When you take a proton pump inhibitor (PPI) like omeprazole for heartburn and an antifungal like itraconazole for a stubborn fungal infection, you might think you’re just managing two separate problems. But in your body, these drugs are having a silent, potentially dangerous conversation - one that can leave you with dangerously low levels of the antifungal you need to survive.
Why Your Antifungal Isn’t Working
Proton pump inhibitors don’t just reduce stomach acid - they turn your stomach into a near-neutral environment. Normally, your stomach pH hovers around 1 to 2, which is strong enough to break down most pills and dissolve drugs that need acid to be absorbed. But when you take a PPI, that pH climbs to 4 or even 6. That’s not just a small change. It’s enough to stop certain antifungals from dissolving at all. The most affected drug? Itraconazole capsules. Studies show that when taken with a PPI, the amount of itraconazole that gets into your bloodstream drops by 50% to 60%. That’s not a minor dip. That’s the difference between a drug that works and one that doesn’t. For someone with invasive aspergillosis or coccidioidomycosis, this isn’t just inconvenient - it’s life-threatening. One study tracked a patient whose itraconazole blood levels jumped from 0.3 mcg/mL to 1.7 mcg/mL just by switching from omeprazole to famotidine. That’s more than a five-fold increase.Not All Antifungals Are Created Equal
This isn’t a universal problem. Fluconazole? It doesn’t care about stomach pH. It dissolves easily in water, so even if your stomach is neutral, it still gets absorbed. Voriconazole? It’s affected, but only about 22% to 35% - still significant, but not as bad as itraconazole. Posaconazole is tricky: the delayed-release tablet loses 40% of its absorption with PPIs, but the older oral suspension doesn’t drop nearly as much. The key difference? How the drug is formulated. Itraconazole capsules rely on acid to dissolve the solid particles inside. The liquid solution, on the other hand, already has the drug dissolved - so it doesn’t need stomach acid to work. That’s why the solution form only drops 10-15% in absorption with PPIs, not 60%. If you’re on itraconazole and you’re also on a PPI, the solution version is the safer choice.What About Other Acid Reducers?
Not all acid-reducing drugs are the same. H2 blockers like famotidine or ranitidine only raise stomach pH for 4 to 10 hours. PPIs? They shut down acid production for 12 to 24 hours. That’s why PPIs cause much bigger drops in antifungal absorption. One study showed omeprazole cut itraconazole levels by 57%, while famotidine cut it by 41%. That’s a big gap. Antacids like Tums or Maalox? They work fast and fade fast. If you take them at least two hours before or after your antifungal, they won’t interfere much. But if you’re popping antacids all day, you’re still creating a problem. The longer your stomach stays above pH 3, the worse it gets for drugs like itraconazole and posaconazole.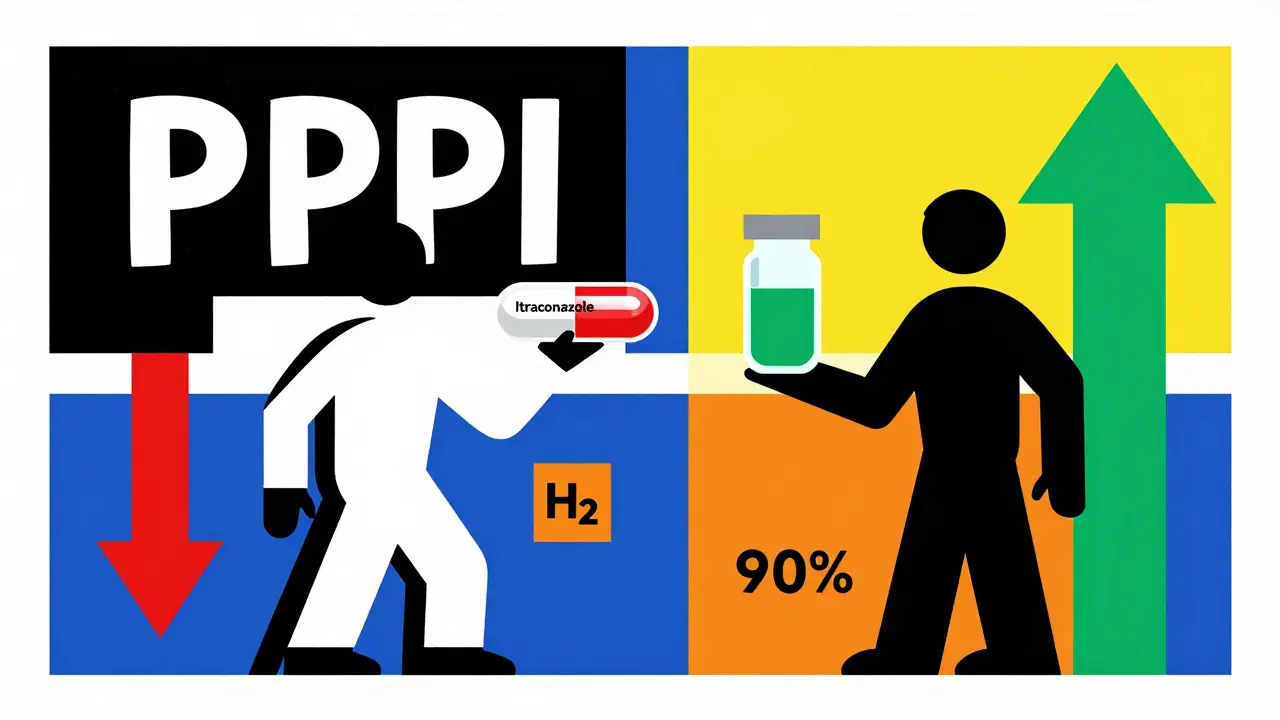
The Hidden Risk: Treatment Failure and Resistance
When antifungal levels drop too low, the fungus doesn’t die - it adapts. The European Committee on Antimicrobial Susceptibility Testing (EUCAST) warns that subtherapeutic antifungal levels can turn a susceptible infection into a resistant one. That means the drug that should’ve cured you might not work at all next time - even if you take the full dose later. Hospital pharmacists report seeing this firsthand. A 2022 survey found 68% of them encountered at least one itraconazole-PPI interaction every month. And 23% of those cases led to confirmed treatment failures. That’s not a rare mistake. It’s a pattern. One patient in Massachusetts General Hospital had chronic pulmonary aspergillosis. His itraconazole levels were so low, his doctor thought the infection was getting worse. It turned out he was on omeprazole. Once they switched him to famotidine and gave him the itraconazole solution, his levels climbed into the therapeutic range. He didn’t need a new drug. He just needed the right combination.What Should You Do?
If you’re prescribed itraconazole capsules and you’re on a PPI, here’s what you need to do:- Ask your doctor if you can switch to itraconazole solution instead. It’s less affected by PPIs.
- If you must use capsules, stop the PPI if possible. If you can’t stop it - say, because you have a history of bleeding ulcers - switch to an H2 blocker like famotidine.
- Take itraconazole at least two hours before your PPI. Timing matters.
- For posaconazole delayed-release tablets, take them with a glass of cola. The acidity helps absorption.
- Ask for therapeutic drug monitoring. For itraconazole, the target level is 0.5-1.0 mcg/mL. If you’re below that, your treatment isn’t working.
New Hope: Better Formulations and Unexpected Synergies
There’s good news on the horizon. In 2023, the FDA approved a new version of itraconazole called Tolsura. It’s designed to absorb regardless of stomach pH. In trials, it only dropped 8% in absorption with PPIs - compared to 50% for the old capsules. That’s a game-changer. Even more surprising? Research from 2025 found that when you combine low-dose omeprazole with itraconazole in a lab, they actually work better together against resistant strains of Aspergillus fumigatus. In 77.6% of tested fungal strains, the combo killed more fungus than either drug alone. This isn’t a mistake - it’s a discovery. The National Institutes of Health is now running clinical trials to see if this synergy can be used intentionally to treat drug-resistant fungal infections.The Bigger Picture
About 15% of U.S. adults take PPIs long-term. Around 5-7% of hospitalized patients get systemic antifungals. That means thousands of people are getting these drugs together - often without anyone checking if it’s safe. The cost? Around $287 million a year in wasted drugs and failed treatments. The solution isn’t just about switching pills. It’s about communication. Pharmacists need to flag these interactions. Doctors need to ask: “Are you on a PPI?” before prescribing itraconazole. Patients need to speak up: “I take omeprazole every morning.” This isn’t a niche problem. It’s a common, preventable mistake that’s costing lives. But with better awareness, better formulations, and better timing - it doesn’t have to be.Can I take fluconazole with a proton pump inhibitor?
Yes. Fluconazole is not affected by stomach pH changes, so it absorbs normally whether you’re on a PPI, H2 blocker, or nothing at all. It’s one of the few antifungals that works reliably with acid-suppressing drugs.
Why does itraconazole need stomach acid to work?
Itraconazole capsules contain the drug in solid form. It needs a low pH (below 3) to dissolve properly in the stomach. Without enough acid, the capsules don’t break down, so the drug can’t be absorbed into your bloodstream. The solution form already has the drug dissolved, so it doesn’t need acid.
Is it safe to take PPIs and antifungals if I space them out?
For itraconazole solution, spacing by two hours can help reduce the interaction, but it’s not foolproof. For capsules, spacing doesn’t fix the problem - the PPI is still suppressing acid for 24 hours. The best option is to avoid PPIs entirely or switch to the solution form.
What should I do if I can’t stop my PPI?
Talk to your doctor about switching to an H2 blocker like famotidine, which has a shorter effect on stomach pH. Also, ask if you can switch from itraconazole capsules to the solution or to Tolsura, the newer pH-independent formulation. If you’re on posaconazole tablets, take them with an acidic drink like cola.
Can PPIs make fungal infections worse?
Not directly. But by lowering antifungal levels, PPIs can cause treatment failure, which lets the infection grow. This can lead to drug resistance, meaning the fungus becomes harder to treat in the future. In some cases, it can turn a manageable infection into a life-threatening one.
Comments (10)
Sarah Mailloux
January 14, 2026 AT 19:18
Wow, I had no idea PPIs could wreck antifungal absorption like this. My grandma’s on omeprazole and got prescribed itraconazole last year-thank god her pharmacist caught it. This needs to be shouted from the rooftops.
Mike Berrange
January 16, 2026 AT 02:21
You people are missing the real issue. The FDA approved Tolsura in 2023 but didn’t mandate pharmacies to switch patients automatically. That’s corporate greed. They’d rather keep selling $200/month omeprazole than push a $500 pH-independent version. Pharma’s got us all on the hook.
Dan Mack
January 17, 2026 AT 07:25
They’re hiding this on purpose. PPIs and antifungals together? It’s not an accident. Big Pharma wants you sick longer. Fluconazole is cheaper and works fine. Why do you think they push the expensive ones? Wake up.
Nishant Garg
January 18, 2026 AT 03:55
In India, we’ve seen this for years-doctors prescribe omeprazole for ‘digestion’ and then antifungals for athlete’s foot that won’t clear. No one connects the dots. I once had a cousin whose fungal nail infection turned into systemic candidiasis because the doctor didn’t ask about acid meds. We’re lucky if our local pharmacist speaks English, let alone knows drug interactions. This isn’t just American-it’s global.
ellen adamina
January 19, 2026 AT 15:03
I’ve been on famotidine for years after a bad ulcer. My doctor switched me from itraconazole capsules to the solution when I got aspergillosis. It made all the difference. I’m just glad someone finally wrote this down clearly. Thank you.
Jami Reynolds
January 20, 2026 AT 09:47
Let me be clear: if you’re taking a PPI and an antifungal simultaneously without therapeutic drug monitoring, you’re not being treated-you’re being experimented on. The FDA’s own data shows 68% of pharmacists see this monthly. That’s malpractice waiting to happen. And no, ‘spacing them out’ isn’t a fix. It’s a myth peddled by lazy clinicians.
Niki Van den Bossche
January 20, 2026 AT 16:30
There’s a metaphysical layer here, isn’t there? The stomach as the altar of digestion, the acid as the sacred flame-when we suppress it with chemical tyranny, we don’t just break drug absorption, we break the body’s natural rhythm. We’ve forgotten that medicine isn’t about domination, but harmony. The synergy between low-dose omeprazole and itraconazole? That’s not a fluke. It’s the universe whispering that balance, not eradication, is the true cure.
Tom Doan
January 21, 2026 AT 18:03
So let me get this straight: a 2025 NIH study found that combining omeprazole with itraconazole *kills more fungus* in lab settings… but we’re still telling people to avoid the combo? The irony is almost poetic. Are we afraid of unintended consequences, or just too afraid to think outside the pill bottle?
Gloria Montero Puertas
January 23, 2026 AT 05:47
And yet, people still take Tums with their antifungals like it’s candy. I’ve seen it. In the ER. Last week. A 58-year-old man with candidemia, on pantoprazole, popping antacids every hour because ‘his stomach felt funny.’ He didn’t even know what an antifungal was. This isn’t science-it’s a public health circus.
Nicholas Urmaza
January 23, 2026 AT 19:40
STOP. Just stop. If you’re on a PPI and need an antifungal, your doctor needs to know. No excuses. No ‘I thought it was fine.’ This isn’t optional. This is life or death. Get tested. Get switched. Get informed. Or get ready to pay the price.