Diabetes Medications: What Works, What to Avoid, and How to Stay Safe
When you have diabetes, your body either doesn’t make enough insulin, a hormone that helps move sugar from your blood into your cells or can’t use it right. That’s where diabetes medications, drugs designed to help manage blood sugar levels come in. These aren’t one-size-fits-all—some people need insulin injections, others take pills that help their body respond better to insulin, and some use a mix. The right choice depends on your type of diabetes, your lifestyle, and what else is going on in your health.
It’s not just about popping a pill. Many diabetes medications, drugs designed to help manage blood sugar levels can clash with other drugs or even foods. For example, calcium-fortified juice, a common breakfast drink that can interfere with how some drugs are absorbed can block the effect of thyroid meds, which many diabetics also take. Same goes for soy products, foods like tofu and edamame that can reduce how well levothyroxine works. Even something as simple as timing your meals matters—eating right after taking your med can make it useless or too strong. And if you’re on insulin, you can’t ignore expiration dates. Expired insulin doesn’t just lose power—it can send your blood sugar wild without you knowing.
People with type 1 diabetes, a condition where the body stops producing insulin entirely often turn to insulin pump therapy, a device that delivers steady insulin through a small tube under the skin. It’s not for everyone—it takes work to learn, but it gives more control than shots. But even with pumps, you still need to watch for hidden risks. Some meds for cholesterol or heart issues can mess with how your body handles sugar. And if you’re taking blood thinners like aspirin or Eliquis, combining them with diabetes drugs can raise your bleeding risk. It’s not about fear—it’s about awareness. The more you know about what’s in your body and how things interact, the less likely you are to get caught off guard.
There’s no magic bullet. What works for one person might not work for another. That’s why your meds need to be as personal as your diet or exercise plan. You’re not just managing sugar—you’re managing a system. And that system is affected by your sleep, stress, travel, even the humidity where you live. That’s why the posts below cover everything from how to read your label correctly to what happens when your insulin sits in a hot car. You’ll find real talk about what to do when side effects show up, how to tell if your generic drug is truly equivalent, and how to report a bad reaction if something goes wrong. This isn’t theory. It’s what people actually need to know to stay safe and in control every single day.
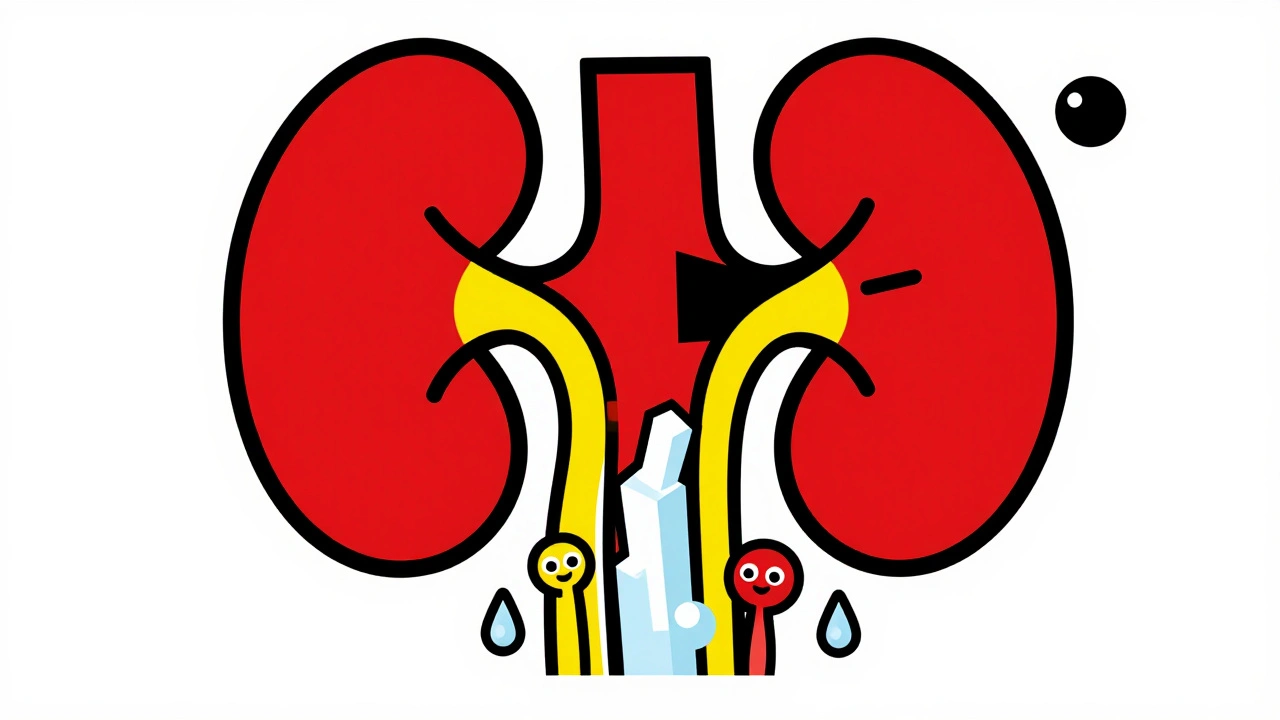
SGLT2 inhibitors help control diabetes by flushing sugar into urine - but that increases yeast and urinary tract infection risks. Learn who’s most at risk, what symptoms to watch for, and safer alternatives.