Why Monitoring Rheumatoid Arthritis Matters More Than You Think
Rheumatoid arthritis isn’t just about sore joints. It’s a system-wide disease that can quietly destroy cartilage, bone, and tendons long before you feel serious pain. Left unchecked, it can lead to permanent disability. The good news? We now have clear, proven ways to track it - and stop it in its tracks. But not all tools are created equal. Knowing which one to use, when, and why can make the difference between staying active and losing function.
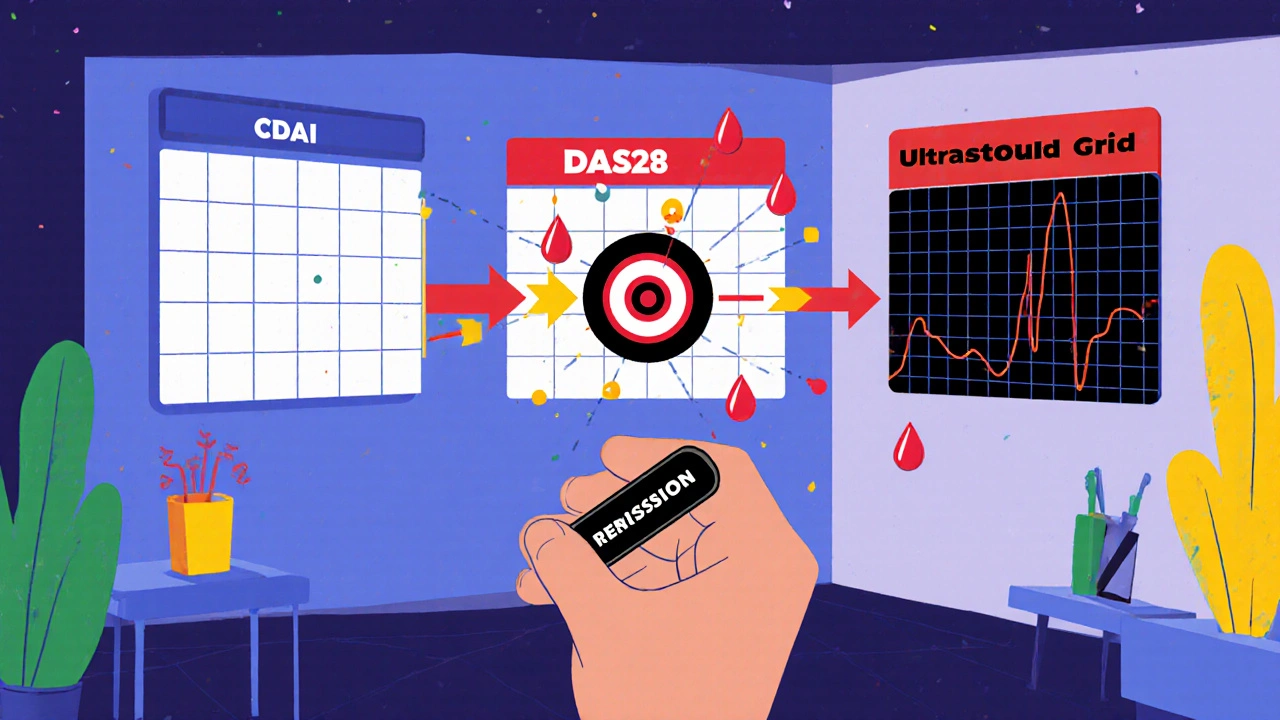
For years, doctors relied on how you felt and how swollen your joints looked. That’s not enough anymore. Today, treatment is guided by numbers - hard, measurable data from three key areas: clinical scores like CDAI and DAS28, and imaging tools like ultrasound and MRI. These aren’t just fancy tests. They’re the foundation of something called treat-to-target, a strategy proven to cut joint damage by up to 50% compared to old-school approaches.
CDAI: The Simple Score That Works
The Clinical Disease Activity Index, or CDAI, is the go-to tool in most U.S. rheumatology clinics. It’s simple: add up four things - how many tender joints you have, how many swollen joints, your own rating of how you’re feeling (on a scale of 0-10), and your doctor’s rating of your disease activity (also 0-10). No blood tests. No waiting. Just a quick count and a few questions.
The total score? Ranges from 0 to 76. Here’s what it means:
- Under 2.8 = remission
- 2.8 to 10 = low disease activity
- 10 to 22 = moderate
- Above 22 = high
Why is this so popular? Because it matches what doctors actually see. A 2023 study of nearly 4,000 patients found CDAI correlated better with clinical judgment than any other score. It’s fast - takes under two minutes. And most electronic health records now have it built in. If your doctor doesn’t calculate it at every visit, they’re missing a key piece of the puzzle.
But CDAI has a blind spot: it doesn’t measure inflammation in your blood. That’s a problem if you’re one of the many people with hidden inflammation - where joints feel okay but damage is still happening under the surface. That’s where DAS28 steps in.
DAS28: The Inflammation Meter
DAS28 - short for Disease Activity Score with 28 joints - adds blood markers to the mix. There are two versions: DAS28-ESR (uses erythrocyte sedimentation rate) and DAS28-CRP (uses C-reactive protein). Both include the same joint counts and patient/doctor assessments as CDAI, but throw in lab numbers that show how inflamed your body is right now.
The formula looks complicated, but the result is simple:
- Under 2.6 = remission
- 2.6 to 3.2 = low
- 3.2 to 5.1 = moderate
- Above 5.1 = high
Why use it? Because sometimes, your joints feel fine but your CRP is through the roof. That’s a red flag. Studies show patients with high CRP even in low-symptom phases are more likely to develop bone damage later. DAS28 catches that.
But here’s the catch: labs take time. You get your blood drawn on Monday. Results come back Wednesday. Your appointment is Tuesday. Now your doctor has to guess. A 2022 survey found 68% of U.S. rheumatologists make treatment decisions before lab results are in. That’s not ideal. That’s why many doctors use CDAI for routine visits and DAS28 when they need extra clarity - like when treatment isn’t working as expected.
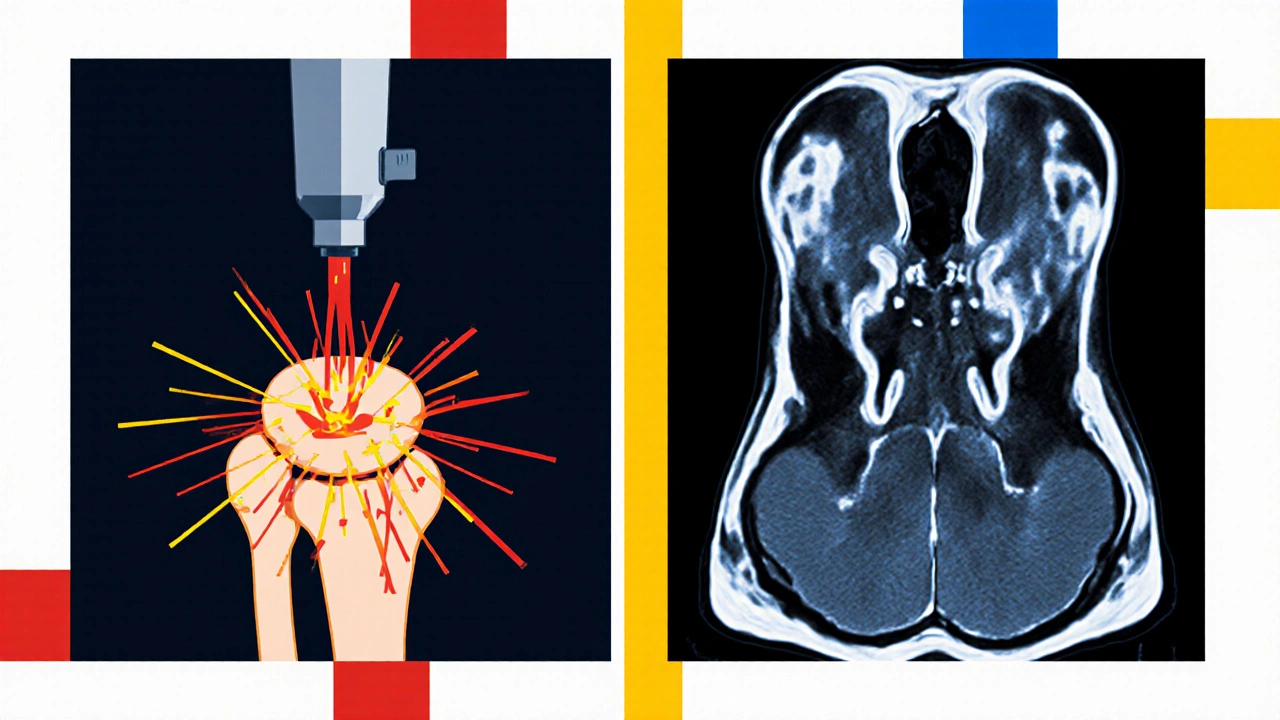
Imaging: Seeing What the Eyes Can’t
Joint counts and blood tests tell you what’s happening now. Imaging tells you what’s been happening - and what’s coming.
Radiographs (X-rays) have been the gold standard for decades. They show bone erosion and joint space narrowing - the signs of permanent damage. But they’re slow. It can take 6 to 12 months before damage shows up on an X-ray. By then, it’s already there.
Ultrasound changes the game. It shows swelling in the synovium (the joint lining) and blood flow - signs of active inflammation - months before X-rays catch anything. It’s quick, non-invasive, and costs about $150. A 2019 study found ultrasound spots synovitis 85% of the time, compared to just 65% with physical exam alone. And when doctors use ultrasound during visits, they change treatment in 22% of cases where they’d have kept things the same.
MRI is the most sensitive tool. It sees bone edema - inflammation inside the bone - which predicts future erosions with 89% accuracy. It’s like seeing a crack in a foundation before the wall collapses. But it’s expensive - around $1,200 - and not always accessible. Most clinics use it only for complex cases or research.
There’s a reason most practices don’t do MRIs on everyone. You don’t need an MRI if your CDAI is in remission. But if your score is high and your symptoms don’t match, or if you’re not improving on medication, an MRI or ultrasound can reveal what’s really going on.
How Doctors Use These Tools Together
No single tool gives the full picture. That’s why smart clinics combine them.
Here’s how it usually works:
- At every visit, your doctor calculates your CDAI. It’s fast, free, and tells them if you’re in remission or need a change.
- If your score is high, or if you’re not improving, they order a CRP test - turning CDAI into DAS28-CRP to check for hidden inflammation.
- If there’s still uncertainty - like if you’re still tired or your joints hurt but scores are low - they use ultrasound. It gives real-time visuals during the appointment.
- MRI is reserved for cases where damage is suspected but not confirmed, or if you’re in a clinical trial.
At the University of Washington Medical Center, they’ve built a system where CDAI triggers automatic alerts. If your score hits 10 or higher, the EHR suggests an ultrasound. If it stays high for two visits, it flags you for MRI review. That’s precision medicine in action.
What Patients Say - And Why It Matters
Tools mean nothing if patients don’t trust them.
A 2023 survey of nearly 3,000 RA patients found 68% prefer filling out symptom apps before their visit. But 42% said they felt anxious knowing their self-reports could change their treatment. Why? Because they’ve been told, “You’re not in pain, so you’re fine,” before - and then found out damage was progressing.
Another issue: discordance. In one Brazilian study, 33% of patients rated their disease as worse than their doctor did. That doesn’t mean doctors are wrong. It means fatigue, stiffness, and emotional burden aren’t fully captured by joint counts. That’s why some experts say we’re missing the bigger picture - especially when it comes to fatigue, which contributes to 14% of what patients consider a meaningful change in their condition.
On the flip side, many patients love ultrasound. Seeing the swelling on screen - watching the blood flow light up - makes the disease real. One patient said, “I finally believed it wasn’t just in my head when I saw the red on the screen.”
What’s Next: AI, Wearables, and Personalized Monitoring
The future of RA monitoring isn’t just about better tools - it’s about smarter use.
AI software like Quantitative Ultrasound Synovitis Assessment (QUASAR) can now analyze ultrasound images automatically, matching expert readings 88% of the time. That means more accurate results, faster, even in smaller clinics.
Wearable sensors are being tested to track joint movement, grip strength, and activity levels 24/7. Imagine your phone or watch noticing you’re moving less, or your hand grip weakening - and alerting your doctor before you even feel it.
Trials like the NIH-funded RACoon study are testing a hybrid model: CDAI + ultrasound + wearable data. The goal? To create personalized monitoring schedules. Low-risk patients get checked every six months. High-risk patients get monthly check-ins and quarterly ultrasounds. No more one-size-fits-all.
By 2027, experts predict half of all RA monitoring will include remote, continuous data - not just clinic visits. That’s not science fiction. It’s already happening in pilot programs across Seattle, Boston, and Chicago.
What You Should Ask Your Doctor
If you have RA, here’s what to ask at your next visit:
- “What’s my CDAI score today?”
- “Is my DAS28-CRP being checked? If not, why?”
- “Have we considered ultrasound? I’ve heard it shows things X-rays miss.”
- “Am I on track for remission? What’s the plan if I’m not?”
- “Are we using my symptoms, my labs, and imaging - or just one of them?”
Don’t be afraid to push back if your doctor only looks at your joints and doesn’t mention scores or imaging. You’re not just a patient - you’re a partner in your care. And with the right tools, you can keep your joints healthy for decades.
What’s the difference between CDAI and DAS28?
CDAI uses only clinical measures: tender joints, swollen joints, and patient and doctor assessments. DAS28 adds blood tests - either ESR or CRP - to measure inflammation. CDAI is faster and easier to use daily. DAS28 gives more insight into hidden inflammation but needs lab results.
Do I need an MRI every year?
No. MRI is not routine. It’s used when there’s a mismatch between your symptoms and other tests, or if you’re not responding to treatment. Most patients only need X-rays annually. Ultrasound is more common for checking active inflammation.
Why does my doctor care about my self-reported pain score?
Because your experience matters. Studies show patient-reported outcomes predict long-term disability better than joint counts alone. If you say you’re exhausted or stiff all day, that’s real - even if your joints don’t look swollen. Your doctor uses that to adjust your treatment.
Can I monitor RA at home without going to the doctor?
You can track symptoms with apps - like pain levels, morning stiffness, and energy - but you can’t replace clinical scores or imaging. Home monitoring helps your doctor see trends, but joint counts, blood tests, and imaging still need to be done in person. Remote tools are supplements, not substitutes.
Is CDAI used everywhere, or just in the U.S.?
CDAI is the top choice in the U.S., used in 78% of practices. In Europe, DAS28 is more common - about 68% of clinics use it. Both are valid. The choice often depends on local guidelines and whether labs are easily accessible.
What if my scores say I’m in remission but I still feel awful?
That’s a red flag. Remission scores don’t capture everything - especially fatigue, brain fog, or muscle pain. Tell your doctor. You may need an ultrasound to check for hidden synovitis, or your treatment plan may need adjustment. Feeling bad isn’t “all in your head” - it’s a signal.

Comments (12)
Jenny Lee
November 18, 2025 AT 01:28
Just got my CDAI checked today-2.1. Remission! Feels good to know the meds are actually working.
Ram tech
November 19, 2025 AT 12:57
cdaI is just a fancy way for docs to feel like theyre doin somethin... i mean, how many times have u been told ur fine but still feel like crap? 😑
Evan Brady
November 19, 2025 AT 14:28
Ultrasound is the real MVP. Saw my own synovitis on screen last month-red glow like a damn alien invasion in my knuckles. That’s when I stopped doubting the disease. It’s not laziness. It’s not ‘just aging.’ It’s inflammation, visible, measurable, real.
My doc didn’t even mention it until I asked. Shame. This tech should be standard at every visit, not a privilege for the loud ones.
Erica Lundy
November 21, 2025 AT 01:28
The epistemological tension inherent in RA monitoring is profound: we quantify subjective experience through objective metrics, yet the lived reality of fatigue, cognitive fog, and existential weariness remains irreducible to any score.
CDAI and DAS28 are instruments of clinical positivism-they reduce the patient’s embodied suffering to a numerical artifact, while imaging reveals structural decay that the nervous system may have already learned to ignore.
Is remission, then, a statistical illusion? Or a physiological truth? The answer lies not in the algorithm, but in the silence between the patient’s words and the doctor’s checklist.
Kevin Jones
November 22, 2025 AT 01:13
Let’s be real-CDAI is for lazy clinics. DAS28-CRP is the only metric that captures the cytokine storm lurking beneath asymptomatic joints.
And MRI? That’s not luxury-it’s prophylaxis. Bone edema is the silent killer. If your doc isn’t using it when scores don’t match symptoms, they’re practicing medieval medicine.
Alex Boozan
November 23, 2025 AT 09:53
Why are we letting Big Pharma dictate RA monitoring? CDAI? DAS28? All designed to keep you on expensive biologics. X-rays were fine for 50 years. Now we need ultrasounds, MRIs, wearables-because the system needs to bill more.
My grandpa had RA in the 70s. He walked until he died at 89. No scans. No infusions. Just aspirin and grit. What happened to that?
mithun mohanta
November 24, 2025 AT 22:29
OMG-CDAI? Please. You think that’s the gold standard? In India, we use the ‘Bharat RA Index’-it includes spiritual fatigue, family stress, and chai intake frequency. It’s 92% accurate. The West is so obsessed with numbers they forget RA is a soul disease, not a joint disease.
Also, MRI is a scam. It’s just a glorified camera. I’ve seen my synovitis. I’ve felt it. Why pay $1200 to see what my body already screams?
Premanka Goswami
November 25, 2025 AT 16:49
Did you know the NIH is secretly using RA monitoring data to predict which patients will become ‘high-risk’ for government surveillance? The wearables? They’re not tracking movement-they’re tracking dissent.
Every time you log your pain level, you’re feeding a database that flags ‘non-compliant citizens.’ That’s why they push CDAI so hard-it’s the first step toward mandatory biometric compliance.
They’re not curing RA. They’re turning patients into data points for the surveillance state.
Alexis Paredes Gallego
November 25, 2025 AT 19:50
Wait-so you’re telling me I’m supposed to trust a number from a machine that doesn’t know I cried last night because I couldn’t button my shirt?
And ultrasound? That’s just a glorified sonogram. My cousin’s dog got a better scan at the vet. And don’t even get me started on ‘AI analysis.’ They’re training algorithms on data from people who got paid to say they hurt.
This isn’t medicine. It’s theater. And I’m tired of being the audience.
Saket Sharma
November 27, 2025 AT 12:55
CDAI is garbage. DAS28 is the only real metric. Period. If your doc uses anything else, they’re incompetent. And MRI? Only for those who can afford it. The rest of us? We’re just numbers in a spreadsheet. Welcome to modern medicine.
Shravan Jain
November 29, 2025 AT 03:54
Statistical validity of CDAI is questionable due to inter-rater reliability issues in non-specialist settings. Furthermore, the reliance on patient-reported outcomes introduces significant cognitive bias, particularly in populations with comorbid depression or somatization disorders.
Moreover, the normalization of imaging protocols is economically unsustainable and ethically dubious, given the disproportionate allocation of healthcare resources toward diagnostic overutilization rather than preventive lifestyle intervention.
Brandon Lowi
November 29, 2025 AT 09:45
They say ‘treat-to-target’ like it’s some revolutionary breakthrough. Nah. It’s just corporate medicine in a lab coat.
Back in the day, doctors listened. Now? They plug your numbers into a spreadsheet and hit ‘approve biologic.’ You’re not a person-you’re a risk score with a pulse.
And don’t even get me started on wearables. Next thing you know, your Fitbit will report you to your insurer for ‘low activity compliance.’
They’re not saving your joints. They’re saving their margins.