Every year, millions of people take turmeric supplements thinking they’re just adding a healthy spice to their routine. But if you’re on a blood thinner-whether it’s warfarin, aspirin, rivaroxaban, or any other anticoagulant-this common supplement could be putting you at serious risk. The problem isn’t just theoretical. Real cases have been documented where people on stable blood thinner doses ended up in the hospital after starting turmeric, their blood too thin to clot, bleeding internally with life-threatening results.
How Turmeric Acts Like a Blood Thinner
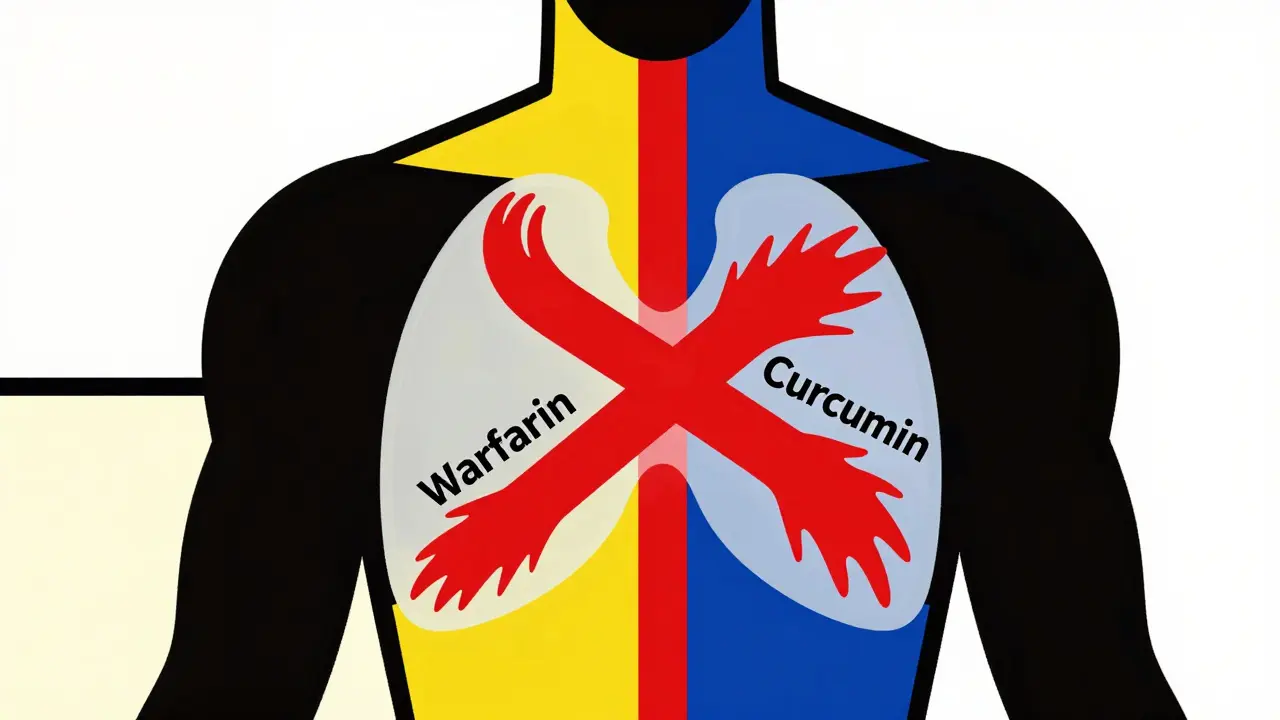
Turmeric gets its bright yellow color from curcumin, and that’s the compound doing the work. Curcumin doesn’t just give flavor to curry-it directly interferes with how your blood clots. Studies show it slows down two key steps in the clotting process: it inhibits thrombin and factor Xa, two proteins your body needs to form clots. It also makes platelets less sticky, so they don’t clump together as easily. That’s why turmeric has a dual effect: it’s both an anticoagulant and an antiplatelet agent.Here’s the catch: prescription blood thinners like warfarin or Eliquis work on similar pathways. Warfarin blocks vitamin K, which your liver needs to make clotting factors. DOACs like rivaroxaban directly block factor Xa. So when you add curcumin on top of that, you’re stacking effects. It’s not just adding one more layer-it’s doubling down on the same system your body uses to stop bleeding.
And unlike pills with exact doses, turmeric supplements vary wildly. A teaspoon of ground turmeric might have 20-40 mg of curcumin. But a capsule labeled “500 mg turmeric extract” could contain up to 95% curcumin-that’s 475 mg per pill. That’s a 10x difference in potency. No one knows exactly how much is safe when you’re already on blood thinners. And that’s the problem.
Real Cases, Real Danger
In 2018, New Zealand’s health agency, Medsafe, issued a warning based on a real patient case. A man had been on warfarin for years. His INR-a test that measures how long it takes your blood to clot-was steady at 2.5, safely in the target range. Then he started taking a turmeric supplement. Within weeks, his INR shot up to over 10. That’s more than three times the upper limit of safety. He was at high risk for spontaneous bleeding: nosebleeds that wouldn’t stop, bruising without injury, even bleeding in the brain.Another case involved a kidney transplant patient. He was taking tacrolimus, a drug to prevent organ rejection. He also took 15 spoonfuls of turmeric powder a day for ten days. His tacrolimus levels spiked to 29 ng/mL-dangerously high. His kidneys were damaged. His body couldn’t clear the drug because turmeric blocked the liver enzyme (CYP3A4) that breaks it down. This isn’t just about bleeding-it’s about multiple drug interactions piling up.
These aren’t rare outliers. The Welsh Medicines Information Centre (WMIC) updated its guidance in October 2024, confirming that curcumin can reduce how fast warfarin leaves the body. That means warfarin builds up. Even small increases in warfarin levels can be deadly because its therapeutic window is so narrow. The difference between working and poisoning is tiny.
Which Blood Thinners Are Most at Risk?
The risk isn’t the same across all blood thinners, but nearly all are affected. Here’s what the evidence shows:- Warfarin (Coumadin): Highest risk. Curcumin interferes with how warfarin is metabolized and increases its effect. INR spikes have been documented repeatedly.
- DOACs (rivaroxaban, apixaban, dabigatran): Curcumin inhibits factor Xa-the same target as rivaroxaban. Combining them may lead to excessive anticoagulation. The British Heart Foundation explicitly warns about this.
- Aspirin, clopidogrel (Plavix): These are antiplatelet drugs. Turmeric also reduces platelet clumping, so the effect is additive. Bleeding risk goes up, especially in the stomach or brain.
- NSAIDs (ibuprofen, naproxen): These already irritate the stomach lining and raise bleeding risk. Turmeric adds another layer of thinning, making ulcers and internal bleeding more likely.
- Enoxaparin (Lovenox), dalteparin (Fragmin): These injectable anticoagulants work differently, but turmeric still affects clotting factors and platelets, increasing bleeding time.
Even if you’re not on a prescription blood thinner, if you take daily aspirin for heart health, you’re still at risk. And if you’re on multiple medications-like blood pressure pills, diabetes drugs, or immunosuppressants-turmeric can mess with how your liver processes them too.
Why “Natural” Doesn’t Mean Safe
People assume that because turmeric comes from a plant, it’s harmless. That’s a dangerous myth. Many of the most dangerous drugs in history came from plants: digitalis from foxglove, morphine from poppies, vinca alkaloids from periwinkle. Nature doesn’t care if something is “natural.” It only cares about chemistry.Prescription blood thinners are tested in thousands of people over years. Their doses, interactions, and side effects are known. Turmeric supplements? They’re not regulated like drugs. There’s no standardization. One bottle might have 5% curcumin. Another might have 95%. No label tells you how much is actually in there. And there’s no FDA oversight to ensure safety or consistency.
That’s why doctors don’t say “avoid turmeric.” They say “avoid turmeric supplements.” Using a pinch of turmeric in cooking is fine. You’re not getting enough curcumin to cause harm. But popping capsules? That’s a different story. The dose matters. The form matters. And the interaction matters.
What Should You Do?
If you’re on a blood thinner, here’s what to do right now:- Stop taking turmeric supplements. Even if you feel fine. The damage can build silently.
- Talk to your doctor or pharmacist. Don’t assume they know you’re taking it. Many people don’t mention supplements unless asked directly.
- Get your INR checked. If you’re on warfarin, ask for a blood test. A sudden spike in INR could mean you’re in danger.
- Stop turmeric two weeks before any surgery. Even dental work can cause dangerous bleeding if your blood is too thin.
- Read labels carefully. Turmeric is in everything: golden milk powders, joint health blends, anti-inflammatory formulas. Check the ingredient list.
And if you’re thinking of starting turmeric for arthritis, inflammation, or “detox”-ask yourself: Is the potential benefit worth risking a stroke, a brain bleed, or internal bleeding? There are safer, proven ways to reduce inflammation: exercise, sleep, omega-3s from fish, and proven medications. Turmeric isn’t the only option.

What About Cooking With Turmeric?
If you’re using turmeric as a spice in food-like in curry, soups, or scrambled eggs-you’re fine. The amount of curcumin you get from food is tiny. You’d need to eat several tablespoons of pure turmeric powder every day to reach the levels linked to bleeding risk. That’s not realistic. The real danger comes from concentrated supplements.But even here, be cautious. If you’re on warfarin and suddenly start eating a lot of turmeric-rich dishes every day, your INR could still rise. It’s rare, but it’s possible. Consistency matters. Don’t go from no turmeric to three curries a week without telling your doctor.
What’s the Bottom Line?
Turmeric supplements and blood thinners don’t mix. The evidence is clear, consistent, and backed by real medical emergencies. This isn’t a “maybe” or a “could happen.” It’s a documented, preventable risk that’s already hurt people.If you’re on a blood thinner, skip the turmeric capsules. Don’t gamble with your life because something is labeled “natural.” Your doctor didn’t prescribe warfarin to be taken with a supplement you bought off a shelf. They prescribed it because you need precise, controlled anticoagulation. Turmeric throws that control out the window.
There’s no safe dose of turmeric supplement if you’re on blood thinners. Not yet. Not until more research is done. And until then, the only safe choice is to avoid it entirely.
