Foods and Medicine: How What You Eat Can Change Your Drugs
One glass of grapefruit juice can change how a prescription works. Food isn’t just fuel — it can speed up, slow down, or block medicine. That matters whether you take an allergy pill, diabetes drug, antibiotic, or a herbal supplement. Here are clear, practical facts you can use today.
Everyday foods that matter
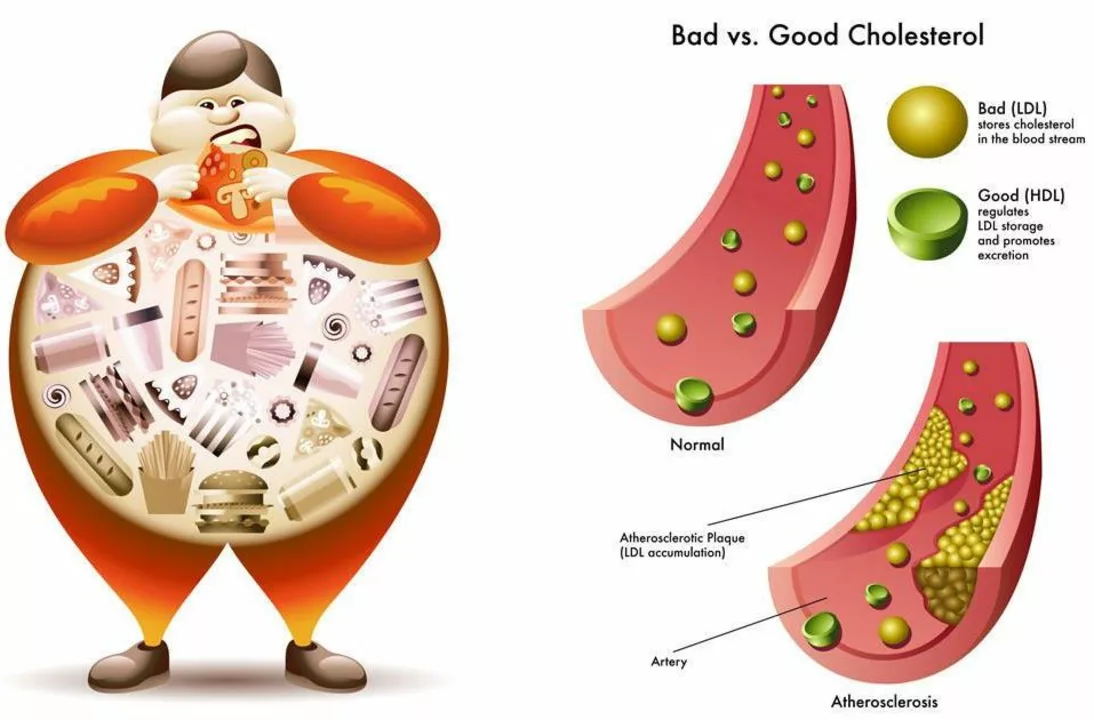
Grapefruit and grapefruit juice: these are famous for interacting with many drugs. They can raise levels of some heart and cholesterol medicines, and certain anti-anxiety or immunosuppressant drugs. If a label warns about grapefruit, don’t guess — avoid it and ask your pharmacist.
Fruit juices and some antihistamines: fruit juices like apple or grapefruit can lower the absorption of fexofenadine and a few other meds. If your allergy medicine isn’t working, try taking it with water instead of juice.
Dairy and calcium-rich foods: milk, yogurt, and supplements can bind to antibiotics such as doxycycline or ciprofloxacin and make them less effective. A simple rule: take those antibiotics 2 hours before or 4–6 hours after dairy or calcium supplements.
Leafy greens (vitamin K): if you’re on blood thinners like warfarin, eating a lot of kale or spinach can change how the drug works. You don’t need to avoid greens — just keep your intake steady and tell your doctor about big changes.
High-fiber meals: very fibrous diets can lower absorption of some thyroid medicines and certain heart drugs. Take thyroid pills on an empty stomach when recommended, usually 30–60 minutes before breakfast.
Supplements from foods: things like indole-3-carbinol (from broccoli and cabbage) or prickly pear cactus extract can affect hormones or blood sugar. If you take diabetes meds, prickly pear could add to their effect and cause low blood sugar. Treat supplements like medicines — discuss doses with a provider.
Quick, practical rules to stay safe
1) Read labels and follow timing instructions: some meds say take with food to avoid nausea, others say take on an empty stomach for best absorption.
2) Use water as your go‑to drink when taking pills. It’s the safest choice and avoids many juice-related issues.
3) Space problem combinations: when in doubt, wait 2 hours between a medication and dairy or mineral supplements like calcium, magnesium, or iron.
4) Tell your provider about all supplements and herbal products. Natural doesn’t mean harmless—prickly pear and hormone-affecting supplements can change drug effects.
5) Ask your pharmacist one quick question: “Does food affect this?” It takes seconds and can prevent real problems.
Food and meds interact in predictable ways. Keep it simple: read labels, use water, tell your healthcare team what you eat and take, and space pills around dairy or mineral supplements when needed. Small changes in timing or drink choice often fix the problem.