Pharmaceutical Manufacturing: How Drugs Are Made and Why It Matters
When you pick up a pill at the pharmacy, you’re holding the result of pharmaceutical manufacturing, the complex process of designing, testing, and producing medicines at scale. Also known as drug production, it’s not just mixing chemicals—it’s a tightly controlled system that decides whether a drug is safe, effective, and affordable. Every tablet, injection, or cream you use started in a lab, went through strict quality checks, and was built to meet rules set by agencies like the FDA. This isn’t magic. It’s science, engineering, and regulation working together—often under pressure to deliver more drugs faster and cheaper.
Behind every generic drug, a lower-cost version of a brand-name medicine that works the same way. Also known as bioequivalent medication, it is a direct product of pharmaceutical manufacturing. Companies don’t just copy the brand—they prove their version behaves identically in the body. That’s why the FDA Orange Book, the official database that lists approved drugs and their therapeutic equivalence ratings matters so much. If a generic isn’t listed there with an AB rating, it might not work the same. And if the manufacturing facility doesn’t follow Good Manufacturing Practices (GMP), even a perfectly formulated drug could be contaminated, weak, or dangerous. The same rules apply to brand-name pills too. A single batch of faulty manufacturing can lead to recalls, hospitalizations, or worse.
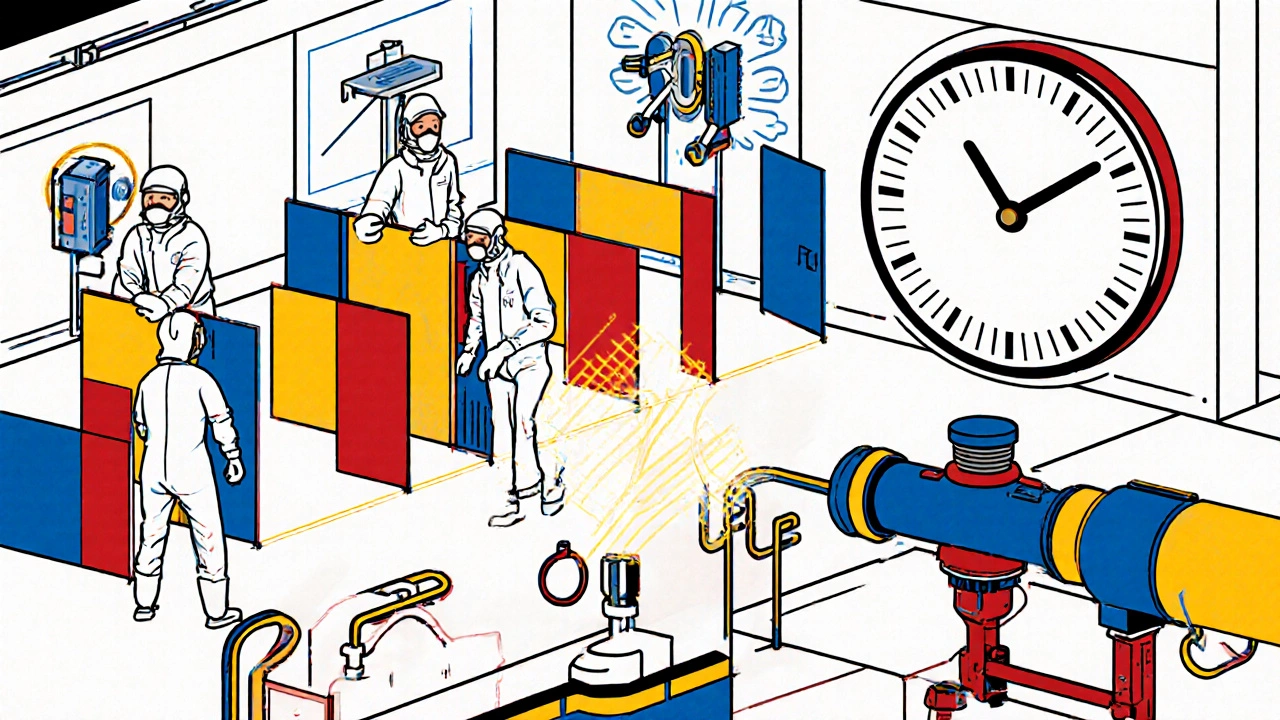
It’s not just about making pills. It’s about making them right—every time. That’s why the process includes testing for purity, stability, and how the drug breaks down in your body. It’s why some drugs cost more, not because they’re better, but because their manufacturing is harder—like biologics made from living cells, or drugs that need ultra-cold storage. Even something as simple as a nasal spray or topical cream has to be produced in clean rooms with exact measurements. And when you see a coupon for a generic, or hear about a drug shortage, it’s often because of a hiccup in this system: a factory shut down, a raw material delay, or a quality failure.
What you’ll find in the posts below are real examples of how this system affects you. From how to check if your generic is truly equivalent, to why some drugs interact dangerously with others because of how they’re processed in the body, to how cost-cutting in manufacturing can lead to risky substitutions. These aren’t abstract theories. They’re the hidden rules behind every prescription you fill. You don’t need to run a factory to understand what’s in your medicine—but knowing how it got there helps you ask the right questions, spot red flags, and make smarter choices about your health.
Understand the latest GMP standards for pharmaceutical and medical device manufacturing in 2025. Learn FDA and EU requirements, key compliance areas, costs, and real-world challenges.