Multiple sclerosis vision loss: Causes, Symptoms, and Management
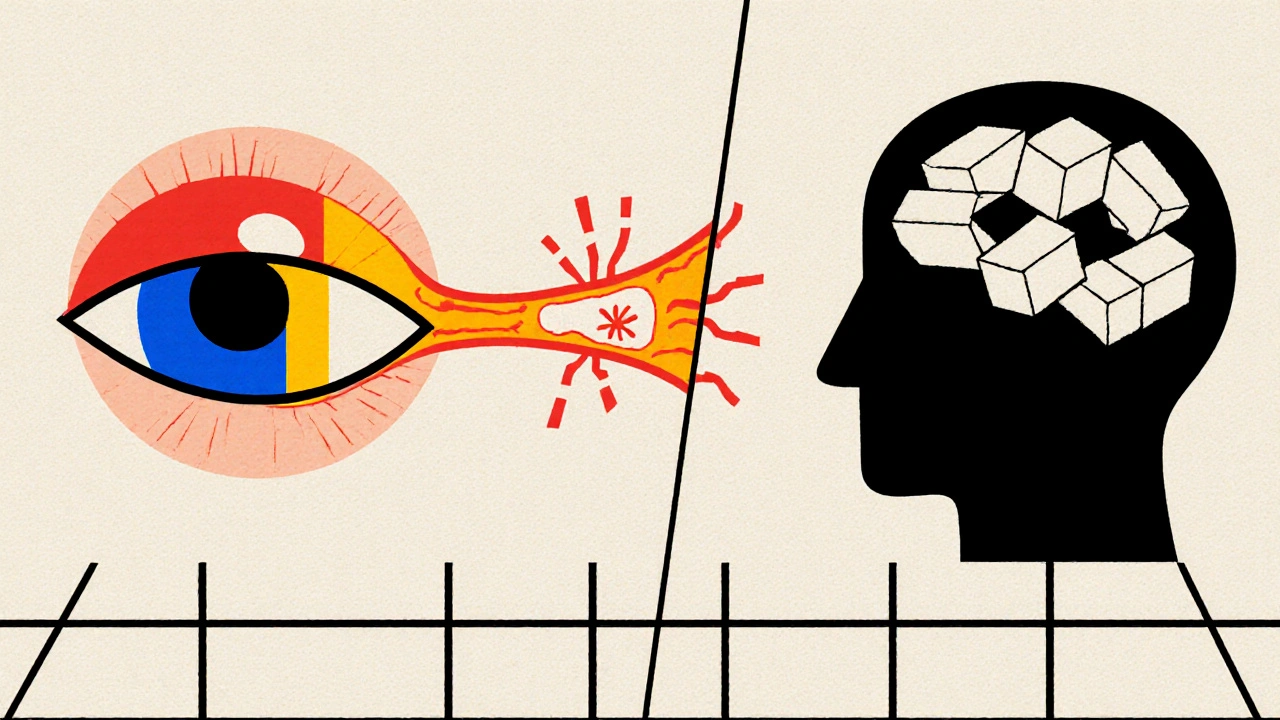
When talking about Multiple sclerosis vision loss, the reduction or distortion of sight caused by the autoimmune disease multiple sclerosis. Also known as MS‑related vision loss, it often arises when the immune system attacks the myelin sheath around optic nerves, disrupting signal transmission from the eyes to the brain.
Key related conditions you should know
The most common trigger is optic neuritis, an inflammation of the optic nerve that leads to pain and rapid visual decline. Optic neuritis requires prompt neuro‑ophthalmic evaluation because early steroid treatment can speed recovery and protect long‑term vision.
Underlying this inflammation is demyelination, the loss of the protective myelin covering nerve fibers, which slows or blocks electrical impulses. Demyelination influences not only optic nerves but also the brain pathways that process visual information, leading to a range of visual field defects.
Patients often report visual field defects, areas of reduced or absent vision such as scotomas, peripheral loss, or blurred central vision. These defects can be graded with perimetry tests, helping clinicians track disease activity and adjust disease‑modifying therapies.
All of these elements sit within the broader specialty of neuro‑ophthalmology, the field that bridges neurology and ophthalmology to diagnose and treat visual problems caused by nervous system disorders. Neuro‑ophthalmologists play a crucial role in differentiating MS‑related vision loss from other causes like retinal disease or glaucoma.
Understanding the link between these entities is essential. Multiple sclerosis vision loss encompasses optic neuritis; optic neuritis requires timely neuro‑ophthalmic assessment; demyelination influences visual field defects; and neuro‑ophthalmology provides the tools to monitor and manage these changes. Together they form a pathway that guides both diagnosis and treatment.
For people living with MS, recognizing early signs—such as sudden eye pain, color desaturation, or blurred vision—can prompt faster intervention. Lifestyle adjustments, like protecting eyes from bright light and maintaining a balanced diet rich in omega‑3 fatty acids, may support overall nerve health. Disease‑modifying drugs (e.g., interferon‑beta, glatiramer acetate) aim to reduce new lesions, which indirectly lowers the risk of future vision loss episodes.
When a relapse occurs, high‑dose corticosteroids are the first line to calm optic nerve inflammation. If steroids are contraindicated, plasma exchange therapy offers an alternative, especially for severe or steroid‑resistant cases. Visual rehabilitation—using low‑vision aids, contrast‑enhancing glasses, and targeted eye‑exercise programs—helps patients retain independence during recovery.
Regular monitoring with MRI scans can reveal new demyelinating plaques near the optic chiasm before symptoms appear. Combining imaging data with visual field testing creates a comprehensive picture of disease activity, allowing neurologists to fine‑tune therapy before irreversible damage sets in.
Beyond medical treatment, psychological support matters. Vision loss can trigger anxiety or depression, so counseling and peer‑support groups are valuable resources. Addressing mental health alongside physical symptoms leads to better overall outcomes.
Below you’ll find a curated collection of articles that dive deeper into each aspect mentioned here— from detailed guides on optic neuritis management to practical tips on visual field testing and the latest advances in disease‑modifying therapies. Explore the resources to arm yourself with the knowledge you need to manage multiple sclerosis vision loss effectively.
Learn how multiple sclerosis impacts eyesight, common visual symptoms, diagnosis tools, and effective treatments to protect your vision.