Statin Interaction Checker
This tool helps you check whether your medications interact dangerously with statins and increase your risk of muscle damage (myopathy). Enter your statin and other medications to see if there's a risk.
Important: This tool is for educational purposes only and should not replace medical advice from your doctor.
If you have a dangerous interaction, your doctor may recommend:
- Switching to a safer statin like pravastatin or fluvastatin
- Stopping the interacting medication temporarily
- Reducing the statin dose or using intermittent dosing
Statins save lives. They’ve lowered heart attack and stroke rates for decades by cutting bad cholesterol. But for some people, they cause muscle pain so bad they stop taking them. And it’s not always the statin alone - often, it’s what’s combined with it.
Why Some Statins Are More Dangerous Than Others
Not all statins are the same. Some slip into muscle tissue more easily than others. That’s why simvastatin and lovastatin carry a much higher risk of muscle damage than pravastatin or rosuvastatin. Simvastatin is 95% broken down by the liver enzyme CYP3A4. When something blocks that enzyme - like certain antibiotics - statin levels in your blood can spike. A 10-fold increase isn’t theoretical. It’s documented. And that’s when muscle cells start breaking down. Lipophilic statins (fat-soluble) like atorvastatin, simvastatin, and lovastatin enter muscle cells more readily. Hydrophilic statins (water-soluble) like pravastatin and rosuvastatin don’t. That’s why pravastatin has a myalgia rate as low as 0.6%, while rosuvastatin can hit 12.7% in real-world use. The difference isn’t just chemistry - it’s clinical.The Top 5 Medications That Turn Statins Into a Hazard
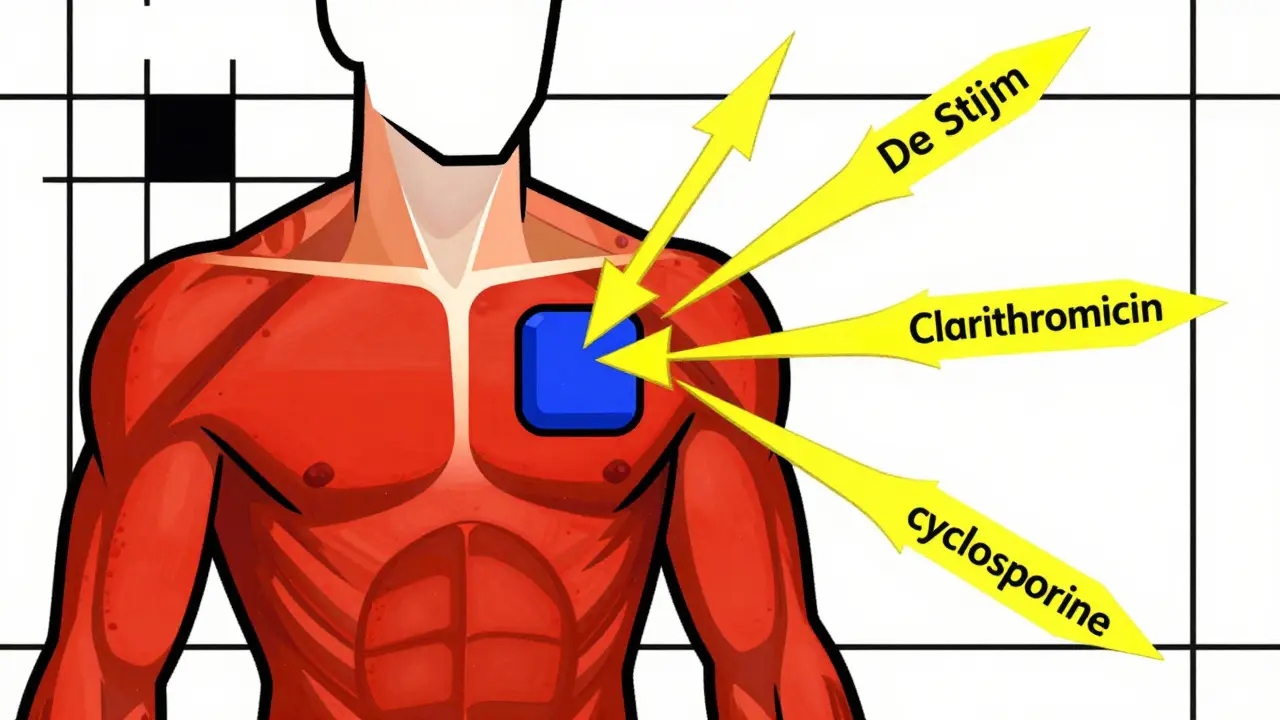
These drugs don’t just add side effects - they multiply statin toxicity.- Clarithromycin and erythromycin: These macrolide antibiotics block CYP3A4. Clarithromycin can make simvastatin levels jump 10 times. That’s why the NHS recommends stopping simvastatin entirely during these antibiotic courses. Azithromycin? Safe. It doesn’t touch CYP3A4.
- Cyclosporine: Used after transplants, this drug can increase statin levels by up to 13 times. It’s one of the most dangerous combinations. Even low-dose statins become risky.
- Gemfibrozil: This fibrate increases statin levels by 2-fold. It also interferes with muscle repair. The FDA added a black box warning for this combo in 2010. Fenofibrate? Much safer.
- Diltiazem and verapamil: These calcium channel blockers, used for high blood pressure and heart rhythm, inhibit the same liver pathway. The FDA now limits simvastatin to 20mg max when taken with these drugs.
- Niacin: Often paired with statins to boost HDL, niacin increases muscle toxicity risk. Many doctors now avoid combining them unless absolutely necessary.
Who’s Most at Risk - Beyond the Drugs
It’s not just about what you’re taking. Your body matters too.- Age 75+: Older adults clear drugs slower. Their muscles are more vulnerable.
- Small frame or low BMI: Less muscle mass means higher drug concentration per pound of tissue.
- Chronic kidney disease: Impaired clearance = higher statin exposure.
- Hypothyroidism: Low thyroid function slows metabolism of statins.
- Alcohol abuse: Damages liver function and muscle tissue - a double hit.
- Intense exercise: Muscle stress + statin = higher risk of breakdown.

What to Do If Your Muscles Start Aching
Muscle pain isn’t always a sign of danger - but it shouldn’t be ignored.- Don’t assume it’s just aging. Muscle weakness, cramps, or unexplained soreness that doesn’t go away after a few days? Get it checked.
- Get a creatine kinase (CK) blood test. Levels over 10 times the upper limit mean myopathy. Levels over 5 times with symptoms? That’s a red flag.
- Stop the statin if CK is high and symptoms are present. Restarting too soon can cause rhabdomyolysis - a life-threatening condition where muscle breaks down and floods your kidneys with toxic proteins.
- Ask your doctor about switching to pravastatin or fluvastatin. Many patients who quit simvastatin due to muscle pain tolerate these just fine.
When to Avoid Statins Altogether - and What to Use Instead
Some people just can’t take statins. That doesn’t mean they’re out of options.- Bempedoic acid (Nexletol): Approved in 2020, this drug lowers LDL without entering muscle cells. It’s not a statin, so it avoids myopathy. But it costs over $4,000 a year - versus $6.60 for generic atorvastatin.
- Ezetimibe: Works in the gut to block cholesterol absorption. Often paired with low-dose statins to reduce the statin dose needed.
- PCSK9 inhibitors (alirocumab, evolocumab): Injectable biologics that slash LDL by 60%. Used for very high-risk patients. Costly, but covered by insurance for qualifying cases.
- Icosapent ethyl (Vascepa): A purified fish oil. Proven to reduce heart attacks and strokes in statin-treated patients. May allow lower statin doses.
What Doctors Should Be Doing - And What They Often Skip
Many primary care doctors don’t screen for drug interactions before prescribing statins. That’s a gap.- Check for interacting meds before starting any statin. Use tools like Lexicomp or Micromedex.
- Test CK before starting - and again if muscle symptoms appear.
- For high-risk patients, start with pravastatin or fluvastatin at low doses.
- Don’t just tell patients to “take it with food.” That doesn’t fix a CYP3A4 interaction.
- For short-term antibiotics like clarithromycin, pause the statin - don’t just reduce the dose.
What’s Changing - And What’s Coming
Science is catching up.- Genetic testing for SLCO1B1 variants can predict who’s at higher risk for simvastatin myopathy. The FDA added this to the label in 2011. But most doctors don’t order it.
- Intermittent dosing (e.g., rosuvastatin every other day) is being tested in the 2023 DECLARE trial. Early data suggests it keeps LDL low while cutting muscle side effects.
- Coenzyme Q10 supplements are recommended by the European Society of Cardiology for muscle symptoms. Evidence is mixed, but many patients report feeling better.
- Newer statins like pitavastatin are emerging with lower interaction potential - but they’re not widely used yet.
Can I take statins with antibiotics?
It depends on the antibiotic. Avoid clarithromycin and erythromycin with simvastatin or lovastatin - they can cause dangerous muscle damage. Azithromycin is safe. If you need a macrolide, ask your doctor to switch your statin to pravastatin or fluvastatin temporarily.
What’s the safest statin for muscle pain?
Pravastatin has the lowest reported rate of muscle symptoms - around 0.6% to 1.4%. Fluvastatin and rosuvastatin (at 20mg or less) are also safer options. Avoid simvastatin and lovastatin if you’ve had muscle pain before.
Does muscle pain from statins go away on its own?
Sometimes, yes - especially if you lower the dose or switch statins. But if pain is severe, persistent, or accompanied by weakness or dark urine, don’t wait. Get a CK test. Rhabdomyolysis can develop silently.
Is it safe to take CoQ10 with statins?
Yes. CoQ10 is safe and may help some people with muscle discomfort, though studies aren’t conclusive. Many patients report feeling better. It’s worth trying at 100-200mg daily if you’re on a statin and have muscle symptoms.
Can I restart a statin after stopping for muscle pain?
Many can - but not the same one. About 71% of people who stopped statins due to muscle pain can tolerate a different statin at a lower dose. Try pravastatin, fluvastatin, or low-dose rosuvastatin. Never restart simvastatin or lovastatin after muscle symptoms unless under strict monitoring.
Are there statin alternatives without muscle side effects?
Yes. Bempedoic acid (Nexletol) doesn’t enter muscle tissue, so it avoids myopathy. Ezetimibe and PCSK9 inhibitors are also options. They’re more expensive, but for those who can’t tolerate statins, they’re life-saving alternatives.
Comments (9)
Wesley Pereira
January 5, 2026 AT 19:39
So let me get this straight - we’re telling people to avoid simvastatin like it’s a cursed amulet because some dumbass doc didn’t check for clarithromycin? CYP3A4 isn’t exactly a secret pathway, folks. I’ve seen patients on 80mg simva + macrolide and then wonder why their legs feel like wet noodles. The FDA’s been screaming about this since 2010. It’s not a ‘risk,’ it’s a goddamn textbook case of iatrogenic myopathy waiting to happen.
And don’t even get me started on niacin. ‘Boosts HDL’ my ass. It’s a glorified flush pill that makes your skin look like you got into a fight with a toaster. No one should be on that combo unless they’re paying out of pocket for a VIP ticket to rhabdo city.
Molly McLane
January 6, 2026 AT 19:38
As someone who’s been on statins for 12 years and switched from simvastatin to pravastatin after my CK spiked to 5x, I can say this: it’s not about avoiding statins - it’s about matching the right one to your body. I used to think muscle pain was just ‘getting older.’ Nope. It was the drug. Pravastatin? Zero issues. My doctor didn’t even know about the CYP3A4 thing until I brought up the antibiotic interaction. We need better patient education - not just doctor education.
Also, CoQ10? I started taking 200mg daily after reading this thread. My cramps dropped by 70%. Not magic, but it helped. Worth a shot if you’re struggling.
Isaac Jules
January 8, 2026 AT 12:10
LOL. You people are acting like statins are poison. 99% of you are just too lazy to exercise or eat real food. My grandpa was on simvastatin 80mg for 15 years, never had a problem. You want to blame the drug? Fine. But don’t blame the drug because you won’t walk 10 minutes a day. The real problem is laziness wrapped in a lab coat.
And CoQ10? That’s just placebo with a price tag. Buy a banana instead. It’s cheaper and you’ll feel better.
Pavan Vora
January 9, 2026 AT 11:51
Thank you for this post, truly. I am from India, and here, many doctors still prescribe simvastatin as first-line, even for elderly patients with kidney issues. I had a friend who developed severe myopathy after taking simvastatin with diltiazem - he was hospitalized for two weeks. We didn’t even know these interactions existed! Now I share this post with everyone I know. Please, doctors - check the interactions! It’s not hard. There are apps for this. Thank you again.
Kelly Beck
January 10, 2026 AT 04:41
Okay, I just read this whole thing and I’m crying 😭 - not because I’m sad, but because this is the kind of info that saves lives. I’m so tired of people saying ‘statins are dangerous’ without understanding the context. This isn’t fear-mongering - it’s precision medicine. 💪❤️
Pravastatin for the win! I switched from atorvastatin after muscle pain and now I’m running 5Ks again. Also, CoQ10? Yes, please. I take it with my morning coffee and I swear I feel more energy. Not a miracle, but a gift. And if you’re on clarithromycin? Pause the statin. Period. No excuses. Your muscles will thank you.
Also, bempedoic acid? I didn’t even know it existed until now. $4000 a year? Oof. But if insurance covers it? Game-changer. We need this to be cheaper. Like, NOW.
And Katie - you’re right, we need to stop treating muscle pain as ‘just aging.’ It’s not. It’s a signal. Listen to your body. And if your doctor brushes you off? Get a second opinion. You deserve better.
Also, I just told my mom to read this. She’s 76 and on simvastatin. She’s switching tomorrow. 🙌
Katie Schoen
January 12, 2026 AT 00:18
Wait - so you’re telling me azithromycin is safe but clarithromycin is basically a statin bomb? That’s wild. I just got prescribed azithro for a sinus thing and I was worried. Now I’m not. Also, why isn’t this on every pharmacy label? Like, should we be getting pop-ups when we fill a statin script? ‘Hey, you’re on simva + this antibiotic. Don’t be an idiot.’
Also, I’ve been on rosuvastatin for 3 years. No muscle pain. But I also don’t drink, I’m not overweight, and I don’t run marathons. Maybe the ‘risk factors’ list should be called ‘things you’re doing wrong.’
Tiffany Adjei - Opong
January 12, 2026 AT 00:33
Okay but let’s be real - this whole ‘pravastatin is safer’ thing is just marketing. Rosuvastatin has a 12.7% myalgia rate? That’s because people are taking 40mg. At 10mg? It’s fine. And simvastatin 80mg? Yeah, that’s a death trap. But 20mg? Totally fine. Stop cherry-picking numbers. Also, CoQ10? The only reason people ‘feel better’ is because they believe in it. Placebo effect is real, folks.
And bempedoic acid? It’s literally just a statin that doesn’t work as well. You’re paying $4000 to get 20% less LDL reduction. That’s not innovation - that’s corporate greed.
Also, ‘genetic testing for SLCO1B1’? Who’s got time for that? My PCP doesn’t even know what that is. So stop pretending this is accessible.
Ryan Barr
January 14, 2026 AT 00:24
Simvastatin 80mg = avoid. Clarithromycin + statin = avoid. Pravastatin = safe. Done.
Cam Jane
January 15, 2026 AT 18:10
I’m a nurse practitioner and I see this every week. Patients come in saying, ‘I can’t take statins - my legs ache.’ We switch them to pravastatin or fluvastatin - boom, problem solved. No more pain. No more stopping meds. But here’s the kicker: most of them never got tested for CK. They just assumed it was the statin. And their doctor didn’t push back.
Also - I love that you mentioned intermittent dosing. I’ve started prescribing rosuvastatin every other day for older patients with mild muscle symptoms. LDL still drops 40%. Muscle pain? Gone. It’s not in the guidelines yet, but it’s working.
And CoQ10? I recommend it. Not because it’s proven, but because it’s safe and people feel better. If someone’s spending $20 a month on supplements to avoid a $4000 drug? That’s a win.
And for the love of god - if you’re on gemfibrozil with a statin, stop. Now. I’ve seen two cases of rhabdo from that combo. Both patients ended up in the ICU. It’s not a ‘maybe.’ It’s a ‘never.’
Finally - if you’re 75+, have kidney disease, and are on simvastatin? You’re playing Russian roulette. Switch. Today. Your muscles will thank you tomorrow.