LDL – What It Means for Your Health
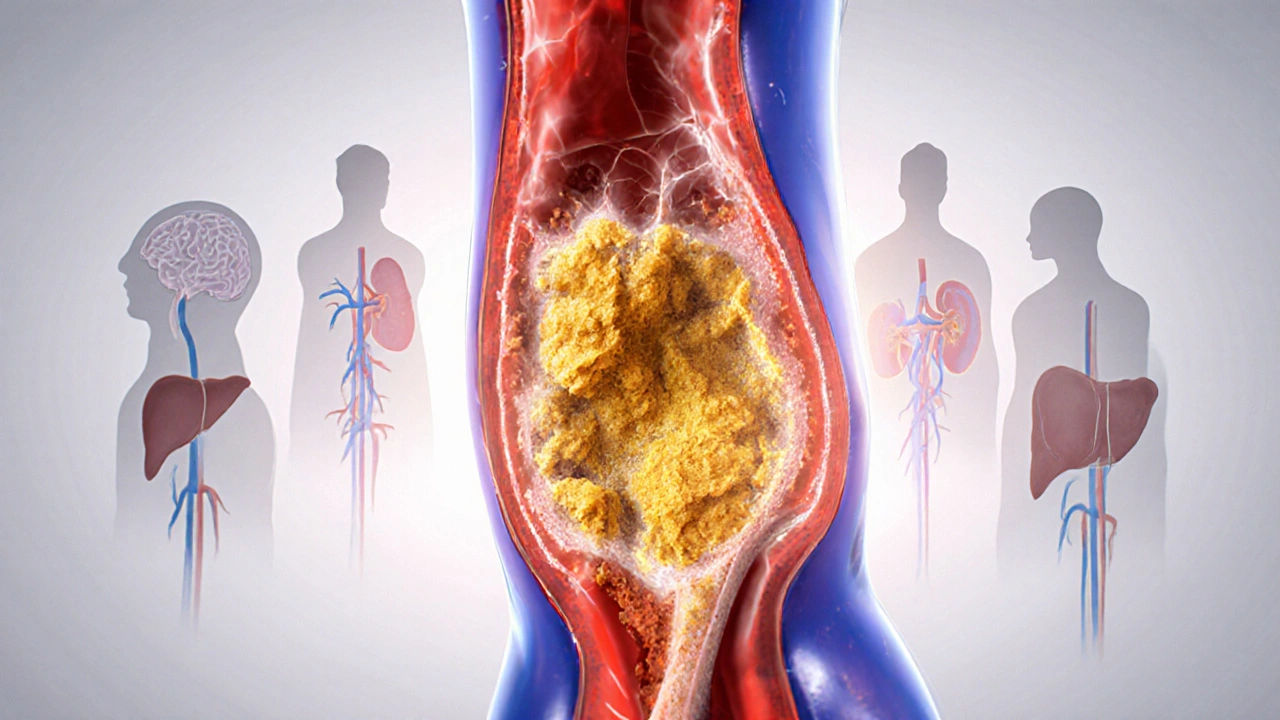
When you hear the term LDL, low‑density lipoprotein, often called the “bad” cholesterol that carries fat through the bloodstream. Also known as low‑density lipoprotein, it plays a direct role in arterial plaque buildup.
Understanding cholesterol, a waxy substance essential for cell membranes and hormone production helps put LDL into context. While cholesterol is necessary, an excess of LDL can tip the balance toward disease. In fact, LDL contributes to heart disease, a condition where arteries narrow or block, leading to heart attacks or strokes. The relationship is simple: higher LDL levels increase the chance of plaque formation, which narrows arteries and raises cardiac risk. Doctors use a lipid panel, a blood test that measures LDL, HDL, total cholesterol, and triglycerides to gauge this risk and decide on treatment.
How Statins and Lifestyle Choices Interact with LDL
One of the most common ways to lower LDL is with statins, prescription drugs that safely reduce the production of cholesterol in the liver. Statins have proven to cut LDL by up to 50%, which in turn lessens plaque buildup and lowers heart‑disease events. But medication isn’t the only tool. Diet, exercise, and weight management also shift LDL numbers. A diet low in saturated fats, rich in fiber, and balanced with healthy fats can reduce LDL production, while regular aerobic activity helps raise HDL (the “good” cholesterol) that counters LDL’s effects. When you combine statins with these lifestyle tweaks, the result is often a healthier lipid profile and a clearer path to heart‑healthy living.
Below you’ll find a curated set of articles that dig deeper into each of these topics. Whether you want to decode your lab results, compare medication options, or learn food swaps that naturally curb LDL, the collection offers practical tips and evidence‑backed guidance to help you take control of your heart health.
Learn how high blood cholesterol harms the heart, brain, liver and more, and discover practical steps-diet, exercise, screening, and meds-to keep your levels in check.