Medical History: What It Is, Why It Matters, and How It Shapes Your Care
When you talk to a doctor, your medical history, the complete record of your health events, diagnoses, treatments, and reactions over time. Also known as health history, it’s the foundation for every prescription, test, and decision about your body. This isn’t just paperwork—it’s your personal safety net. A missed allergy, an old reaction to a blood thinner, or even how your body handled a thyroid med years ago can change what’s safe to take today.
Your medical history, the complete record of your health events, diagnoses, treatments, and reactions over time. Also known as health history, it’s the foundation for every prescription, test, and decision about your body. This isn’t just paperwork—it’s your personal safety net. A missed allergy, an old reaction to a blood thinner, or even how your body handled a thyroid med years ago can change what’s safe to take today.
Think of it this way: if you’ve ever taken levothyroxine and ate soy at breakfast, your medical history tells your doctor why your thyroid levels might still be off. If you’ve used an EpiPen before, that detail helps them avoid prescribing something that could trigger another reaction. And if you’ve had a bad reaction to a generic drug, that’s not just a complaint—it’s critical data that could prevent a life-threatening error. patient information, the way you understand and report your own health experiences. Also known as patient-reported outcomes, it’s what turns clinical notes into real-world insight. Without it, even the best lab results miss the point.
Modern medicine is starting to connect the dots between your history and your genes. pharmacogenetic testing, a DNA-based tool that predicts how your body will respond to certain drugs. Also known as gene-drug testing, it’s not sci-fi—it’s cutting 30% of dangerous side effects before they happen. But even the most advanced test can’t work without your history. Did your mom have a stroke on warfarin? Did you get a rash on an antibiotic as a kid? That’s the context that makes genetic data useful.
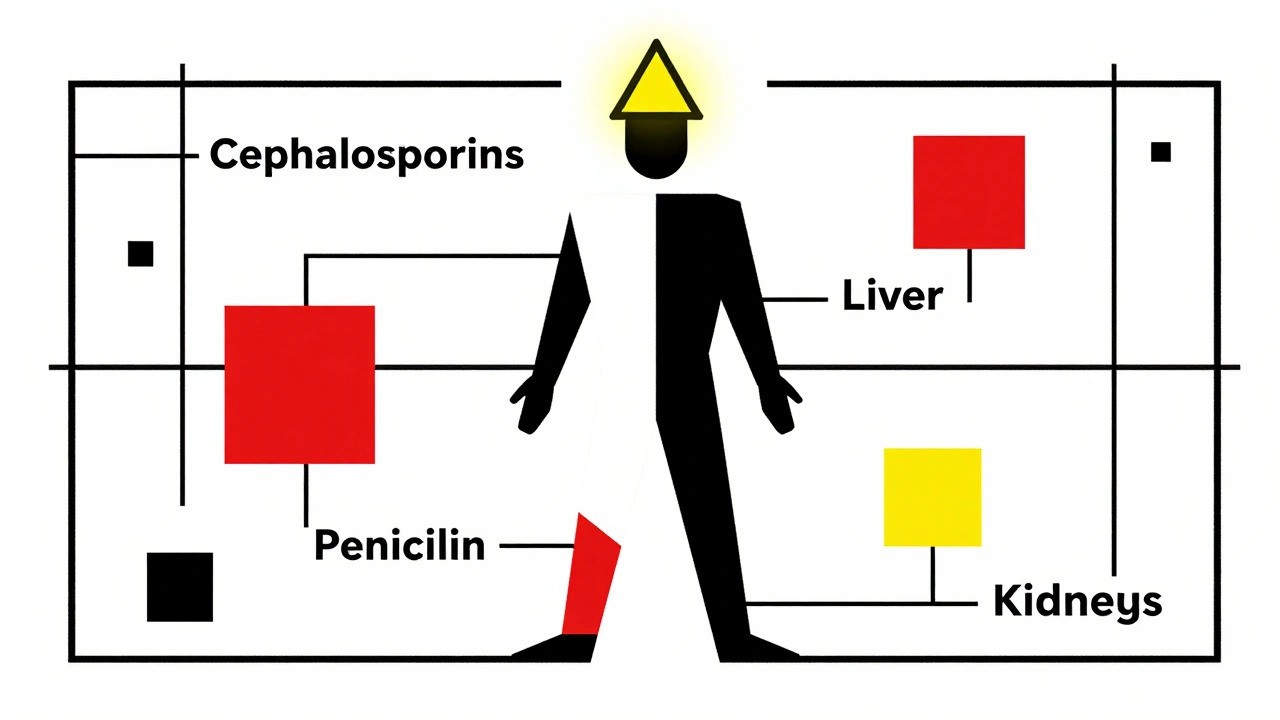
And then there’s the gap between what doctors see and what you feel. adverse drug reactions, unintended, harmful responses to medications. Also known as drug side effects, they’re often underreported because patients don’t know how to describe them—or doctors don’t ask the right questions. That’s why your medical history matters so much. It’s not just about what happened—it’s about what you noticed. Was your vision blurry after a new pill? Did your shoulder pain get worse after a steroid shot? Those details are the clues that turn a generic label into personalized care.
Your medical history isn’t static. It grows with every new symptom, every change in meds, every trip to the ER. And the more accurately you track it—what you took, when, how you felt—the better your care becomes. That’s why the posts below cover everything from how calcium juice blocks absorption of thyroid meds, to how soy can ruin your hormone therapy, to why mixing aspirin with blood thinners is a silent danger. They’re all connected to one thing: your story. And when you know how to tell it, you don’t just get treated—you get protected.
Your medical history directly affects how your body reacts to medications. From past allergies to chronic conditions and polypharmacy, knowing your history can prevent dangerous side effects and even save your life.