Appetite Regulation: How Medications and Health Tools Control Hunger
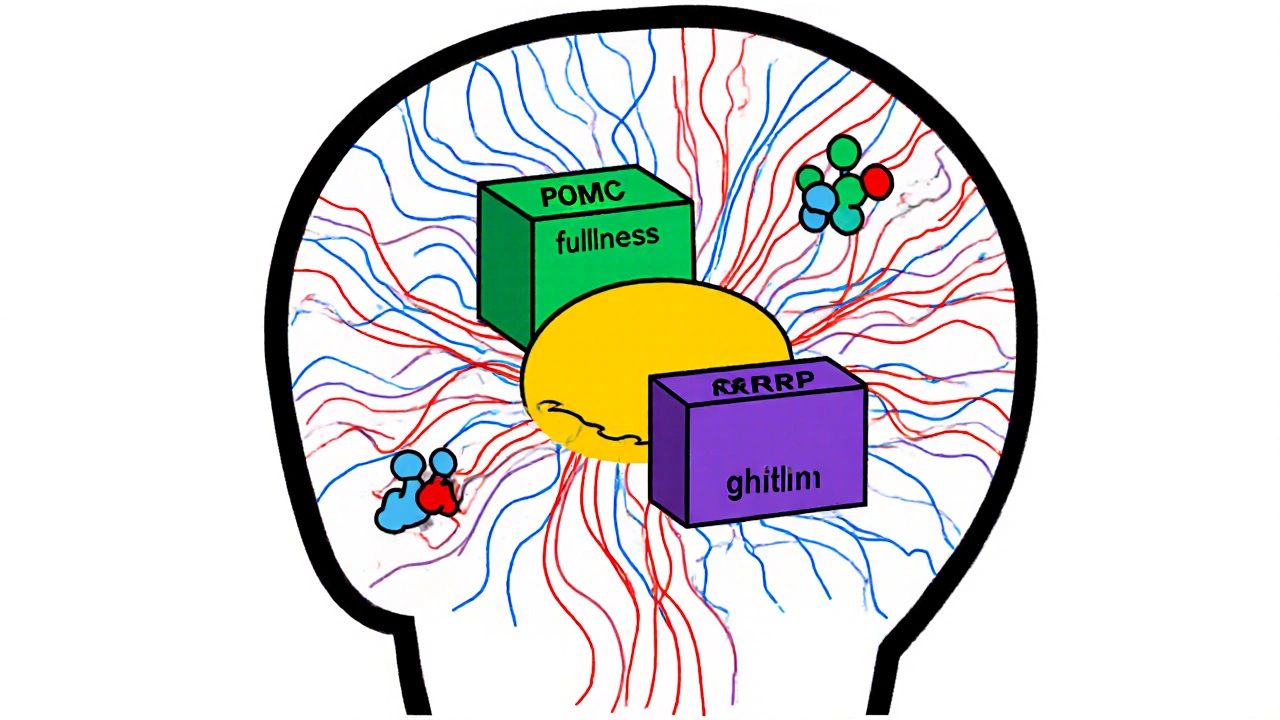
When you feel hungry or full, it’s not random—it’s your body’s appetite regulation, the biological process that controls hunger and fullness through hormones, brain signals, and nerve responses. Also known as hunger control, it’s the invisible system that decides when you eat, how much, and when to stop. This isn’t just about willpower. It’s chemistry. Hormones like ghrelin and leptin talk directly to your brain, and medications can tweak those signals to help manage weight, treat eating disorders, or support diabetes care.
Many people don’t realize that appetite suppressants, drugs designed to reduce hunger by affecting brain pathways are already part of treatment for obesity and certain metabolic conditions. Drugs like semaglutide and liraglutide, originally for diabetes, now work by slowing stomach emptying and signaling fullness to the brain. Meanwhile, metabolic health, the state of your body’s ability to process energy efficiently plays a huge role—poor insulin response, inflammation, or sleep loss can throw appetite regulation off track, making you crave carbs even when you’re not hungry.
Appetite regulation also connects to how your body handles medication side effects. Some drugs for high blood pressure, depression, or even cholesterol can increase hunger as a side effect, while others suppress it. That’s why understanding your own hunger patterns matters—not just for weight, but for safety. If you’re on a medication that changes your appetite, you need to know whether it’s normal or a sign something else is wrong. The CDC and FDA track these patterns because they affect real outcomes: people gain weight on some meds, lose muscle on others, or end up in emergency rooms from uncontrolled cravings.
What you’ll find in this collection isn’t theory. It’s real-world insight. You’ll see how medications like gemfibrozil affect bone health and appetite indirectly, how drug interactions can alter hunger signals, and why some people need to report changes in eating habits to the FDA. There’s no magic pill for appetite control—but there are smart, science-backed ways to understand and manage it. Whether you’re managing diabetes, trying to lose weight, or just wondering why you’re always hungry, the posts here give you the tools to ask the right questions—and find answers that fit your body, not just a diet trend.
Obesity is not just about eating too much-it's a disease of broken hunger signals and metabolic dysfunction. Learn how leptin resistance, brain pathways, and hormones like ghrelin and insulin drive weight gain and make weight loss so hard.