Optic Neuritis: What It Is, Why It Matters, and How to Manage It
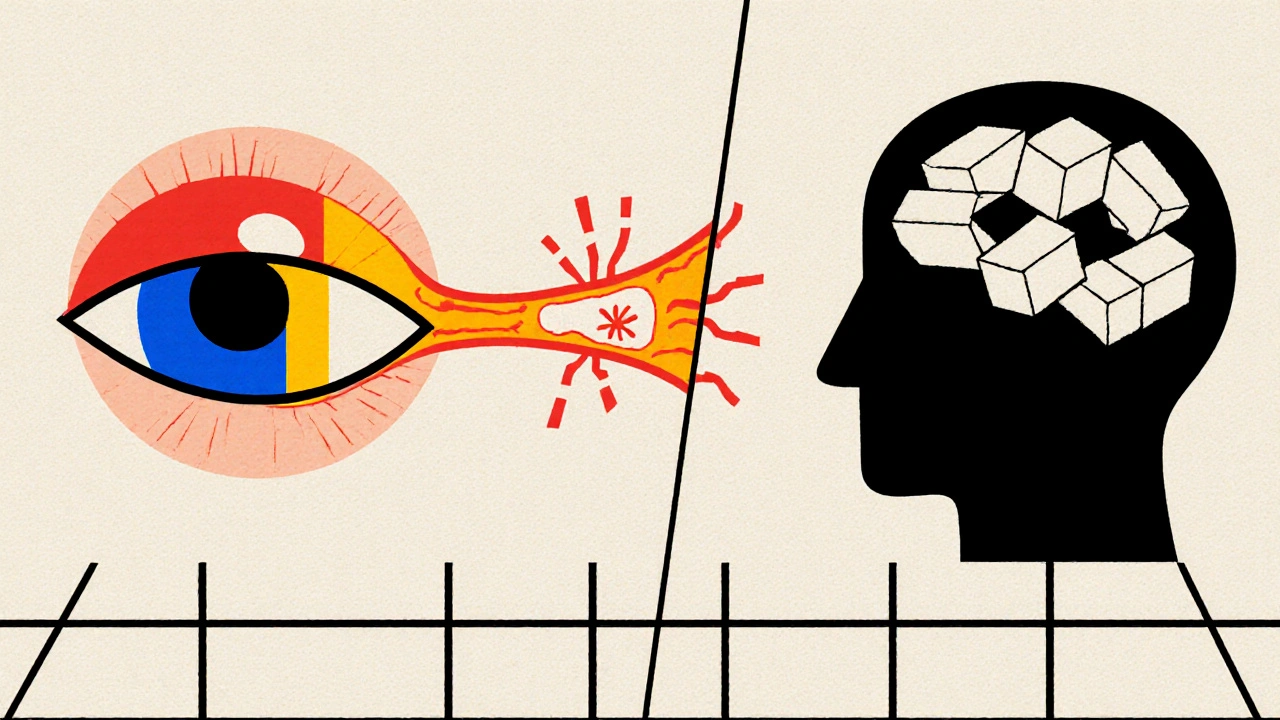
When dealing with optic neuritis, a sudden inflammation of the optic nerve that often brings rapid vision loss and eye pain. Also known as optic nerve inflammation, it can be the first sign of a broader autoimmune problem. One of the most common connections is with multiple sclerosis, a disease where the immune system attacks the nervous system. If you’ve never heard of it, think of it as a condition that can turn blurry vision into a warning light for doctors to investigate further. optic neuritis doesn’t stay hidden for long, and catching it early makes a big difference in outcomes.
How Doctors Pinpoint the Problem
Diagnosis leans on two main tools. First, a MRI, magnetic resonance imaging that shows inflammation around the optic nerve and any brain lesions gives a clear picture of what’s happening inside. Doctors also run visual evoked potentials, tests that measure the brain’s electrical response to visual stimuli. Together, these tests tell you whether the nerve is inflamed, if there are hidden plaques typical of multiple sclerosis, and how severe the damage might be. The results guide the next steps and help reassure patients about the prognosis.
Beyond imaging, a quick eye exam checks color vision, visual acuity, and pupil reactions. Blood work may rule out infections or other inflammatory causes, but the MRI and visual evoked potentials remain the gold standard for confirming optic neuritis and spotting any associated central nervous system issues.
When the diagnosis clicks, treatment moves fast. The go‑to therapy is a short course of corticosteroids, powerful anti‑inflammatory drugs that reduce swelling of the optic nerve. Oral prednisone or an IV methylprednisolone drip can speed up visual recovery, especially if started within two weeks of symptom onset. While steroids don’t change the long‑term outlook for most patients, they can cut the recovery time from weeks to days, making daily life less disruptive.
Not everyone needs steroids. Some people recover fully without medication, and doctors weigh the benefits against possible side effects like blood sugar spikes or mood changes. For those with recurring episodes or a confirmed multiple sclerosis diagnosis, disease‑modifying therapies may be added later to keep the immune system in check and protect future nerve health.
Living with optic neuritis also means practical steps at home. Reducing screen time, using good lighting, and wearing sunglasses outdoors can ease discomfort. If vision is blurry, a temporary magnifier or larger print can help keep work or school tasks manageable. Most patients see significant improvement within a month, but a follow‑up eye exam is essential to ensure the nerve has healed properly.
If you’re reading this because you or a loved one just got the diagnosis, know that the medical community has a clear roadmap. From the quick MRI scan to the targeted steroid regimen, each step aims to restore sight and limit any further nerve damage. Below you’ll find a curated set of articles that dive deeper into each of these areas—whether you want to understand the science behind MRI findings, learn how steroids work, or explore lifestyle tips while your eyes heal. Browse the collection to get practical advice and the latest research, all geared toward helping you navigate optic neuritis with confidence.
Learn how multiple sclerosis impacts eyesight, common visual symptoms, diagnosis tools, and effective treatments to protect your vision.