How the U.S. Drug Supply Chain Stops Counterfeit Medicines Before They Reach You
Every year, over 5.8 billion prescription drug packages move through the U.S. supply chain. That’s a lot of pills, injections, and patches-each one a potential target for counterfeiters. But here’s the thing: you’re far safer today than you were a decade ago. Thanks to a federal law called the Drug Supply Chain Security Act (DSCSA), the system that gets your medicine from the factory to your pharmacy is now built to catch fakes before they ever hit the shelf.
This isn’t just about stopping shady online sellers. Real counterfeit drugs-fake antibiotics, diluted cancer meds, or pills with the wrong active ingredient-can kill. In 2014, the FDA recorded over 1,100 suspected counterfeit drug incidents. By 2022, that number had dropped to 412. That’s a 63% decline. The reason? A decade-long overhaul of how drugs are tracked, verified, and authenticated at every step.
The DSCSA: A 14-Year Plan to Lock Down the Drug Supply
The DSCSA didn’t appear overnight. It was signed into law in 2013, but its full power only kicked in gradually. The goal was simple: make every prescription drug package uniquely identifiable and traceable. No more guessing where a bottle came from. No more paper trails that get lost in shipping warehouses.
By November 2023, every manufacturer, wholesaler, and pharmacy had to start exchanging electronic data about each drug package. That means when a box of insulin leaves the factory, it carries a digital fingerprint-a 2D barcode with four key pieces of info: the National Drug Code (NDC), a unique serial number, the lot number, and the expiration date. That’s not just a label. It’s a digital passport.
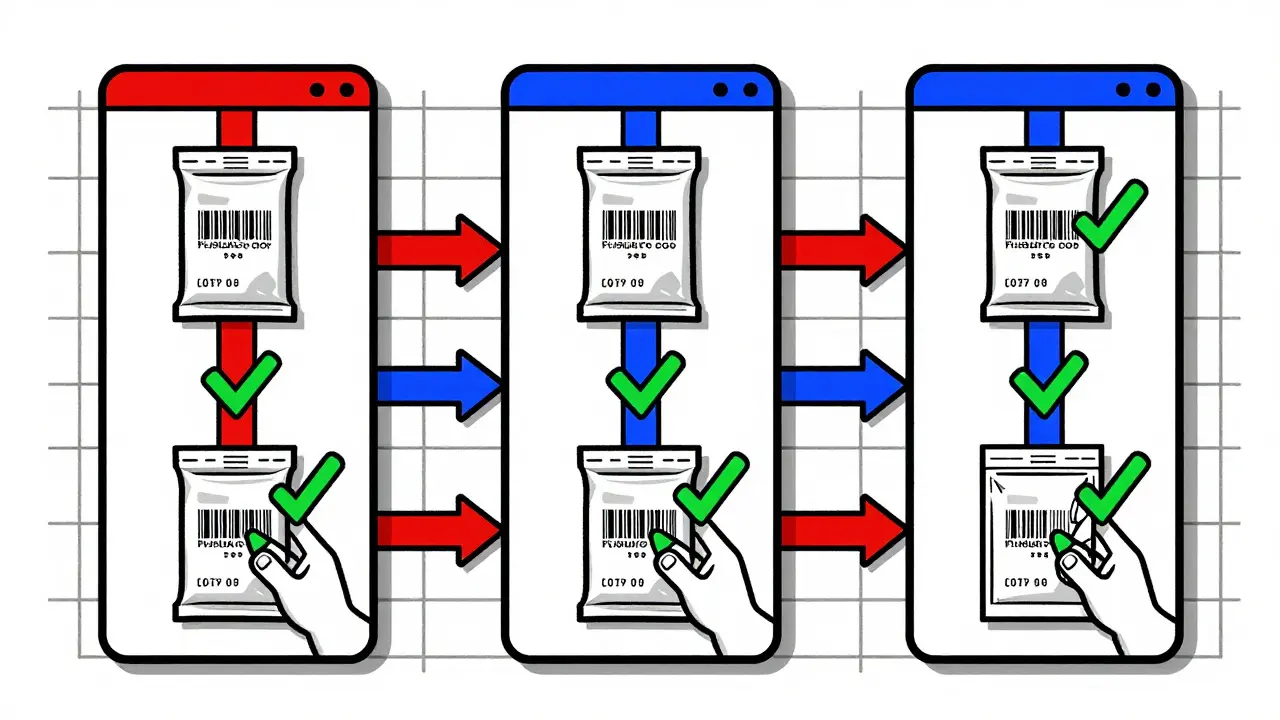
Each time that package changes hands-whether it’s moved from a distributor to a hospital or from a pharmacy’s backroom to your hands-it’s scanned. The system checks: Is this serial number real? Did it come from an authorized supplier? Has it been reported as stolen or tampered with? If something looks off, the system flags it within seconds.
How Serialization Works: One Package, One Identity
Think of serialization like giving every pill bottle its own license plate. The barcode isn’t just a random string-it’s generated using GS1 standards, the same global system used to track everything from groceries to electronics. Each code is unique. No two are the same. And every code is recorded in a secure database tied to the manufacturer.
Manufacturers print these codes on the packaging during production. Then, as the drugs move through the chain, each trading partner scans them. A wholesaler scans when they receive the shipment. A pharmacy scans when they stock the shelves. Even your local pharmacy’s automated dispenser might scan it again before handing it to you.
This system generates about 1.2 million unique identifiers every single day. And it works. In 2023, the FDA reported over 12,000 suspect product incidents were caught and quarantined before reaching patients. Most of these were traced back to unauthorized suppliers trying to slip fake or stolen drugs into the system.
But it’s not foolproof. Repackaged drugs-like those split into blister packs by pharmacies for easier dosing-are a weak spot. When the original barcode is destroyed, the new packaging must still carry a valid traceable identifier. Many small pharmacies still struggle with this, especially those using older equipment.
Authorized Trading Partners: Who’s Allowed in the Chain?
Not everyone can handle prescription drugs. The DSCSA requires every company in the supply chain to be verified as an Authorized Trading Partner (ATP). That means the FDA and industry systems check each company’s credentials before allowing them to receive or send drugs.
The ATP verification system runs behind the scenes, processing over 50,000 requests per day. If a wholesaler tries to sell to a pharmacy that’s not on the approved list, the transaction is blocked. This has shut down dozens of illegal operations that used fake paperwork to pose as legitimate distributors.
But here’s the catch: a 2022 FDA audit found only 47% of wholesale distributors were fully doing their ATP checks. Some skipped it to save time. Others didn’t realize how critical it was. That’s why enforcement is ramping up. Companies that fail to verify partners now face fines, suspension, or worse.
Technology Behind the Scenes: What Powers This System?
None of this works without the right tech. Pharmacies and distributors need barcode scanners that can read 1,200 codes per minute. Warehouse systems must track items with 0.01% error tolerance. Data must flow between companies using EPCIS 2.0, a standardized digital language for tracking goods.
Companies like TraceLink, SAP, and Movilitas built platforms to handle this. These aren’t simple apps-they’re enterprise systems that connect manufacturers, distributors, and pharmacies in real time. One pharmacy owner told Supply Chain Dive that switching to an EPCIS-compliant system cost him $18,500 a year. That’s a big hit for a small business.
But the payoff? Merck’s team cut verification time from 15 minutes to under a minute. That means fewer delays, fewer false alarms, and faster response when something goes wrong. During the 2022 infant formula crisis, this system helped remove unsafe batches from shelves in 72 hours. Before DSCSA, that would’ve taken two weeks.
Where the System Still Falls Short
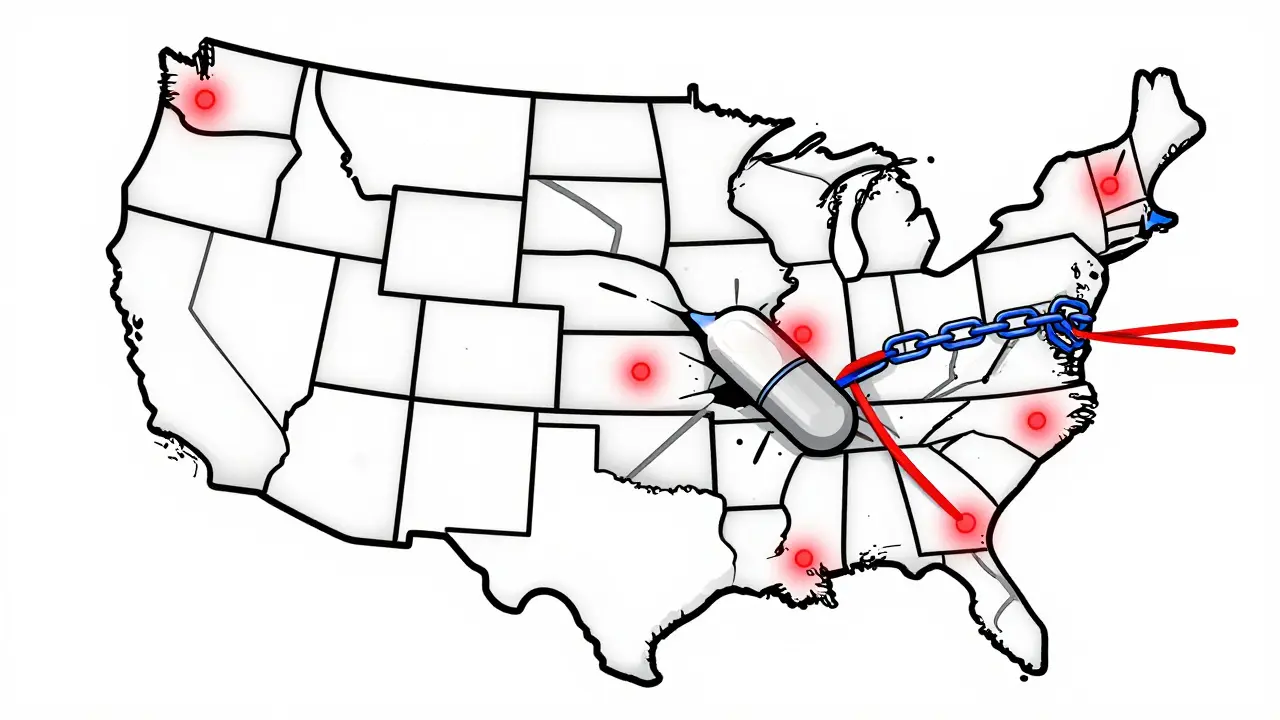
For all its strengths, DSCSA isn’t perfect. First, it only covers the U.S. The global supply chain is still a patchwork. A drug made in India, shipped through Singapore, and sold in the U.S. might not have the same tracking rules all the way. That’s a loophole counterfeiters exploit.
Second, small pharmacies are struggling. A 2023 survey found 63% of independent pharmacies with fewer than 10 employees had trouble meeting the 2023 electronic data exchange deadline. They can’t afford the $500,000+ systems that big companies use. Many are still using manual logs or outdated scanners that can’t read modern barcodes.
Third, false positives are a problem. The system flags suspicious activity-but sometimes it’s just a glitch. One pharmacist on Reddit said his system flagged legitimate packages 8.3% of the time. That means staff waste hours checking things that aren’t actually fake.
And then there’s cybersecurity. In early 2023, the Change Healthcare cyberattack knocked out DSCSA verification for 72 hours across 35% of U.S. pharmacies. Without access to the verification system, pharmacists couldn’t confirm if a drug was real. That’s a scary gap.
What’s Next: The Road to Full Interoperability by 2027
The DSCSA isn’t done. By November 2027, every single drug package must be traceable electronically across the entire chain. Paper records will be gone. Every transaction will be digital, secure, and instantly verifiable.
The FDA is pushing hard for this. In 2023, they updated rules to require all data to be in EPCIS 2.0 JSON format by 2025. That’s a big shift-most companies are still using older XML formats. The 2024 DSCSA Interoperability Pilot, involving 12 major pharma companies, is testing whether full system-wide communication is possible.
Experts predict this system will evolve into a predictive tool by 2030. Instead of just reacting to fakes, it’ll spot patterns: unusual shipping routes, abnormal temperature changes in cold-chain drugs, or sudden spikes in serial number requests. That’s when the real protection kicks in-before the fake even enters the system.
What You Can Do to Stay Safe
Even with all these safeguards, you’re not completely off the hook. Here’s how to protect yourself:
- Buy from licensed pharmacies. If a website doesn’t require a prescription or looks sketchy, walk away.
- Check your pills. If the color, shape, or taste is different from what you’re used to, ask your pharmacist.
- Report anything suspicious. The FDA has a portal to report counterfeit drugs. Your tip could stop a batch from reaching others.
- Don’t trust too-good-to-be-true prices. Legitimate drugs cost money to make. If a brand-name drug is 80% cheaper online, it’s probably fake.
The system is strong. But it’s only as good as the people using it. Your awareness matters.
How does the DSCSA prevent counterfeit drugs from entering the U.S. supply chain?
The DSCSA requires every prescription drug package to have a unique 2D barcode with a serial number, lot number, expiration date, and NDC. Every time the drug changes hands-from manufacturer to distributor to pharmacy-it’s scanned and verified against a secure database. If the serial number doesn’t match or comes from an unauthorized source, the system flags it. This stops fake drugs from being sold legally.
Are all pharmacies required to comply with DSCSA?
Yes. All dispensers-including hospitals, retail pharmacies, and mail-order pharmacies-must comply with DSCSA requirements by November 2023. However, smaller independent pharmacies often struggle with the cost and complexity of upgrading their systems. The FDA has provided guidance and support, but compliance rates are lower among small operators.
What’s the difference between DSCSA and the EU’s FMD?
The DSCSA uses a decentralized model where each company exchanges data directly with its trading partners. The EU’s Falsified Medicines Directive (FMD) uses a centralized system: every drug must be scanned and "decommissioned" at the pharmacy through a single European database. FMD also requires tamper-evident packaging, while DSCSA focuses on traceability. Both aim to stop counterfeits, but they use different tech and rules.
Can I verify if my medication is real using a smartphone app?
Not directly. The DSCSA system is designed for industry use-pharmacies and distributors verify drugs through secure, enterprise-level platforms. Consumers can’t access the database. However, if your pharmacy uses a patient-facing app that shows drug history (like some CVS or Walgreens apps), it may confirm the drug came from an authorized source. Always ask your pharmacist if you’re unsure.
Why do some drugs still get counterfeited despite DSCSA?
Counterfeiters target areas where the system is weakest: repackaged drugs, international shipments, and small pharmacies with outdated tech. Some fake drugs enter through gray-market suppliers or are smuggled in from countries without strong regulations. DSCSA works well within the U.S. chain, but global gaps remain. Also, criminals constantly adapt-so the system must keep evolving.
What happens if a fake drug gets past the system?
If a suspect product is identified, the company that discovered it must investigate within 24 hours. They check the serial number, test the product, and if confirmed fake, notify the FDA and other trading partners. The system then recalls the entire batch. Because every package is traceable, they can pinpoint exactly where it went and pull it off shelves within hours-not weeks. This speed has saved lives.
Final Thoughts: A System That Works-But Needs Everyone’s Help
The U.S. pharmaceutical supply chain is now one of the most secure in the world. The DSCSA turned a vulnerable system into a digital fortress. Counterfeit drugs haven’t disappeared-but they’re far harder to sell. The real victory? Patients can trust their meds again.
But this system doesn’t run itself. It needs pharmacies to scan, distributors to verify, manufacturers to code right, and patients to speak up. The next step isn’t just better tech-it’s better participation. Because when every link in the chain does its part, no fake drug stands a chance.

Comments (13)
Adarsh Uttral
January 30, 2026 AT 01:19
lol so now my insulin has a license plate? kinda wild. but honestly, if it keeps the fakes out, i’ll take it.
Sheila Garfield
February 1, 2026 AT 00:21
I work in a small pharmacy in Manchester and we’re still using a scanner from 2018. It beeps when it reads the barcode, but half the time it just says 'error' and we have to re-scan manually. The cost to upgrade? Not happening. We’re doing our best.
Melissa Cogswell
February 2, 2026 AT 13:22
The DSCSA is one of the most underappreciated public health wins of the last decade. Before this, counterfeit drugs were slipping through like water through a sieve. Now, every batch is traceable. It’s not perfect, but it’s a massive leap forward. The real challenge is global alignment - especially with India and China still operating on paper trails.
Blair Kelly
February 3, 2026 AT 01:39
Let’s be real - this whole system is a corporate tax write-off disguised as patient safety. Big pharma loves it because it locks out small competitors. And don’t get me started on the $500k software bills forcing independent pharmacies into oblivion. This isn’t security - it’s consolidation.
Rohit Kumar
February 4, 2026 AT 08:31
In India, we have a saying: 'The river is clean until the garbage arrives.' The DSCSA is a beautiful river - but counterfeiters are still dumping waste at the borders. The real issue isn’t technology. It’s governance. Until every country enforces the same rules, the system will always have cracks.
kate jones
February 5, 2026 AT 13:39
The EPCIS 2.0 transition is non-negotiable. Legacy XML schemas are incompatible with real-time blockchain-adjacent traceability architectures. Without standardized JSON payloads, interoperability at scale is mathematically infeasible. The FDA’s 2025 deadline is aggressive but necessary - any delay increases systemic risk exponentially.
Lisa McCluskey
February 5, 2026 AT 15:37
I’ve seen the system flag legit meds 10% of the time. It’s exhausting. We spend hours checking things that aren’t even fake. But I’d rather waste time than risk someone getting poisoned. So we keep scanning.
owori patrick
February 6, 2026 AT 10:31
This is why global health equity matters. In Lagos, we don’t have barcode scanners. We rely on trusted suppliers and patient feedback. The DSCSA works in the US, but what about the rest of the world? If we only protect the rich, we’re not solving the problem - just moving it.
Mike Rose
February 7, 2026 AT 20:03
so like... we spend billions so we can scan pills? why not just make them cheaper? also why do i care if my tylenol has a barcode? i just want it to work.
Russ Kelemen
February 8, 2026 AT 06:15
The real hero here isn’t the tech - it’s the pharmacists. The ones staying late to re-scan 300 bottles because the system glitched. The ones who call the FDA when something feels off. This system only works because people care. Don’t forget them.
April Allen
February 9, 2026 AT 07:33
The predictive analytics angle is where this gets exciting. Imagine AI detecting anomalies in shipping patterns - like a batch of insulin suddenly routed through three countries before reaching a pharmacy. That’s not just traceability - that’s prevention. The 2030 horizon isn’t science fiction. It’s logistics.
Sarah Blevins
February 10, 2026 AT 00:41
The 63% decline in counterfeit incidents is misleading. The FDA’s reporting criteria changed in 2019 to exclude unconfirmed cases. The actual number of counterfeits may have remained stable - the detection rate just improved. Transparency in metrics is essential.
Diksha Srivastava
February 10, 2026 AT 08:59
This is why I believe in systems that protect people, not just profits. Even if I’m not a pharmacist or a CEO, knowing my meds are safe makes me feel like I’m part of something bigger. Thank you to everyone keeping this chain strong.