For millions of people with type 2 diabetes, the idea of getting off medication isn’t just a dream-it’s a real possibility. But it’s not about magic pills or quick fixes. It’s about weight loss, sustained lifestyle changes, and understanding what remission really means. And yes, it’s possible-even if your doctor has told you this disease is lifelong.
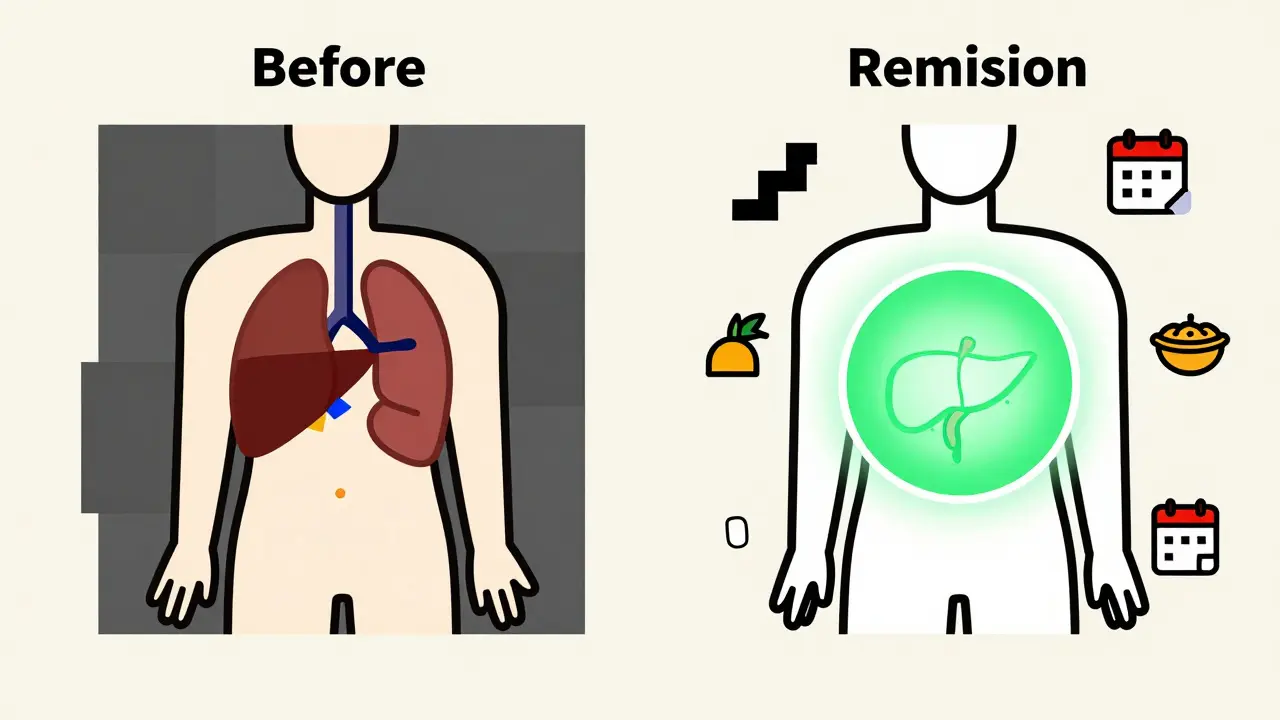
What Does Remission Actually Mean?
Remission in type 2 diabetes isn’t a cure. It doesn’t mean your body suddenly stopped being insulin resistant or that your pancreas is back to full strength. It means your blood sugar has stayed normal for at least three months without any diabetes medications. That’s the official definition set by the American Diabetes Association, the European Association for the Study of Diabetes, and other major health groups in 2021.The key number is HbA1c below 6.5% (or 48 mmol/mol). That’s the average blood sugar over the past 2-3 months. If you’ve been taking metformin, sulfonylureas, or even insulin-and now your HbA1c is below that mark for three months straight, with no meds-then you’re in remission. Not cured. Not reversed. In remission.
And here’s the catch: if you’re still on medication, even if your HbA1c is perfect, you’re not considered in remission. The definition is strict. It’s designed to show that your body is managing blood sugar on its own now. That’s huge.
How Much Weight Do You Need to Lose?
Weight loss is the most powerful tool we have for triggering remission. Not a little loss. Not 5 pounds. We’re talking about losing at least 10 kilograms (about 22 pounds), and often more.The DiRECT trial, one of the most important studies on this topic, showed that 46% of participants who lost 10 kg or more went into remission after one year. That’s nearly half. And those who lost 15 kg or more? Over 80% went into remission. These aren’t outliers. These are people just like you-living with type 2 diabetes, trying to manage it, and then making a shift.
It’s not just about the number on the scale. It’s about fat around the liver and pancreas. When you lose weight, especially visceral fat, you reduce the fat that’s clogging up your pancreas. That’s what lets insulin-producing beta cells start working again. It’s not a miracle. It’s biology.
Who Has the Best Chance?
Not everyone has the same odds. Some people are more likely to reach remission than others. If you’ve had type 2 diabetes for less than five years, your chances are much higher. The longer you’ve had it, the more damage your pancreas may have taken.People who aren’t on insulin also have better odds. Insulin use usually means your body has lost a lot of its ability to make insulin naturally. That’s harder to recover. Those with lower starting HbA1c levels-say, below 8%-also have a better shot.
Age doesn’t rule you out. Neither does BMI. Even people with a BMI under 30 have gone into remission, as long as they lost enough weight relative to their starting point. It’s not about being "obese." It’s about losing enough fat to unblock your pancreas.
What Happens After You Stop Medication?
Stopping meds isn’t the finish line. It’s the start of a new phase. Many people see their HbA1c creep back up after a year or two. The DiRECT study found that remission dropped from 46% at one year to 36% at two years. That’s still better than most people expect-but it shows how hard it is to keep the weight off.That’s why remission requires lifelong maintenance. You can’t go back to your old eating habits, even if you feel fine. Your body still has the same underlying tendency toward insulin resistance. It’s just quiet right now. The moment you gain back the weight, the diabetes can come roaring back.
That’s why doctors recommend annual HbA1c checks even after remission. You still need to see your provider. You still need to monitor your blood pressure, cholesterol, and kidney function. Diabetes complications don’t disappear just because your blood sugar is normal.
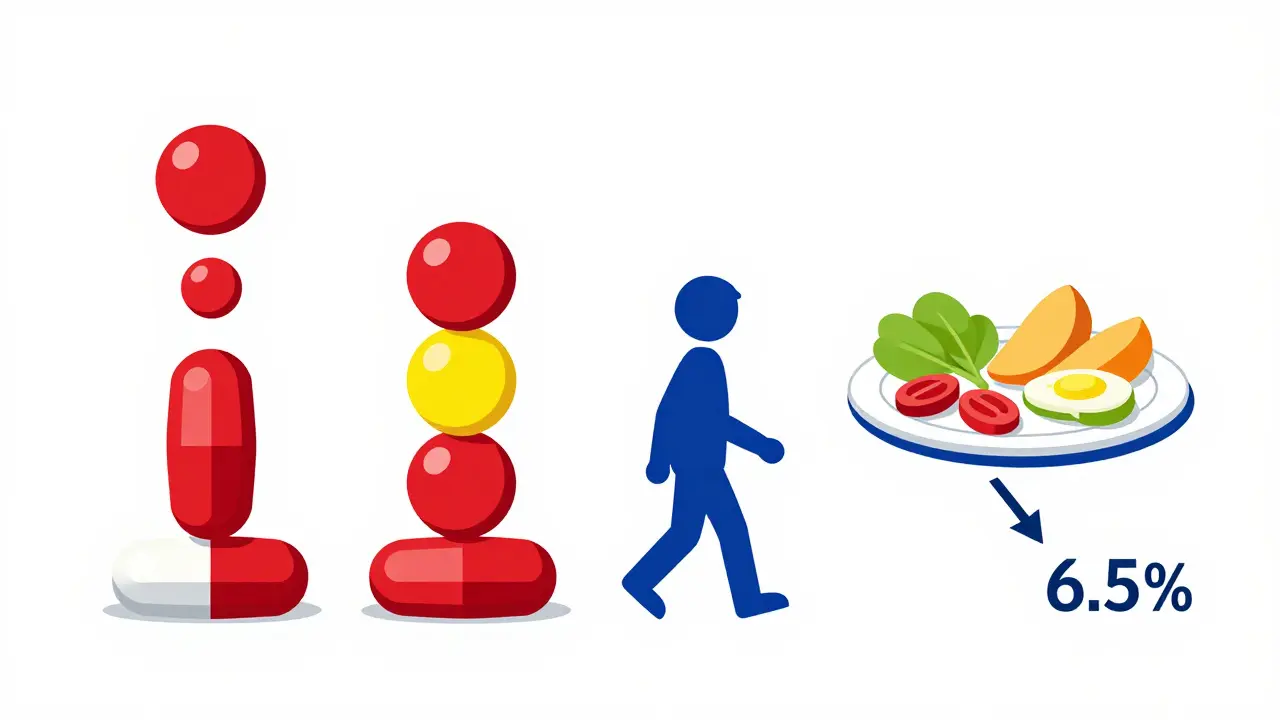
Can You Get There Without Surgery?
Yes. The DiRECT trial used a total diet replacement program-liquid meals for 8-12 weeks, followed by gradual food reintroduction and long-term support. No surgery. No drugs. Just structured weight loss.Other programs, like those from the American College of Lifestyle Medicine and NHS Scotland, use similar approaches: calorie control, protein-rich meals, regular physical activity, and behavioral coaching. You don’t need a gastric sleeve to get there. You need consistency.
That said, metabolic surgery (like gastric bypass) works even better. The ARMMS-T2D trial showed 37.5% remission after surgery at three years. But surgery isn’t for everyone. It’s expensive, carries risks, and requires lifelong vitamin monitoring. For most people, intensive lifestyle change is the first and best step.
Why This Matters Beyond Blood Sugar
Remission isn’t just about avoiding pills. It’s about reducing your risk of heart disease, stroke, nerve damage, and kidney failure. Even if you’re not fully in remission, losing 5-10% of your body weight cuts your risk of complications by up to 40%.People in remission report better energy, fewer cravings, improved sleep, and less joint pain. Their blood pressure drops. Their triglycerides fall. Their mood lifts. It’s not just diabetes management-it’s life improvement.
And here’s something most people don’t realize: being in remission can change how you see yourself. No longer a "diabetic" who needs meds to survive. You’re someone who took control. That mindset shift is powerful. It sticks.
What About Medication De-escalation?
Medication de-escalation isn’t just stopping drugs. It’s a planned, step-by-step process. You don’t just quit metformin cold turkey. You work with your doctor to lower doses slowly while monitoring your blood sugar daily.Some people start by dropping one drug. Then another. Some go from insulin to oral meds, then to no meds. Others keep one low-dose pill-like metformin-because it still helps with weight and insulin sensitivity, even if they’re in remission.
Dr. Michael Nauck, a leading expert, suggests we might need a second category: "remission with ongoing medication." That’s because some people stay in near-normal blood sugar ranges only because they’re still on a low dose of metformin or GLP-1 agonists. They’re not "cured," but they’re doing better than ever.
That’s okay. The goal isn’t to be medication-free at all costs. The goal is to be healthy. If a low-dose pill helps you keep the weight off and your blood sugar stable, then it’s working.
The Hard Truth: Remission Isn’t Permanent for Everyone
Let’s be honest. Not everyone will stay in remission. The science is clear: relapse is common. That doesn’t mean you failed. It means diabetes is a chronic condition with a strong genetic and environmental component.But here’s the flip side: even if you relapse, the time you spent in remission mattered. Studies suggest that time spent with normal blood sugar reduces long-term damage to your blood vessels, kidneys, and nerves. You bought yourself years. Maybe even a decade.
And if you relapse? You can try again. Weight loss works every time. The body doesn’t forget how to respond to it. You just need to restart the process.
How to Start
If you’re thinking about remission, here’s how to begin:- Get your HbA1c tested. Know your starting point.
- Set a realistic weight loss goal. Aim for 10% of your body weight.
- Work with a dietitian or lifestyle coach. Don’t guess. Get a plan.
- Track your food. Use an app or journal. Awareness changes behavior.
- Move daily. Walk 10,000 steps. Strength train twice a week.
- Talk to your doctor about de-escalating meds. Don’t stop on your own.
- Check your HbA1c every 3 months during the process.
- Once you’re in remission, keep your appointments. Stay vigilant.
You don’t need to go on a 1,200-calorie diet overnight. You don’t need to run marathons. You just need to lose weight, keep it off, and stay consistent.
What’s Next?
Science is still catching up. We don’t yet know exactly why some people stay in remission for 10 years and others relapse in 6 months. We don’t know the best long-term diet-low-carb, Mediterranean, plant-based? All work if they lead to weight loss.What we do know is this: type 2 diabetes remission is real. It’s not theoretical. It’s happening in clinics in Scotland, Australia, and the U.S. every day. And it’s not reserved for the young or the thin. It’s for anyone willing to make a sustained change.
So if you’re tired of counting pills, checking your blood sugar, and feeling like your body is working against you-there’s another path. It’s hard. It’s slow. But it’s possible. And it’s worth it.
Comments (15)
Juan Reibelo
January 24, 2026 AT 05:40
Okay, I need to say this: I lost 24 lbs in 5 months using the DiRECT plan, and my HbA1c dropped from 7.8% to 5.9%-no meds. I’m not cured. But I’m in remission. And yeah, I still check my sugar. Every. Single. Day.
Jamie Hooper
January 24, 2026 AT 17:19
so like… i got off metformin last year and now i eat pizza on sundays and feel like a boss?? 🤷♂️ diabetes? what’s that? 😎
Izzy Hadala
January 24, 2026 AT 17:56
While the DiRECT trial demonstrates statistically significant remission rates, one must consider the confounding variables of adherence, socioeconomic status, and baseline metabolic health. The generalizability of these findings to non-clinical populations remains empirically uncertain without longitudinal, randomized control data across diverse demographics.
Patrick Gornik
January 25, 2026 AT 01:52
Let’s be real-this isn’t about ‘remission.’ It’s about the pharmaceutical-industrial complex being terrified that people might realize they can outsmart their own biology without a prescription. The system doesn’t want you well-it wants you dependent. Metformin’s been around since the 1950s. Why? Because it’s cheap. And profitable. But your pancreas? It remembers how to work. It just needs you to stop feeding it poison. You’re not broken. You’re just overfed. And the real cure? It’s not in a pill. It’s in your hands. And your fork. And your will. And your refusal to let Big Pharma define your worth.
Luke Davidson
January 25, 2026 AT 07:44
Bro this hit different. I was on insulin for 3 years. Lost 30 lbs. Stopped everything. Now I walk 10k steps daily and eat like a normal human. My kids think I’m a superhero. I just think I’m finally listening to my body. You guys? You can do this. It’s not magic. It’s just consistency. And yeah, I still get cravings. But now I know: the sugar isn’t the enemy. The habit is.
Karen Conlin
January 26, 2026 AT 21:19
Let me tell you what no one says: remission isn’t about weight. It’s about worth. I used to feel like a failure every time I checked my glucose. Now? I’m proud. I’m not perfect. I slip. But I get back up. And if you’re reading this and thinking ‘I can’t’-you can. Start with one meal. One walk. One day. You don’t have to be a saint. Just show up. I’ve seen people in their 70s do this. And they’re happier than people half their age. You got this. I believe in you.
asa MNG
January 27, 2026 AT 16:35
ok but like i lost 15 lbs and my sugar went down but then i ate a whole cake and now im back to 8.4% and i cried in the grocery store and bought a tub of ice cream and my doctor said i need to try again but i just wanna nap forever 😭🍦 #diabetesstruggles #notsorry
Heather McCubbin
January 29, 2026 AT 09:24
So let me get this straight-you’re telling me people who can’t control their eating habits just need to ‘lose weight’? Like, that’s the solution? No one talks about the trauma, the depression, the emotional eating, the food deserts, the generational poverty. This isn’t a willpower issue. It’s a systemic failure. And now you’re blaming the victim? Classic.
Tiffany Wagner
January 29, 2026 AT 12:51
I’ve been in remission for 18 months. Still take metformin 500mg. Still walk. Still track. I don’t feel like I ‘failed’ because I’m not fully off meds. My doctor says it’s fine. I just feel… better. That’s enough.
Viola Li
January 30, 2026 AT 01:52
Remission? Please. This is just a marketing ploy by diet companies and wellness influencers. You think losing weight fixes insulin resistance? Try genetics. Try epigenetics. Try the fact that your body was designed to store fat in times of scarcity. You’re fighting evolution with a kale smoothie. This isn’t empowerment-it’s delusion.
venkatesh karumanchi
January 30, 2026 AT 15:55
I am from India. Many here think diabetes is from eating too much sugar. But it’s not. It’s from stress. From sleep. From walking 10 km to work. From eating rice every day. But when I lost 12 kg-slowly, with my family’s help-I stopped my medicine. Now I eat roti, but less. Walk more. Sleep better. It is not easy. But it is possible.
Jenna Allison
January 31, 2026 AT 11:53
For anyone thinking about this: talk to a registered dietitian. Not a TikTok guru. Not a YouTube ‘expert.’ A real RD. They’ll help you create a plan that fits your life-not some rigid 1200-calorie hell. And don’t skip the mental health support. This isn’t just physical. It’s emotional. You’re not alone.
Kevin Waters
January 31, 2026 AT 22:22
I’ve been in remission for 2 years. My HbA1c is 5.6%. I still have the same body. I still crave carbs. But now I know how to handle it. I don’t beat myself up. I just reset. And I tell everyone: you don’t have to be perfect. You just have to be persistent. One day at a time. That’s how you win.
Kat Peterson
February 1, 2026 AT 11:17
Ugh. Another ‘weight loss is the answer’ lecture. I’m so tired of this. I’m a size 14. I’m healthy. I run marathons. My HbA1c is 5.8%. But I’m not ‘in remission’ because I didn’t lose 20 lbs? What a joke. This is fatphobia dressed up as science. 🤦♀️ #HealthAtEverySize
Husain Atther
February 1, 2026 AT 20:38
Thank you for this balanced, evidence-based perspective. In my community, many believe diabetes is a life sentence. This article gives hope without false promises. I will share it with my patients. Consistency, not perfection. That is the message.