Obesity Pathophysiology: How Fat Changes Your Body and What You Can Do
When we talk about obesity pathophysiology, the biological process by which excess body fat leads to disease. It's not just about eating too much or moving too little—it's about how fat tissue becomes a dysfunctional organ that sends harmful signals through your body. This isn't a simple energy balance problem. Fat isn't passive. Once it builds up, especially around your belly, it starts releasing inflammatory chemicals, disrupting hormones, and confusing your brain's hunger signals. The result? Your body starts resisting insulin, your liver gets fatty, and your blood pressure climbs—all before you even feel sick.
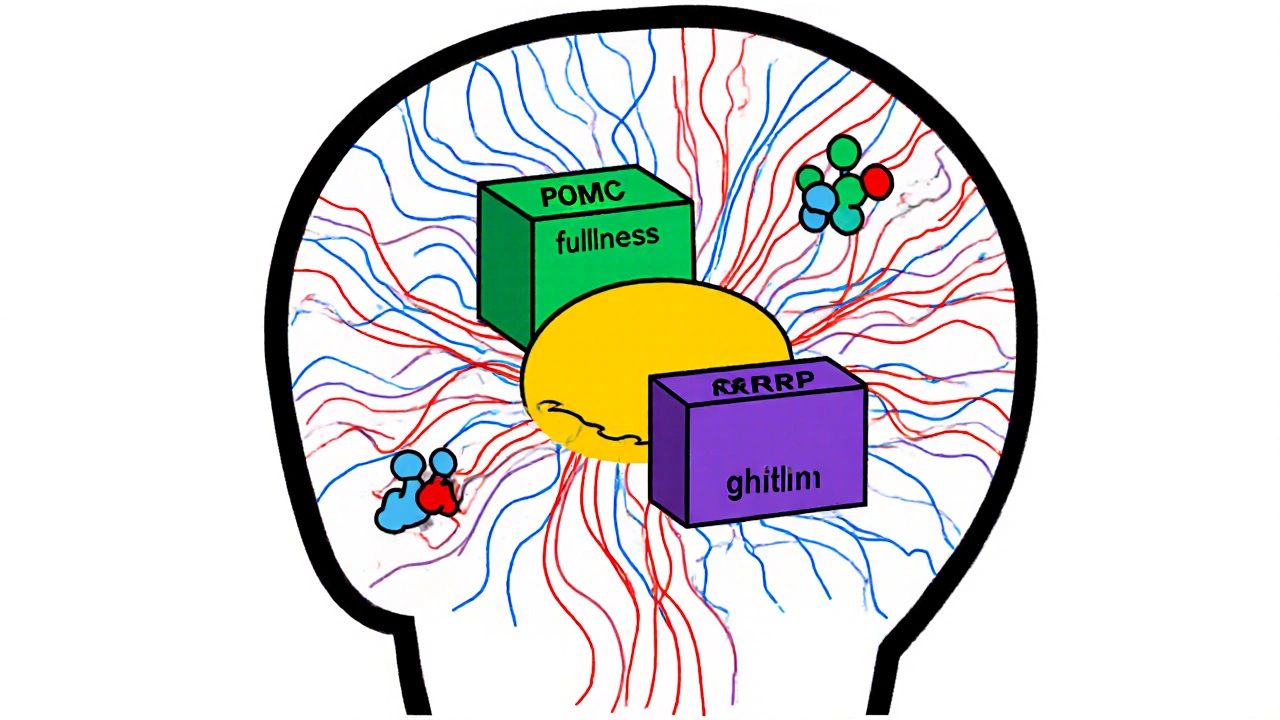
One of the biggest players here is insulin resistance, when cells stop responding to insulin, forcing the pancreas to pump out more. This is the core driver behind type 2 diabetes and is directly worsened by excess fat around organs. Then there's leptin resistance, where your brain stops hearing the "I'm full" signal from fat cells. Even if you have plenty of fat, your brain thinks you're starving. That's why diets often fail: your body fights back with hunger, fatigue, and slowed metabolism. And let's not forget adipose tissue, the fat tissue itself, which becomes inflamed and releases proteins that damage blood vessels and increase clotting risk. This isn't just about weight—it's about systemic damage.
Obesity doesn't happen in a vacuum. It ties directly into metabolic syndrome, a cluster of conditions—high blood sugar, abnormal cholesterol, high blood pressure, and waist size—that raise your risk for heart disease and stroke. These aren't separate problems. They're symptoms of the same root issue: fat tissue gone rogue. That's why treating obesity with just a pill or a short-term diet rarely works. You have to retrain your body's chemistry. The good news? Small, sustained changes—like moving more, sleeping better, and cutting ultra-processed foods—can reverse some of this damage. Your fat cells can become less inflammatory. Your insulin sensitivity can improve. Your leptin levels can normalize.
What you'll find below isn't a list of weight-loss hacks. It's a collection of real, practical insights into how medications, lifestyle choices, and biological processes interact with obesity pathophysiology. From how certain drugs affect fat storage to how inflammation links obesity to heart disease and kidney problems—these posts break down the science without fluff. You'll see how drugs like GLP-1 agonists work on the same pathways your body already struggles with. You'll learn why some people gain weight on certain meds, and how others manage to lose it despite the odds. This isn't about blame. It's about understanding the system so you can work with it—not against it.
Obesity is not just about eating too much-it's a disease of broken hunger signals and metabolic dysfunction. Learn how leptin resistance, brain pathways, and hormones like ghrelin and insulin drive weight gain and make weight loss so hard.