Cholesterol Risk Assessment Calculator
Enter your cholesterol values and risk factors then click "Assess My Cholesterol Risk" to see your assessment.
Key Takeaways
- High blood cholesterol raises the risk of heart disease, stroke, and peripheral artery problems.
- LDL (bad) cholesterol and triglycerides drive plaque buildup, while HDL (good) cholesterol helps protect arteries.
- Regular screening, a balanced diet, and physical activity are the most effective ways to lower dangerous levels.
- Statin medications can be lifesavers, but lifestyle changes often reduce the need for drugs.
- Early detection and management improve long‑term quality of life and reduce medical costs.
Understanding high blood cholesterol is the first step toward protecting every organ that relies on clean blood flow.
High blood cholesterol is a condition where the concentration of cholesterol in the bloodstream exceeds the limits set by health authorities. When this happens, the walls of arteries become a playground for plaque, and the ripple effects spread far beyond the heart.
What Cholesterol Is and Why It Matters
Cholesterol is a fat‑like molecule that helps build cell membranes and produce hormones. Your liver makes most of it, but you also get cholesterol from animal‑based foods.
Three main lipid particles travel together in the blood:
- LDL cholesterol (low‑density lipoprotein) - often called “bad” cholesterol because it deposits cholesterol in artery walls.
- HDL cholesterol (high‑density lipoprotein) - the “good” cholesterol that scoops excess cholesterol away for disposal.
- Triglycerides - another type of fat that, when elevated, signals metabolic stress.
How Elevated Levels Damage the Body
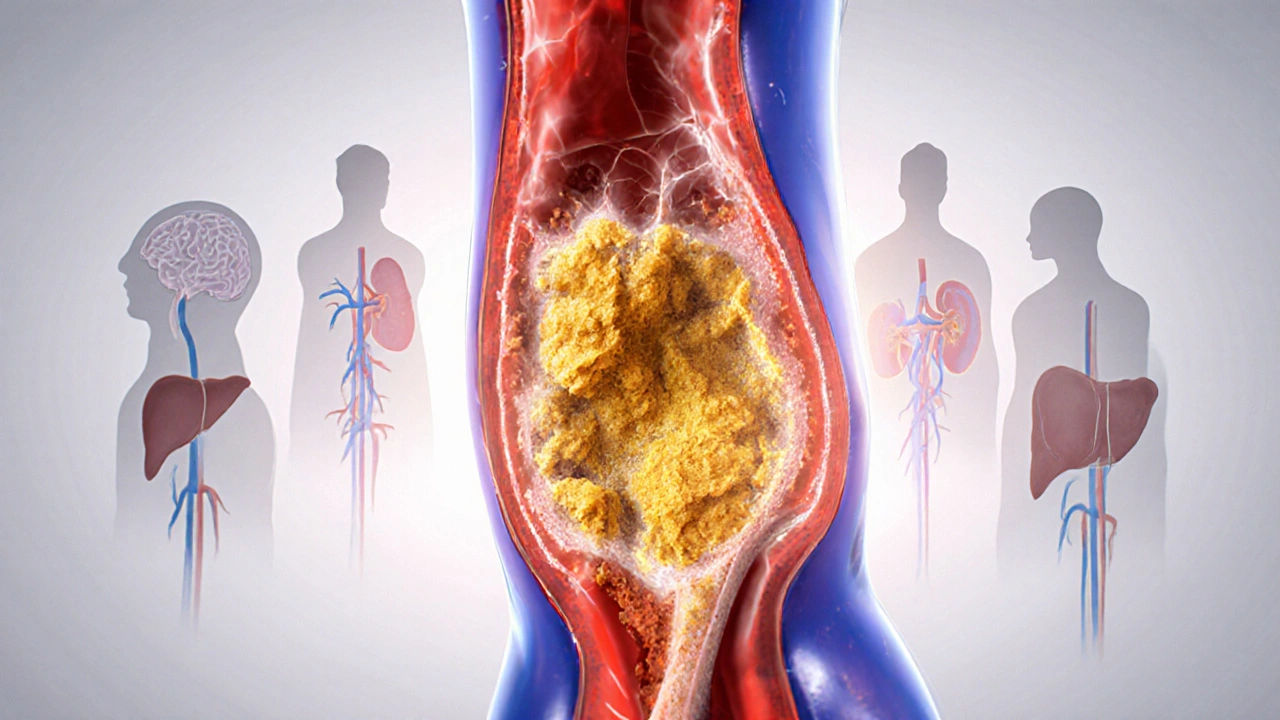
The biggest danger comes from atherosclerosis (hardening and narrowing of the arteries). LDL particles infiltrate the inner lining of arteries, where they oxidize and trigger inflammation. Over months and years, this creates plaque-an ugly mix of cholesterol, calcium, and cellular debris.
When plaque grows:
- Blood flow to the heart muscle can be blocked, leading to heart disease (ischemic heart disease or coronary artery disease).
- Pieces of plaque may break off, travel to the brain, and cause a stroke (cerebral vascular accident).
- Peripheral arteries in the legs and arms can narrow, causing pain, ulcers, or even gangrene.
High triglycerides also worsen the picture by making the blood more viscous, which raises blood pressure and strains the heart.

Beyond the Heart: Other Organs Feel the Impact
The liver, which regulates cholesterol production, can become fatty when blood lipids stay high. This fatty liver disease raises the risk of liver inflammation and, eventually, cirrhosis.
Kidneys filter blood under pressure. When vessels leading to them narrow, chronic kidney disease can develop, reducing the body's ability to balance fluids and electrolytes.
Even the brain’s micro‑circulation suffers; studies link chronic high cholesterol to cognitive decline and an increased chance of Alzheimer’s‑type changes.
How to Spot the Problem: Testing and Numbers
Because high cholesterol rarely shows symptoms, blood tests are the only reliable way to catch it early. The standard panel includes:
- Total cholesterol (mg/dL)
- LDL cholesterol (mg/dL)
- HDL cholesterol (mg/dL)
- Triglycerides (mg/dL)
Guidelines from the American Heart Association (2024 update) suggest:
- LDL < 100mg/dL for most adults (below 70mg/dL for those with existing heart disease).
- HDL ≥ 60mg/dL is protective; men below 40mg/dL and women below 50mg/dL are at higher risk.
- Triglycerides < 150mg/dL.
When results exceed these thresholds, doctors usually assess additional risk factors such as age, smoking status, blood pressure, and family history before deciding on treatment.
Managing High Cholesterol: Lifestyle First
Most experts agree that lifestyle changes can lower LDL by 10‑30% and raise HDL by 5‑10%.
- Diet: Swap saturated fats (red meat, full‑fat dairy) for unsaturated fats (olive oil, nuts, fatty fish). Aim for 5‑7 servings of fruits and vegetables daily.
- Fiber: Soluble fiber (oats, beans, apples) binds cholesterol in the gut and helps excrete it.
- Physical activity: At least 150minutes of moderate aerobic exercise per week improves HDL and lowers triglycerides.
- Weight control: Losing 5‑10% of body weight can reduce LDL by up to 15%.
- Smoking cessation: Quitting raises HDL within weeks and reduces overall cardiovascular risk.

When Medication Is Needed: Statins and Beyond
If lifestyle tweaks don’t bring LDL under target, most physicians prescribe statins (HMG‑CoA reductase inhibitors). Statins lower cholesterol production in the liver and can cut heart‑attack risk by about 25‑30%.
Common statins include atorvastatin, rosuvastatin, and simvastatin. Side effects are generally mild-muscle aches or occasional liver enzyme elevations-but patients should discuss any concerns with their doctor.
For people who can’t tolerate statins, alternatives such as ezetimibe, PCSK9 inhibitors, or omega‑3 fatty‑acid supplements may be used. Each has specific indications and cost considerations, so a personalized plan is essential.
Putting It All Together: A Practical Checklist
- Get a lipid panel every 4‑6years if you’re under 45 and have no risk factors; more often if you have a family history.
- Track food intake with an app or journal to spot hidden saturated fats.
- Schedule at least 30minutes of brisk walking, cycling, or swimming most days.
- Ask your doctor about a statin trial if LDL stays above 130mg/dL after 3months of lifestyle work.
- Re‑check your lipid numbers 4‑12weeks after any diet or medication change.
Frequently Asked Questions
Can I have high cholesterol without any symptoms?
Yes. Most people feel fine until a heart attack, stroke, or other serious event occurs. That’s why regular blood tests are crucial.
Is HDL really "good" cholesterol?
HDL helps transport excess cholesterol back to the liver for disposal, which slows plaque buildup. Higher HDL levels are linked to lower heart‑disease risk.
How quickly can lifestyle changes lower LDL?
Most people see a 5‑10% drop within 6‑8weeks if they cut saturated fat, add soluble fiber, and exercise regularly. Bigger drops may take 3‑6months.
Are statins safe for long‑term use?
Long‑term studies show statins reduce cardiovascular events without major safety concerns for most adults. Regular monitoring of liver enzymes and muscle symptoms is recommended.
What foods are best for lowering cholesterol?
Oats, barley, beans, nuts, fatty fish (salmon, mackerel), olive oil, and plenty of fruits and vegetables are all proven to improve lipid profiles.
Comparison of Key Lipid Markers
| Marker | Ideal Range (mg/dL) | Health Impact |
|---|---|---|
| LDL | < 100 ( < 70 if high risk ) | High levels promote plaque buildup → heart disease, stroke |
| HDL | ≥ 60 (men ≥ 40, women ≥ 50) | Higher levels help remove cholesterol → protective effect |
| Triglycerides | < 150 | Elevated levels increase blood viscosity and raise heart‑attack risk |
Keeping LDL low, HDL high, and triglycerides within range creates the best environment for a healthy circulatory system.
Comments (14)
Howard Mcintosh
October 6, 2025 AT 17:53
Yo, ditch the junk food and get that LDL down pronto!
Jeremy Laporte
October 11, 2025 AT 08:59
Adding a handful of almonds or a splash of olive oil to your meals can gently nudge LDL lower while giving you a dose of heart‑friendly monounsaturated fats.
Whole grains like oats provide soluble fiber that binds cholesterol in the gut, helping the body excrete it.
Regular brisk walks of 30 minutes most days boost HDL and improve overall lipid balance.
Keeping an eye on portion sizes prevents excess calorie intake, which is key for weight control and triglyceride management.
Stay consistent and you’ll see gradual improvements in your blood work.
Andy Lombardozzi
October 16, 2025 AT 00:06
Regular aerobic exercise boosts HDL levels by improving the efficiency of lipid transport.
Studies show that 150 minutes per week of moderate activity can raise HDL by 5 to 10 percent.
In addition, vigorous interval training has been linked to modest reductions in LDL.
The mechanism involves increased activity of lipoprotein lipase, an enzyme that clears triglyceride‑rich particles from the bloodstream.
Dietary fiber, especially soluble forms found in oats, barley, and legumes, binds bile acids and forces the liver to use more cholesterol to replace them.
This process gradually lowers circulating LDL concentrations.
Substituting saturated fats with polyunsaturated oils such as canola or sunflower oil reduces the hepatic synthesis of cholesterol.
Plant sterols added to fortified spreads competitively inhibit cholesterol absorption in the intestines.
For individuals who smoke, cessation alone can produce a measurable rise in HDL within weeks.
Weight loss of even 5 percent of body mass can translate into a 6 to 8 percent drop in LDL.
Limiting refined carbohydrate intake helps control triglyceride spikes that would otherwise impair HDL function.
When lifestyle measures fail to achieve target LDL levels, statin therapy reduces cardiovascular events by roughly a quarter in primary‑prevention trials.
Newest agents such as PCSK9 inhibitors provide up to a 60 percent LDL reduction but are reserved for high‑risk patients due to cost.
Regular monitoring of lipid panels every six months after a therapeutic change ensures that treatment goals are being met.
Ultimately, a combination of diet, exercise, weight management, and, when needed, medication offers the most robust defense against atherosclerotic disease.
Joshua Ardoin
October 18, 2025 AT 07:39
Adding a daily 20‑minute walk fits perfectly into the plan you just laid out, and the extra steps help burn those extra triglycerides 🚶♂️💥.
Glenn Gould
October 22, 2025 AT 22:46
Yo, swap soda for water, your triglycerides will thank you!
Poonam Sharma
October 25, 2025 AT 06:19
Listen, the sugar tsunami in fizzy drinks is a silent war on our arteries, and the only victory comes from a disciplined, home‑cooked regimen that honors our heritage of wholesome grains and spices.
Meigan Chiu
October 29, 2025 AT 20:26
While many hail statins as miracle workers, the data also reveal a non‑trivial incidence of myopathy and elevated liver enzymes that cannot be brushed aside.
Moreover, the blanket prescription of these drugs without individualized risk assessment undermines the principle of precision medicine.
Patricia Hicks
November 1, 2025 AT 03:59
It’s true that medications have side effects, but when we pair them with a sturdy foundation of diet, exercise, and stress management, the overall risk profile becomes far more favorable.
Think of the body as a garden: the right nutrients, sunlight, and pruning keep weeds at bay, while occasional herbicides (the statins) are only needed when the invasive species get out of control.
By monitoring labs regularly, patients and clinicians can adjust dosages or switch to alternatives like ezetimibe or PCSK9 inhibitors, ensuring that therapy stays both effective and tolerable.
In practice, a collaborative approach empowers individuals to take charge of their heart health, turning the narrative from one of passive medication intake to active, informed stewardship.
Quiana Huff
November 5, 2025 AT 19:06
Yo fam, NADH‑linked pathways get supercharged when you slash those saturated fats, leading to a smoother lipid profile 🚀👍.
William Nonnemacher
November 8, 2025 AT 02:39
Statins work but watch for muscle pain and liver issues.
Alex Ramos
November 12, 2025 AT 17:46
Indeed, the therapeutic index of statins warrants meticulous dosage titration; consequently, clinicians should employ periodic lipid panels, hepatic function tests, and patient‑reported outcomes to optimize treatment efficacy.
Mita Son
November 15, 2025 AT 01:19
But don’t forget that even with perfect labs, lifestyle slip‑ups can quickly reverse gains, so consistency remains king.
ariel javier
November 19, 2025 AT 16:26
It is reprehensible how many ignore the stark evidence that unchecked cholesterol accelerates vascular calcification, yet persist in detrimental eating habits.
Bryan L
November 21, 2025 AT 23:59
Hang in there, small changes add up, and you’ve got a community cheering you on 😊.