SGLT2 Inhibitor Infection Risk Calculator
This calculator helps you understand your personal risk of developing urinary tract infections or yeast infections while taking SGLT2 inhibitors. Based on a 2024 study in Diabetes Care, a score of 3 or higher indicates over 15% chance of serious infection.
The tool asks about 5 key risk factors from the study. Each 'yes' answer equals 1 point. Scores of 3+ are considered high risk and may warrant discussing alternative medications with your doctor.
When you’re managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar or weight gain feels like a win. That’s why SGLT2 inhibitors became so popular. But for many people, the relief of better glucose control comes with an unexpected side effect: recurring yeast infections and serious urinary complications.
How SGLT2 Inhibitors Work - and Why They Cause Infections
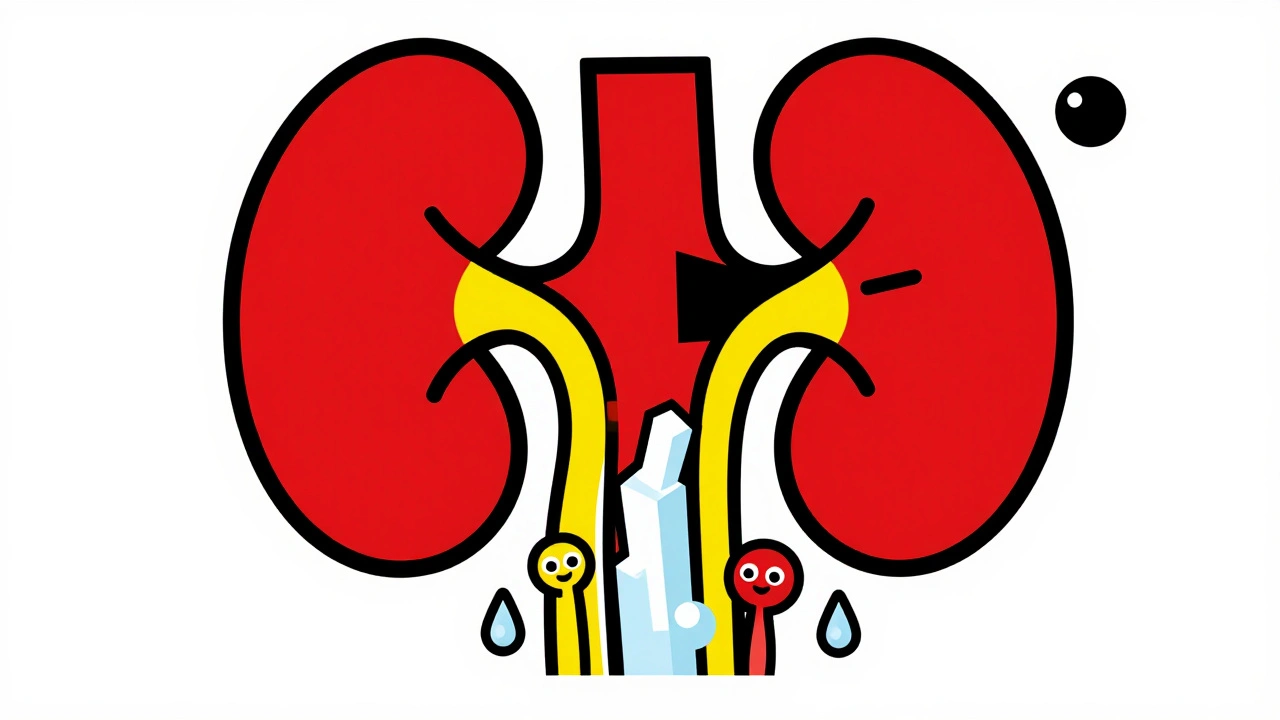
SGLT2 inhibitors like canagliflozin (a diabetes medication that blocks glucose reabsorption in the kidneys), dapagliflozin (a drug that increases sugar excretion through urine), and empagliflozin (a medication linked to heart failure benefits) work by making your kidneys dump excess sugar into your urine. That’s how they lower blood sugar - no insulin needed. But here’s the catch: sugar in urine is food for yeast and bacteria. Every day, someone on these drugs passes 40 to 110 grams of glucose in their pee. That’s roughly 10 teaspoons of sugar - all sitting in the bladder and genital area. It’s like leaving a bowl of syrup out overnight. Candida, the fungus that causes yeast infections, thrives in that environment. That’s why up to 5% of women taking these drugs develop vulvovaginal candidiasis, and about 3% of men get balanitis - swelling and redness of the penis.The Numbers Don’t Lie: Infection Risk Is Real
A 2022 meta-analysis in Pharmacology Research & Perspectives looked at data from over 40,000 patients. It found that SGLT2 inhibitors nearly double the risk of urinary tract infections compared to other diabetes drugs like DPP-4 inhibitors or sulfonylureas. The absolute increase? Between 2.1% and 3.8% more infections per year. That might sound small, but when you’re the one dealing with daily burning, urgency, or recurrent infections, it’s not small at all. Genital infections are even more common. These drugs raise the risk of yeast infections by 4.5 times compared to DPP-4 inhibitors. That’s not a minor inconvenience - it’s enough that 23.7% of patients in a Swedish study stopped taking their SGLT2 inhibitor within two years because of these side effects.When It Gets Dangerous: Beyond Yeast Infections
Most infections are mild - itching, discharge, discomfort. But some aren’t. The FDA reviewed reports from 2013 to 2014 and found 19 cases of urosepsis - a life-threatening bloodstream infection that started in the urinary tract. All 19 required hospitalization. Four ended up in the ICU. Two needed dialysis because their kidneys failed. One case, published by the NIH, involved a 64-year-old woman who developed emphysematous pyelonephritis (a rare, gas-forming kidney infection). She had no prior history of UTIs. Within weeks of starting dapagliflozin, she had severe pain, fever, and gas in her kidney tissue. She needed antibiotics for 14 days and later required surgery to drain an abscess. She went back on the drug 11 months later - and got the same infection again. Then there’s Fournier’s gangrene (a fast-spreading necrotizing infection of the genitals and perineum). It’s rare - less than 1 in 1,000 users - but it kills. The European Medicines Agency added it to the warning labels in 2016. Symptoms? Sudden, severe pain or swelling in the genital area, fever, and a feeling of being extremely unwell. If you have this, you need emergency surgery and IV antibiotics. Delay by even a day can be fatal.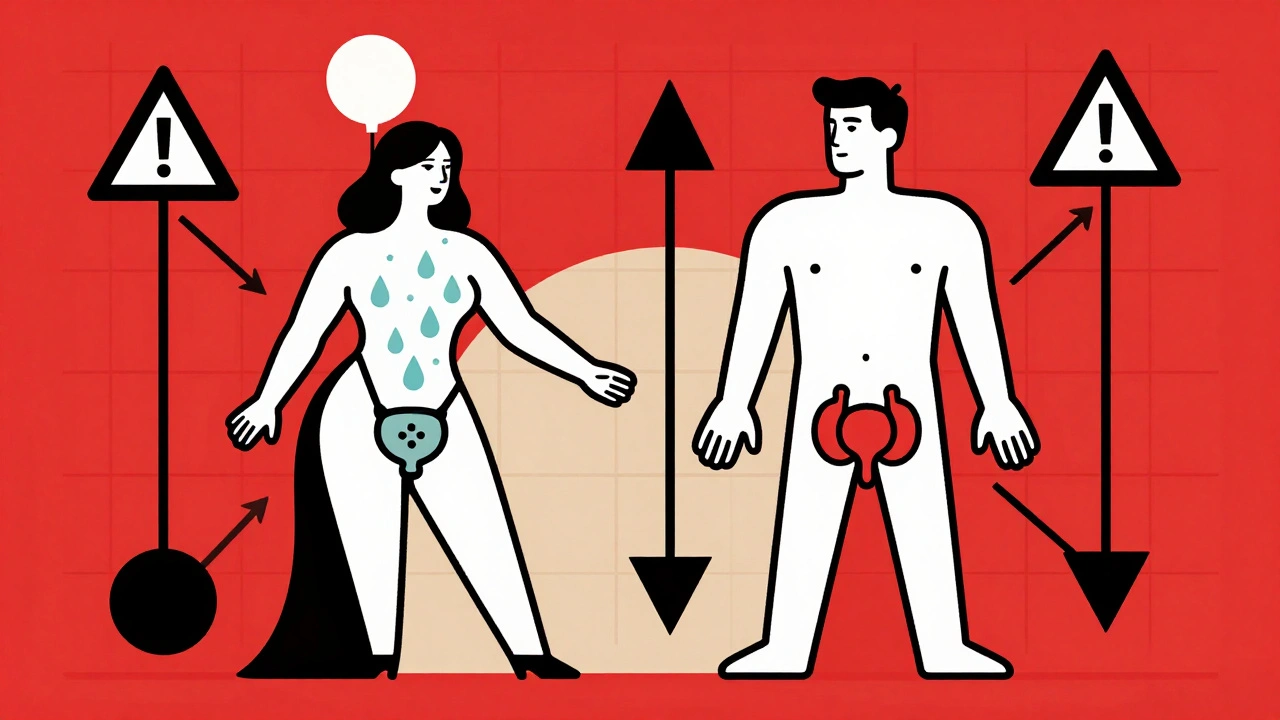
Who’s at Highest Risk?
Not everyone on SGLT2 inhibitors gets infections. But some people are far more likely to. Risk goes up if you:- Are female (due to shorter urethra and proximity to vaginal flora)
- Have had previous yeast or UTI infections
- Are over 65
- Have poor blood sugar control (HbA1c above 8.5%)
- Have kidney problems (eGFR below 60)
- Are immunocompromised or have urinary tract abnormalities
What Doctors Recommend - and What You Should Do
The American Diabetes Association says clearly: check your history of urinary infections before starting an SGLT2 inhibitor. If you’ve had three or more UTIs in the past year, they recommend picking a different drug - like a GLP-1 receptor agonist or a DPP-4 inhibitor. If you’re already on one and it’s working well for your heart or kidneys, don’t stop cold turkey. Talk to your doctor. But here’s what you must do:- Wash your genital area daily with mild soap and dry thoroughly
- Drink at least 2 liters of water a day - flush out the sugar
- Urinate after sex
- Wear cotton underwear, avoid tight pants
- Never ignore symptoms: burning, itching, unusual discharge, frequent urination, or fever
Are There Alternatives?
Yes. And for many people, they’re better.- GLP-1 receptor agonists (like semaglutide or liraglutide) - lower blood sugar, help with weight loss, protect the heart and kidneys - and don’t cause yeast infections.
- DPP-4 inhibitors (like sitagliptin or linagliptin) - minimal infection risk, no weight gain, low hypoglycemia risk.
- Metformin (the first-line diabetes drug) - still the safest, cheapest, and most studied option for most people.
What’s New in 2025?
New research is trying to fix the problem. A 2023 FDA safety update found that people taking cranberry supplements had a 29% lower rate of UTIs while on SGLT2 inhibitors. It’s not FDA-approved for this use, but some doctors now suggest it - especially for women with recurrent infections. Drugmakers are also working on dual SGLT1/2 inhibitors that reduce sugar absorption in the gut before it reaches the kidneys. Less sugar in urine = lower infection risk. Early trials look promising. There’s also a new 5-point risk calculator now being used in endocrinology clinics. If you’re considering an SGLT2 inhibitor, ask your doctor if you qualify for this screening. It could save you from a hospital stay.Bottom Line: Benefits vs. Risks
SGLT2 inhibitors are not bad drugs. They’re life-saving for people with heart failure, kidney disease, or high cardiovascular risk. But they’re not magic bullets. The sugar in your urine isn’t just a side effect - it’s a direct cause of infection. If you’re on one and haven’t had problems, keep doing what you’re doing - but stay alert. If you’re thinking about starting one, ask: Do I have a history of infections? Am I at risk for heart or kidney complications? Are there safer options? For many, the answer is yes - there are safer options. And that’s not weakness. It’s smart management.Can SGLT2 inhibitors cause yeast infections in men?
Yes. While vulvovaginal yeast infections are more common in women, men can develop balanitis - inflammation and redness of the penis - from the sugar in urine. Studies show about 3% of men on SGLT2 inhibitors experience this, compared to less than 1% on other diabetes drugs. Good hygiene and hydration reduce the risk.
How soon after starting SGLT2 inhibitors do infections usually appear?
Most genital and urinary infections occur within the first 3 to 6 months of starting the drug. The FDA found that the median time to a serious infection like urosepsis was 45 days. That’s why early monitoring is critical - don’t wait for symptoms to get worse.
Is it safe to take cranberry supplements with SGLT2 inhibitors?
There’s no known interaction, and a 2023 FDA review found cranberry products reduced UTI risk by 29% in SGLT2 inhibitor users. While not officially approved for this use, many doctors recommend it as a preventive step, especially for women with a history of UTIs. Choose unsweetened capsules or juice without added sugar.
Should I stop my SGLT2 inhibitor if I get a yeast infection?
Not necessarily. Mild yeast infections can be treated with antifungals while continuing the drug. But if you have recurrent infections - three or more in a year - your doctor may recommend switching to a different diabetes medication. The infection risk isn’t worth the trade-off if your heart and kidneys are stable.
Do SGLT2 inhibitors cause kidney damage?
No - the opposite. These drugs are proven to slow kidney disease progression in people with type 2 diabetes and chronic kidney disease. But if a urinary infection spreads to the kidneys (like in pyelonephritis or urosepsis), it can cause acute kidney injury. That’s why treating infections early is so important. The drug protects your kidneys long-term - but untreated infections can hurt them fast.
Comments (15)
Ada Maklagina
December 5, 2025 AT 21:24
I got a yeast infection 6 weeks after starting empagliflozin. No big deal, right? Until you're itching at 3am and your doctor says 'just use clotrimazole.' Like that fixes the syrup bath my kidneys are dumping into my pants. I switched to semaglutide. Best decision ever.
Washed my underwear with vinegar. Still no relief. The drug was the problem.
Stephanie Bodde
December 7, 2025 AT 10:35
You're not alone 😊 I had the same thing! I thought it was just stress or my new yoga pants. Turns out? Sugar in my pee. I started drinking 3L of water a day + cranberry capsules. No more recurrences. You got this! 💪
Laura Saye
December 9, 2025 AT 00:50
The biochemical irony here is profound. We pharmacologically engineer a mechanism to excrete glucose as a therapeutic lever-yet we ignore the ecological consequences of that excretion within the human microbiome. The urinary tract is not a sterile conduit; it is a dynamic ecosystem. Introducing 10 teaspoons of fermentable substrate daily is not a side effect-it is an environmental disruption. The rise in candidiasis is not an accident. It is a predictable outcome of metabolic intervention without ecological foresight. We treat the symptom, not the system.
Philip Kristy Wijaya
December 10, 2025 AT 04:37
Let me tell you something about Big Pharma they dont want you to know. SGLT2 inhibitors were pushed because they make money not because they save lives. The infection risk? A footnote in the prospectus. I've seen patients get Fourniers gangrene and the reps still show up with free samples. This is not medicine. This is capitalism with a stethoscope. And dont even get me started on how they buried the 2014 urosepsis data for two years
Carole Nkosi
December 11, 2025 AT 05:34
You people are so obsessed with Western medicine. In my village in South Africa, we use neem leaves, garlic paste, and prayer. No drugs. No hospitals. No sugar in urine. The body heals itself when you stop poisoning it with pills designed by men in suits who never even had diabetes. This whole system is broken. You're treating symptoms because you refuse to see the root: processed food. Sugar is the real villain. Not the drug. The culture.
William Chin
December 11, 2025 AT 08:41
The data is unequivocal. The FDA's own pharmacovigilance database confirms a statistically significant increase in genitourinary infections with SGLT2 inhibitors, with p-values below 0.001 across multiple RCTs. The 4.5-fold relative risk increase is not marginal-it is clinically actionable. Any clinician who prescribes this class without first evaluating a patient's history of recurrent candidiasis or UTI is practicing negligent medicine. The ADA guidelines are not suggestions. They are standards of care. Failure to adhere constitutes malpractice.
an mo
December 12, 2025 AT 10:15
The real issue isn't the drug. It's that the FDA approved this without proper long-term microbiome studies. We're playing Russian roulette with our gut flora. And now they want us to take cranberry supplements? That's not prevention. That's damage control for a product they knew was risky. The pharmaceutical industry doesn't care if you get a yeast infection. They care if you keep buying pills. And they know you'll come back for more after the first infection. It's a business model.
Jennifer Patrician
December 12, 2025 AT 16:33
Cranberry? Are you kidding me? That's what they want you to believe. The real solution? Stop taking the drug. But they don't want you to know that because the patent expires in 2026 and they're making billions. The FDA knows this. Your doctor knows this. But they're all too scared to say it out loud. This is controlled chaos. You're being used as a test subject. And the 'risk calculator'? That's just to make you feel better about taking poison.
Lynette Myles
December 13, 2025 AT 15:23
Fournier’s gangrene is not rare. It’s underreported.
Mark Curry
December 15, 2025 AT 08:27
I was on canagliflozin for a year. No issues. Then I got a UTI. Treated it. Went back on. Got another. Third time, I switched to metformin. No more problems. I'm 62, overweight, but my A1c is 6.8 and I feel better than ever. Sometimes the old way is the right way.
Also, drink water. Like, a lot.
Ali Bradshaw
December 17, 2025 AT 02:57
I've been on dapagliflozin for 18 months. Had one mild yeast infection-treated it with fluconazole. I drink 2.5L water daily, wear cotton, and dry thoroughly. I also have heart failure. This drug cut my hospitalizations in half. For me? Worth it. But I get it. Not everyone's in the same boat. Know your risk. Talk to your doc. Don't panic. Just be smart.
aditya dixit
December 18, 2025 AT 11:42
In India, we have a saying: 'The medicine that cures one may harm another.' SGLT2 inhibitors are powerful, yes. But they are not universal. For someone with kidney disease and heart failure, they are life-changing. For someone with recurrent UTIs and no cardiovascular risk? They are a gamble. The key is personalized medicine. Not blanket prescriptions. Ask your doctor: What is my risk? What is my benefit? Not just: What's the newest pill?
Annie Grajewski
December 19, 2025 AT 17:27
So like... you're telling me that the drug that's supposed to help my diabetes is basically making my pee sweet? And then we're surprised when yeast throws a rave in my undies? 😭 I thought I was just bad at hygiene. Turns out my kidneys are basically a sugar factory. And now I gotta take cranberry pills? Like a gummy bear for my bladder? This is the future? 🤦♀️
Chris Brown
December 21, 2025 AT 07:52
It is not the responsibility of the patient to mitigate the consequences of a pharmaceutical agent that was approved with inadequate scrutiny. To suggest that drinking water or wearing cotton underwear is an adequate countermeasure to a 4.5-fold increase in fungal infection risk is not merely inadequate-it is morally negligent. The onus is not on the individual to adapt to a flawed intervention. The onus is on the regulatory bodies, the manufacturers, and the medical establishment to withdraw or reformulate a drug that systematically creates a pathological environment within the human body. This is not medicine. This is negligence dressed in white coats.
Mellissa Landrum
December 22, 2025 AT 08:10
They knew. They KNEW. I read the FDA filings. The first trial in 2011 had 17 cases of balanitis. They buried it. Now they say 'wash better'? Like we're toddlers? I'm a nurse. I've seen the abscesses. I've seen the amputations. This isn't about hygiene. It's about profit. And if you're still on this drug? You're being played.