CK elevation, indicating actual muscle damage.
Should I stop my statin if I feel sore after a workout?
Not automatically. Exercise‑related soreness is common and usually unrelated to the drug. Track the pattern: if pain appears every day, in the same muscles, and persists beyond a few days, bring it to your doctor’s attention.
When is rhabdomyolysis a real concern?
Rhabdomyolysis is rare (0.1‑0.5 per 10 000 patient‑years) but serious. Look for severe pain, dark urine, and CK >10 × ULN. Prompt medical evaluation is essential.
Statin‑related muscle pain can feel discouraging, but with a systematic approach you can often stay on therapy and keep your heart protected. Talk openly with your clinician, follow the stepwise plan above, and remember that most patients find a regimen that works without persistent aches.

Comments (10)
Abhinav B.
October 24, 2025 AT 19:50
Listen, statins are not a curse – the muscle aches you feel are real but they rarely signal life‑threatening damage. If you’re over 80 or on a high‑intensity dose, cut bak and see if the pain eases. Talk to your doc, don’t just quit cold turkey.
Lisa Woodcock
November 7, 2025 AT 01:23
It can be scary when your thighs start hurting after you begin a new med, but remember that the cardiovascular benefit is huge. Many patients find a lower‑dose or a different statin works just fine, and adding a short statin holiday can clarify if the drug is the cause.
Veronica Appleton
November 20, 2025 AT 07:56
Statin‑related myalgia is common you don’t need to panic it’s usually mild the first step is to document when the pain started and how intense it feels on a 0‑10 scale then get a baseline CK test if CK is normal a short break from the drug for 4‑6 weeks can help you see if the pain improves after stopping if it does you can try a lower dose or switch to pravastatin which has a lower reported myopathy rate
ram kumar
December 3, 2025 AT 14:29
Ah, the tragic chorus of modern medicine – a pill that promises to save your heart yet steals your comfort. The chorus of “muscle pain” echoes through forums, yet the evidence shows true rhabdomyolysis is rarer than a blue moon. Still, the no‑cebo effect looms like a phantom, convincing the vulnerable that every ache is doom. We must not surrender to anecdote alone; clinicians should wield the statin holiday as a scalpel, not a blunt hammer.
Deborah Galloway
December 16, 2025 AT 21:01
Hey there, I totally get how disheartening those lingering aches can feel. It helps to keep a simple journal – note the day you started the statin, the exact spot of pain, and a quick 1‑10 rating. Share that with your doctor, and together you can decide whether a dose tweak or a switch to a gentler statin is best.
Charlie Stillwell
December 30, 2025 AT 03:34
🚨Listen up! The pharmacokinetic interplay between statins and CYP3A4 inhibitors can precipitate iatrogenic myopathy – a textbook case of drug‑drug synergy gone awry. If you’re co‑prescribed a macrolide, you’re flirting with CK spikes 🚑. Trim the dose, monitor labs, or pivot to a statin with minimal hepatic metabolism. No more guesswork.
krishna chegireddy
January 12, 2026 AT 10:07
They want you to believe it’s just a side effect but the real agenda is control – big pharma pushes high‑intensity doses to keep profits up and the truth about muscle toxicity hidden. Switch to a cheap, low‑risk statin or even diet‑only if you can; don’t be a pawn.
Tamara Schäfer
January 25, 2026 AT 16:39
It's easy to feel trapped when a medication meant to protect your heart starts to feel like a foe. Yet, the body is a resilient system that often adapts when given the right guidance. First, consider keeping a simple diary of your daily activities, noting the exact time you take the statin and any subsequent muscle sensations. This log becomes a concrete piece of evidence you can share with your clinician. When you notice a pattern, such as pain appearing two days after a dose increase, you have a clear data point. A statin holiday, typically four to six weeks, is a scientifically supported method to see if symptoms abate. If the aches fade, you’ve essentially performed a natural experiment confirming causality. Reintroducing the drug at half the previous dose, or switching to prvastatin, often restores the balance between lipid lowering and comfort. Some patients also report modest relief with coenzyme Q10, though the literature is mixed, so it’s worth a cautious trial. Remember, severe outcomes like rhabdomyolysis are rare, and the benefits of LDL reduction remain substantial. However, never ignore dark urine or a rapid rise in CK; these are red flags demanding immediate medical attention. It’s also wise to review any concurrent medications, as many common drugs can boost statin levels unintentionally. Simple lifestyle tweaks – regular moderate exercise, balanced diet, and adequate hydration – can further support muscle health. Ultimately, the goal is not to abandon treatment but to fine‑tune it so that you protect your heart without sacrificing quality of life. Keep an open dialogue with your healthcare team, ask questions, and advocate for a regimen that feels right for you. With patience and partnership, you can navigate this challenge and emerge stronger.
Tamara Tioran-Harrison
February 7, 2026 AT 23:12
Indeed, the exhaustive treatise above could have been condensed into a single sentence: “Talk to your doctor.” Yet, the flourish is appreciated, if not a tad pretentious. :)
Jonah O
February 21, 2026 AT 05:45
One might wonder why the “talk to your doctor” mantra is so ubiquitously pushed – perhaps it’s a subtle mechanism to keep patients compliant while the underlying pharmacological risks stay buried beneath layers of jargon. The truth is hidden, and only the skeptical see through.