When you take a pill, inject a vaccine, or use a medical device, you expect it to be safe, effective, and exactly as labeled. That’s not luck. It’s the result of Current Good Manufacturing Practice (GMP) standards - strict rules that keep medicines and medical products from being contaminated, mislabeled, or ineffective. These aren’t suggestions. They’re legally enforceable requirements that manufacturers must follow, or face shutdowns, recalls, and fines.
What Exactly Are GMP Standards?
GMP stands for Good Manufacturing Practice. The "Current" part - often written as CGMP - is critical. It means manufacturers must use modern tools, systems, and methods. It’s not enough to have clean floors and trained staff. You need real-time monitoring, validated processes, and digital records that can’t be altered after the fact.
The U.S. Food and Drug Administration (FDA) first codified CGMP rules in 1978 under 21 C.F.R. Parts 210 and 211. Since then, they’ve been updated constantly. In 2025, the FDA issued new guidance that explicitly says: "Don’t rely on old sampling methods if you can test in real time." That’s a major shift. Instead of pulling vials off the line for lab testing, companies are now encouraged to use sensors that monitor product quality as it’s made - on-line, at-line, or in-line.
The European Medicines Agency (EMA) has its own version, called EU GMP, with Annex 1 - the rulebook for sterile products - fully in effect as of August 25, 2024. And the World Health Organization (WHO) sets baseline standards used by over 100 countries, especially in developing regions where local regulations are still catching up.
The Nine Core Requirements of GMP in 2025
There’s no single checklist, but every major regulator agrees on these nine pillars. Skip one, and your entire batch could be rejected.
- Quality Management - This isn’t just a department. It’s a culture. Every decision, from hiring to equipment cleaning, must be tied to quality. The quality unit must have final say on batch release - no exceptions.
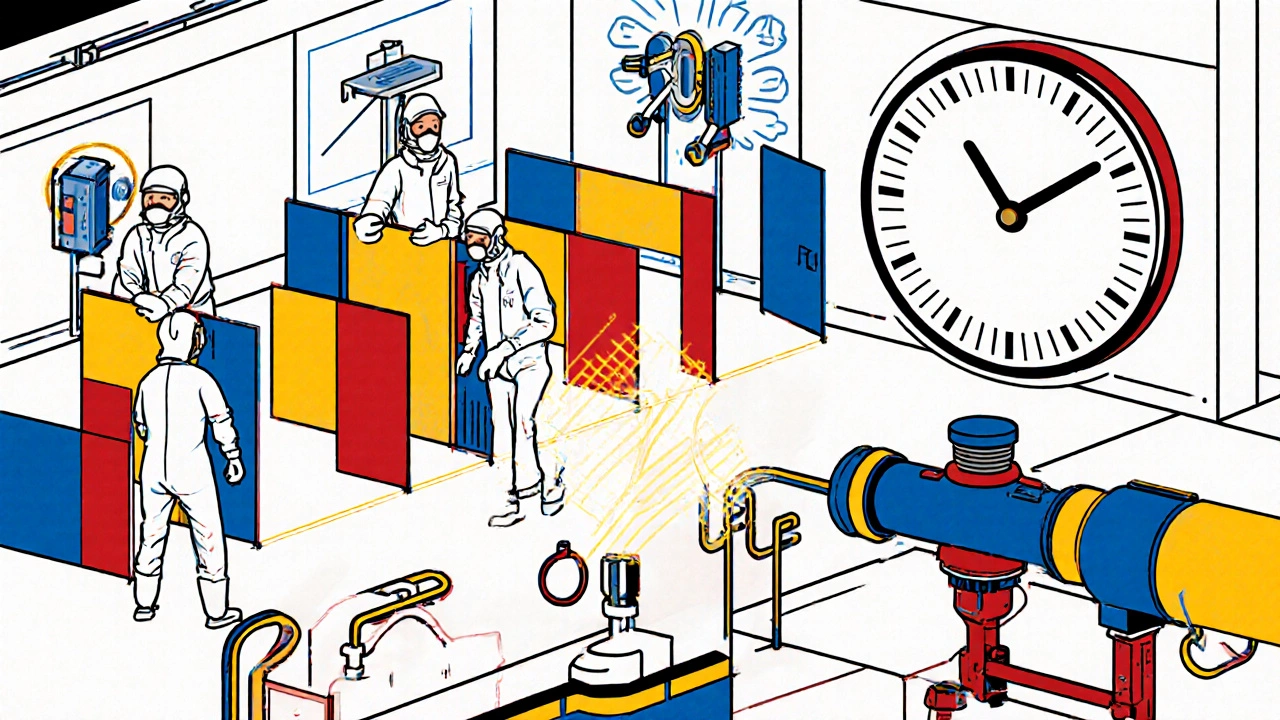
- Sanitation and Hygiene - Clean rooms aren’t optional. For sterile products, you need ISO 14644-1 Class 5 air quality. That’s 100 particles per cubic meter or fewer. Cleaning procedures must be validated, not just written. And personnel gowning? In EU GMP, you now need full-body, sterility-assured suits in Grade A/B zones. No exposed skin.
- Building and Facilities - Layout matters. Production, packaging, and storage areas must be physically separated to prevent cross-contamination. HVAC systems must be monitored 24/7. Temperature and humidity logs? They’re not paperwork - they’re evidence.
- Equipment - Every machine must go through IQ (Installation Qualification), OQ (Operational Qualification), and PQ (Performance Qualification). If you replace a pump, you don’t just install it. You prove it works under real conditions. The FDA requires this under § 211.67. No shortcuts.
- Raw Materials - Every ingredient must be tested for identity, purity, and potency before it touches your product. Storage conditions? Documented. Temperature logs? Kept. Expired materials? Immediately quarantined and destroyed with records.
- Personnel - Training isn’t a one-time event. Staff must be trained quarterly, with competency assessments. If someone handles sterile products, they need retraining every six months. The FDA saw 61% of its 2024 Warning Letters cite poor training or cultural resistance to documentation.
- Validation and Qualification - You can’t just say "it works." You must prove it works, every time, under normal conditions. Process validation is mandatory. And if you use AI or machine learning for quality prediction? You need extra documentation under § 211.100(b). The FDA doesn’t trust black-box algorithms.
- Complaints and Recalls - If a customer reports a problem, you have 72 hours to start an investigation. Root cause analysis must be completed within 30 days. Recalls must be swift and traceable. In 2024, 18% of recalls were tied to poor supply chain oversight - something EMA now requires you to audit proactively.
- Documentation and Record Keeping - This is the backbone. Every action, every test, every change must be recorded contemporaneously. Electronic records must follow ALCOA+: Attributable, Legible, Contemporaneous, Original, Accurate, and + Complete, Consistent, Enduring, Available. If you can’t prove it happened, it didn’t.
FDA vs. EU GMP: Key Differences in 2025
Not all GMP rules are the same. The FDA and EMA have different styles - and that’s a headache for global manufacturers.
| Requirement | FDA CGMP | EU GMP (Annex 1) |
|---|---|---|
| Testing Approach | Allows in-line, at-line, or on-line measurements. No physical sampling required if validated. | Still requires physical sampling for critical quality attributes. In-line tools are supplementary. |
| Personnel Gowning | Requires cleanroom suits, but no explicit full-body sterility mandate. | Full-body, sterility-assured garments required in Grade A/B zones. |
| Data Integrity | Strict ALCOA+ enforcement. Audit trails mandatory for all electronic records. | Requires audit trails per Annex 11. Penalties for missing trails are severe. |
| Flexibility | High. Manufacturers can design their own systems if scientifically justified. | Low. More prescriptive. Exact methods often specified. |
| Enforcement | 2,147 Warning Letters issued in FY2024 - mostly for data integrity issues. | Fewer warnings, but more shutdowns and fines for serious breaches. |
One Pfizer supervisor told the GMP Professionals LinkedIn group: "We run duplicate environmental tests because FDA and EMA want different parameters. It costs us $75,000 a year per facility." That’s the hidden cost of regulatory fragmentation.
What’s Changing in 2025?
Three big trends are reshaping GMP compliance right now.
- Data Integrity Is the #1 Priority - 68% of facilities surveyed in December 2024 said this was their biggest challenge. The FDA is cracking down on backdated entries, shared login credentials, and deleted audit trails. Systems must be validated to prevent tampering.
- Advanced Manufacturing Is Here - Continuous manufacturing is up 37% since 2023. AI-driven quality prediction tools are up 52%. But the FDA warns: don’t use AI alone. Pair it with real-time testing. Merck’s Whitehouse Station facility got zero FDA 483s after implementing Process Analytical Technology (PAT) - but it took two years and $2 million.
- Supply Chain Oversight Is Tightening - EMA now requires serialization for all prescription drugs. The FDA mandates risk-based supplier audits. If your active ingredient comes from a factory in India or China, you must inspect it. In 2024, 27% of recalls came from supplier failures.
And don’t forget: pandemic flexibilities ended January 1, 2025. GMP certificates are no longer extended. Inspections are back to full force.
Implementation Costs and Real-World Challenges
Compliance isn’t cheap. A mid-sized pharmaceutical company spends an average of $1.2 million to get fully compliant. That includes:
- Upgrading equipment for in-line monitoring ($250,000 per production line, according to a Reddit user)
- Building a dedicated compliance team (minimum 3 full-time roles for facilities over 10,000 sq ft)
- Writing 120-150 Standard Operating Procedures (SOPs)
- Training staff 40+ hours per year
- Investing in validated electronic systems
Legacy equipment is the biggest blocker. 73% of facilities say integrating old machines with modern sensors is nearly impossible without full replacement. Cultural resistance is another. People hate documentation. But the FDA found that 61% of their 2024 Warning Letters cited "lack of documentation culture" as a root cause.
And in emerging markets? WHO’s October 2024 report found that only 43% of facilities meet even basic GMP standards. That’s why contaminated medicines still reach patients in low-income countries.
Why This Matters to You
Whether you’re a patient, a pharmacist, or a regulator - GMP is the invisible shield between you and dangerous products. A single failure can lead to death. In 2023, contaminated heparin killed over 80 people in the U.S. alone. That’s why these rules exist.
Manufacturers who embrace GMP don’t just avoid fines. They build trust. Merck, Pfizer, and Johnson & Johnson don’t spend millions on compliance because they have to. They do it because they know it’s the only way to make medicines people can rely on.
And if you’re in the industry? The message is clear: modernize or get left behind. The FDA isn’t asking for more paperwork. It’s asking for smarter, faster, more reliable systems. The future of manufacturing isn’t manual sampling. It’s real-time data. It’s predictive analytics. It’s systems that don’t just meet standards - they anticipate failure before it happens.
What happens if a company doesn’t follow GMP standards?
If a company violates GMP, the FDA or EMA can issue a Warning Letter, seize products, block imports, or shut down operations. In severe cases, executives can face criminal charges. Products may be recalled, leading to massive financial losses and reputational damage. In 2024, the FDA issued 2,147 Warning Letters - most for data integrity or documentation failures.
Is GMP only for pharmaceuticals?
No. GMP applies to pharmaceuticals, medical devices, food products, and dietary supplements. While the exact rules vary by product type, the core principles - control, documentation, validation, and quality - are the same. The FDA’s 21 C.F.R. Part 111 covers dietary supplements, and Part 117 covers food manufacturing.
Can small companies afford GMP compliance?
Yes, but it’s challenging. Small companies often outsource testing or use contract manufacturing organizations (CMOs) that are already compliant. The FDA offers guidance for small businesses and may provide flexibility during inspections if the company demonstrates a good-faith effort. However, there are no exemptions. If you sell a product in the U.S., you must meet CGMP.
How often are GMP inspections conducted?
The FDA inspects high-risk facilities every 2-3 years. Lower-risk sites may be inspected every 4-5 years. However, inspections can happen anytime - especially after a complaint, recall, or whistleblower report. The EMA conducts routine inspections too, often in partnership with national agencies. Post-pandemic, inspections are back to pre-2020 frequency.
What’s the difference between GMP and ISO 9001?
ISO 9001 is a general quality management standard for any industry. GMP is specific to regulated products like drugs and medical devices. GMP includes mandatory testing, validation, and documentation requirements that ISO 9001 doesn’t cover. A company can be ISO 9001 certified and still fail a GMP inspection. GMP is legally binding; ISO is voluntary.
Are AI and automation allowed under GMP?
Yes - but with strict conditions. The FDA supports AI for real-time quality monitoring, but it must be validated. You can’t use an AI model without proving it works under all expected conditions. You need documentation showing how it was trained, what data it uses, and how errors are caught. The FDA explicitly warns against using AI alone - it must be paired with in-process testing.
How long do GMP records need to be kept?
Typically, records must be kept for at least one year after the product’s expiration date. For some products, like vaccines, the requirement is longer - up to five years. Electronic records must be preserved in a way that prevents deletion or alteration. The FDA requires that records remain accessible and readable throughout their retention period.
If you’re in manufacturing, the time to act is now. GMP isn’t about checking boxes. It’s about building systems that protect lives. The rules are clear. The technology exists. The question is: are you ready to meet them?
Comments (16)
Jamie Watts
November 16, 2025 AT 11:33
Let me tell you something - GMP isn’t just paperwork, it’s survival. I’ve seen factories shut down because someone thought ‘close enough’ was good enough. That’s not negligence, that’s negligence with a paycheck. The FDA doesn’t play. They come in with laptops, audit trails, and a death wish for anyone who backdates a log. If your SOPs are outdated, you’re already dead. Just ask Pfizer.
Real-time monitoring? Yeah, it’s expensive. But so is a recall that kills 80 people. And no, you can’t just ‘update it later.’ The system doesn’t care if you were busy. It records. It logs. It remembers. And it doesn’t forgive.
John Mwalwala
November 16, 2025 AT 20:39
Have you ever wondered why the FDA is pushing AI so hard? It’s not about efficiency - it’s about control. They want to know every single variable in your process, down to the humidity in the glovebox. And they want it all stored in a system they can access remotely. Who owns that data? Who’s behind the firewall? Who’s watching your sensors? It’s not just GMP anymore - it’s surveillance capitalism wrapped in a lab coat.
And don’t get me started on ‘validated algorithms.’ What’s validated? Who validated it? Did they test it against a placebo? Or did they just run it on data they cooked themselves? I’ve seen AI models trained on 3 months of data and then deployed for 5 years. That’s not innovation. That’s a time bomb with a compliance sticker.
Deepak Mishra
November 18, 2025 AT 07:00
OMG I JUST READ THIS AND I AM SHAKING 😭😭😭
So like… if your guy in the cleanroom forgets to wipe his nose before putting on the suit… does that mean EVERYTHING IS CONTAMINATED??? 😱 And what if the sensor breaks but no one notices for 3 hours?? 😭😭😭
And the part about $75k/year just to satisfy both FDA and EMA?? I mean… who even made this system?? Some robot from Mars?? I’m not even mad… I’m just impressed… and terrified… and also crying a little 😭😭😭
Rachel Wusowicz
November 19, 2025 AT 20:36
It’s not just about compliance - it’s about control. Who benefits from making GMP so complex? Who profits from the $1.2 million price tag? Big Pharma? The consultants? The software vendors selling ‘validated’ systems that take 18 months to implement? Or… the regulators themselves? Because if every small company is forced to outsource to a CMO, then the market becomes a monopoly of the few who can afford it.
And then they say ‘innovation’ - but innovation dies when you can’t afford to try. They call it ‘safety.’ I call it gatekeeping. And the worst part? The people who need these medicines the most - the ones in Nigeria, India, Bangladesh - they’re getting the leftovers. The ones the big labs rejected because the sensors didn’t like the humidity.
It’s not about quality. It’s about power.
Dan Angles
November 21, 2025 AT 11:51
The structural integrity of pharmaceutical manufacturing is predicated upon the rigorous adherence to standardized operational protocols that ensure patient safety and product integrity. The regulatory frameworks established by the FDA and EMA are not arbitrary; they are the culmination of decades of empirical evidence, incident analysis, and systemic failure mitigation.
It is imperative that stakeholders recognize that compliance is not a cost center, but a risk mitigation strategy of the highest order. The absence of documentation, the failure to validate, or the circumvention of quality unit authority constitutes not merely procedural negligence, but an ethical breach of the social contract between manufacturer and public.
Organizations that treat GMP as a checklist are not merely non-compliant - they are endangering lives. The data is unequivocal. The consequences are irreversible.
David Rooksby
November 21, 2025 AT 22:21
Look, I’ve worked in a factory where the guy who cleaned the vials used the same rag for everything. No joke. And yeah, they got shut down. But here’s the thing - the FDA doesn’t care if you’re a small shop with three employees and a fridge full of vials. They treat you like Pfizer. And that’s the problem. You can’t just slap on a cleanroom suit and call it a day. You need a whole team, a whole system, a whole IT department to keep the audit trails from crashing.
And don’t even get me started on the ‘ALCOA+’ nonsense. It’s like they invented a new language just to make sure only consultants can understand it. Attributable? Legible? Enduring? What does that even mean? I once saw a guy write ‘10/12/24’ on a logbook and they gave him a 483. Why? Because the system wanted ‘YYYY-MM-DD’. No one else in the world writes like that. But yeah, that’s the rule now. So we all just… do it. Because if you don’t, you’re done.
And the worst part? The people who actually make the stuff? They’re the ones getting yelled at. The managers? They’re on vacation in Bali. The regulators? They’re writing another 20-page guidance doc. And the patients? They’re just hoping the pill doesn’t kill them.
Melanie Taylor
November 23, 2025 AT 15:02
Okay but can we talk about how wild it is that we’re using AI to predict if a pill is safe… and yet we still have people writing logs with pens?? 😅
I mean… the sensors are real-time, the algorithms are learning, the machines are talking to each other… but the guy in QA still has to sign a paper? Like… why??
Also… why is the EU so rigid?? Like… I get it, you want sterility… but why can’t we just… merge the standards?? 😭 Why are we spending $75k/year to do the same thing twice??
Also… WHO says only 43% of facilities in developing countries meet basic GMP? That’s… not a number. That’s a tragedy. And we’re still talking about audit trails. 💔
Teresa Smith
November 24, 2025 AT 14:51
This isn’t about rules. It’s about responsibility. Every time a batch is released without proper validation, someone’s life is on the line. Not a statistic. Not a line item. A person. A mother. A child. A grandparent.
And yes, it’s expensive. Yes, it’s complicated. Yes, it’s frustrating. But if you’re in this industry and you’re complaining about the paperwork, you’re in the wrong field.
Medicine isn’t software. You can’t just push a patch. You can’t roll back a bad update. Once it’s in the body, it’s too late. So we don’t cut corners. We don’t take shortcuts. We don’t say ‘it’s good enough.’
If you can’t handle that, then get out. Because the people who need this medicine? They don’t have the luxury of compromise.
ZAK SCHADER
November 25, 2025 AT 05:41
USA rules. FDA knows best. Why are we even listening to the EU? They’re still using paper logs and manual sampling like it’s 1998. We’ve got AI, real-time sensors, and blockchain-ready systems - and they’re still asking for vial samples? Pathetic.
And don’t get me started on India. 43% compliance? That’s why their meds are killing people. We don’t need WHO telling us what to do. We’ve got the best tech, the best science, the best standards. The rest of the world should just adopt ours and shut up.
Also, why do we pay for all this? China’s got cheaper factories. Why don’t we just outsource and call it a day? Wait… oh right. Because we’re not stupid. Unlike them.
Danish dan iwan Adventure
November 26, 2025 AT 19:44
Validation is king. No validation = no batch. No audit trail = no sale. No training = no license. Simple. No drama. If you can’t do it, don’t do it. The market doesn’t care about your excuses.
Ankit Right-hand for this but 2 qty HK 21
November 28, 2025 AT 10:50
Oh so now we’re supposed to believe the FDA and EMA are saints? Please. They’re bureaucrats. They’re scared of change. They’re scared of innovation. They’re scared of being replaced by AI. So they make rules that are impossible to follow - just to keep the consultants rich.
And don’t even mention India. You think we don’t know how many fake drugs are sold in the U.S.? You think the FDA checks every shipment from China? They don’t. They check the ones that get leaked by whistleblowers. That’s not regulation. That’s damage control.
And you want me to spend $1.2 million to follow a rulebook written by people who’ve never touched a machine? I’ll take my chances with the Indian factory. At least they’re honest about it.
Oyejobi Olufemi
November 29, 2025 AT 05:55
Do you know what GMP really is? It’s the last stand of human dignity against the machine. Every log, every signature, every sensor reading - it’s a whisper against the void. The machine wants to automate everything. It wants to erase the human hand. But we are not data points. We are not algorithms. We are the ones who feel the weight of responsibility.
And yet… they want us to trust AI to predict failure? What if the AI is wrong? What if it learns from corrupted data? What if it’s trained on data from a factory that was already failing? Who holds it accountable? Who signs the death warrant?
They say ‘modernize or die.’ But modernization without humanity is not progress. It is annihilation dressed in a lab coat.
Daniel Stewart
December 1, 2025 AT 00:59
There’s a quiet irony here. We’ve built systems that are meant to prevent death - yet they demand such perfection that they become instruments of fear. The fear of failure. The fear of being caught. The fear of being replaced. The fear of being blamed.
And in that fear, we’ve lost something essential: trust. Trust in the system. Trust in the people. Trust in the process.
Perhaps the real failure isn’t in the audit trail. It’s in the silence that follows when someone asks, ‘Why are we doing this?’ and no one answers except with another rule.
Latrisha M.
December 2, 2025 AT 07:26
Compliance is hard. But it’s necessary. Every SOP, every log, every validation - it’s not about bureaucracy. It’s about someone’s child getting the right dose. Someone’s parent not getting poisoned. Someone’s life not ending because a sensor failed and no one checked.
Don’t make it harder than it is. Don’t romanticize it. Don’t hate it. Just do it. Well. Consistently. Accurately.
That’s all.
Diane Tomaszewski
December 2, 2025 AT 23:10
I used to think GMP was just rules. Now I see it as care. Not the kind you show with flowers. The kind you show by writing down what you did. By double-checking. By not cutting corners because you’re tired. By caring enough to log it, even when no one’s watching.
It’s not sexy. But it saves lives.
Jamie Watts
December 4, 2025 AT 12:18
And now they’re adding AI to the mix? Great. So now we’ve got a machine writing logs for a machine that’s monitoring a machine. And if the AI says the batch is good, but the human says it looks weird - who wins? The machine? Because it’s ‘validated’?
Good luck explaining that to a jury when someone dies.