Medical Term Translator
When you read your medical record, you may encounter clinical terms like "poorly controlled DM" or "E11.9." This tool helps translate those terms into language you can understand.
Enter a medical term or code to see its plain language explanation
Common Examples
E11.9
Type 2 Diabetes without complications
Common Examples
poorly controlled DM
Blood sugar levels have been consistently high
Common Examples
non-adherence to metformin
Skipping your diabetes medication
When you read your medical record and see "poorly controlled DM", do you think it means you’re failing as a patient? Or do you think it’s just a way to say your blood sugar’s been high? You’re not alone. Many patients feel confused, even blamed, by the words doctors write down. Meanwhile, your doctor sees "E11.9" - a code for Type 2 Diabetes without complications - and thinks they’ve been clear. This gap isn’t a mistake. It’s a systemic problem built into how healthcare records are written.
Why Your Doctor’s Notes Don’t Sound Like You
Healthcare providers use standardized medical language because it’s precise, universal, and required for billing and insurance. The ICD-10 system alone has over 70,000 diagnosis codes. CPT codes track procedures - more than 10,000 of them. These aren’t meant for you. They’re meant for computers, insurers, and other clinicians who need to quickly understand what happened during your visit. But patients don’t think in codes. You think in symptoms: "I’m always tired," "My feet feel numb," "I keep drinking water and still feel thirsty." You don’t say "hypertension." You say "my blood pressure is through the roof." When your doctor writes "Stage 2 Hypertension (I10)" in the chart, you see jargon. And research shows 68% of patients misunderstand common medical terms like "colitis" or "hyperlipidemia." This isn’t about intelligence. It’s about language. Doctors are trained to use clinical labels. Patients live with the experience. And when those two worlds collide in a medical record, confusion follows.What Gets Lost in Translation
The difference isn’t just words - it’s meaning. A provider sees "non-adherence to metformin" and thinks you’re skipping pills. You might be skipping them because the pill makes you nauseous, you can’t afford refills, or you thought it was just for "sugar" and not for "heart protection." The label doesn’t capture your story. A 2023 Medscape survey found that 64% of physicians spend 15 to 30 minutes per visit just explaining terms patients don’t understand. That’s half a consultation gone - time that could’ve been spent adjusting treatment, answering real concerns, or listening. And it’s not just about confusion. It’s about trust. On patient forums like PatientsLikeMe, someone wrote: "My doctor wrote 'poorly controlled DM' - I thought it meant I was a bad person." That’s not what the code means. But that’s what it felt like. When patients feel judged by their records, they stop asking questions. They avoid follow-ups. And worse - they stop taking meds. The American Medical Association found that 57% of patients feel confused by medical terms in their records. Of those, 32% skipped care because of it. That’s not a small number. That’s millions of people avoiding doctors because they don’t understand what’s written about them.How the System Is Trying to Fix This
The problem isn’t new. But the push to fix it is stronger than ever. The 21st Century Cures Act of 2016 forced providers to give patients direct access to their clinical notes - no filters, no redactions. By April 2021, every U.S. hospital had to comply. Suddenly, millions of patients could read what their doctors wrote. And many were shocked. So healthcare systems started changing. Kaiser Permanente launched "Open Notes" in 2010. By 2021, they saw a 27% drop in patient confusion and a 19% increase in medication adherence. Why? Because patients could read their notes, ask questions, and feel included. Now, hospitals are rewriting notes for patients. Mayo Clinic created "plain language" templates in their EHR. Instead of "myocardial infarction," the patient-facing version says "heart attack." Instead of "polyneuropathy," it says "nerve damage in feet and hands." In their pilot, patient confusion dropped by 38%. The Office of the National Coordinator for Health IT found that 41% of healthcare organizations now adjust clinical notes for patient readability. That’s up from just 8% in 2017. It’s not perfect - but it’s moving.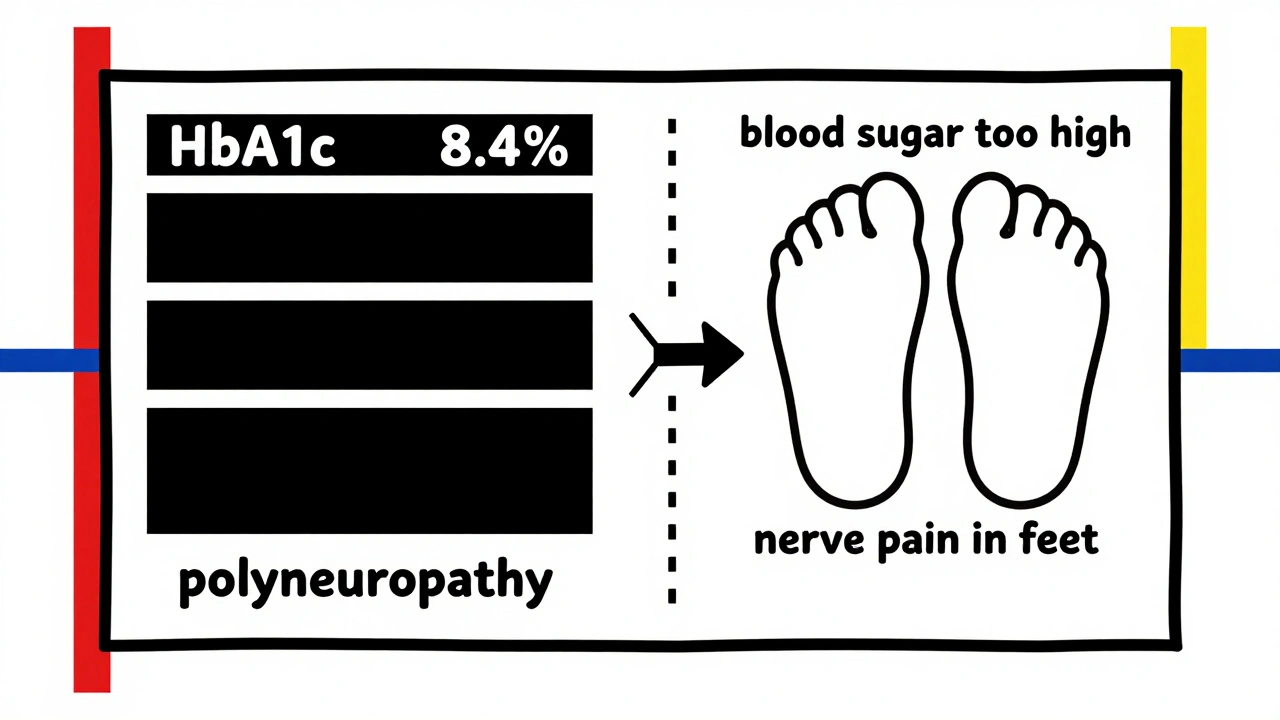
What’s Changing Behind the Scenes
The real shift is happening in the tech that runs hospitals. The new ICD-11, rolled out globally in 2022, includes patient-friendly descriptions alongside clinical codes for the first time. That means when a provider picks "E11.9," the system can also show: "Type 2 diabetes with no complications - you may feel tired, thirsty, or need to pee often." And then there’s FHIR - the modern data standard adopted by 78% of major U.S. health systems. FHIR lets systems show two versions of the same note: one for providers, one for patients. The provider sees "HbA1c 8.4%"; the patient sees "Your average blood sugar over the last 3 months was high." Even AI is stepping in. Google’s Med-PaLM 2, released in 2023, can convert clinical notes into plain language with 72.3% accuracy. It’s not perfect yet - clinical work needs 95% accuracy - but it’s proof that machines can help bridge this gap.What You Can Do Right Now
You don’t have to wait for your doctor’s office to change. Here’s what you can do today:- Ask for plain language. After your visit, say: "Can you explain that term in simpler words?" Or: "What does this code mean for me?"
- Read your notes. Most providers now offer patient portals like MyChart. Log in. Read your visit summary. Don’t assume you know what it says.
- Use the teach-back method. After your doctor explains something, say: "So if I understand right, you’re saying I need to take this pill twice a day because it helps lower my blood sugar. Is that correct?" This cuts miscommunication by 45%, according to JAMA Internal Medicine.
- Write down your own version. Before your next visit, jot down how you feel: "I’ve been dizzy after lunch," "My knee hurts when I climb stairs," "I skipped my pill because I forgot." Bring that list. It helps your provider see you, not just your code.
What Providers Are Learning Too
It’s not just patients who are learning. Doctors are realizing that the old way - writing dense, coded notes and assuming patients "get it" - doesn’t work. A 2021 study by UCSF’s Dr. Thomas Bodenheimer found that 30-40% of medication errors happen because patients misunderstood what they were told. Now, training programs for doctors include communication modules. Health Information Management (HIM) professionals - the people who code and clean up medical records - are trained in both ICD-10 and patient communication. They spend over 1,200 hours learning how to translate clinical data into something that doesn’t scare patients. And reimbursement is changing too. Medicare now ties 2% of hospital payments to how well patients rate their communication with providers. If you say your doctor didn’t explain things clearly, it costs the hospital money. That’s a powerful incentive.The Future: Two Versions of the Same Truth
The goal isn’t to eliminate medical language. It’s to make sure both versions exist. The provider needs "E11.9" for billing and research. You need to know your blood sugar is high and what to do about it. By 2027, experts predict 60% of EHR systems will automatically translate clinical terms into plain language - right inside the patient portal. That means when your doctor types "hyperlipidemia," you’ll see "high cholesterol." When they write "depression screening positive," you’ll see "you’re showing signs of low mood that we can help with." This isn’t about dumbing down medicine. It’s about making sure medicine works for everyone - not just those who speak the code.When your health record speaks your language, you’re more likely to understand your condition, take your meds, and show up for your next appointment. That’s not just better communication. It’s better care.
Why do doctors use medical jargon in patient records?
Doctors use medical jargon because it’s standardized, precise, and required for billing, insurance claims, and communication between providers. Systems like ICD-10 and CPT codes ensure everyone - from hospitals to insurers - understands exactly what diagnosis or procedure was performed. But these codes aren’t meant for patients. They’re designed for efficiency in clinical and administrative workflows, not for patient understanding.
Can I ask my doctor to rewrite my medical notes in plain language?
Yes, you can and should. You have the right to understand your health information. Ask your doctor during your visit: "Can you explain this in simpler terms?" or "Could you write this in a way I’ll understand?" Many providers now use plain-language templates, especially if you’re using a patient portal like MyChart. If they don’t, ask if they can add a plain-language summary to your record.
What’s the difference between ICD-10 and patient-friendly labels?
ICD-10 uses standardized codes like E11.9 for "Type 2 Diabetes Mellitus without complications." Patient-friendly labels say things like: "You have type 2 diabetes - your body doesn’t use insulin well, which can make you tired, thirsty, and need to urinate often." The code is for billing and data tracking. The plain-language version helps you understand your condition and take action.
How does reading my medical record help me?
Reading your record helps you catch errors, understand your diagnosis, and remember what was discussed. A 2021 Kaiser Permanente study found that patients who read their notes had 27% less confusion about their condition and were 19% more likely to take their medications correctly. When you know what’s written, you can ask better questions and partner with your provider instead of feeling left out.
Are there laws that require doctors to share notes with patients?
Yes. The 21st Century Cures Act, which took full effect in April 2021, requires all U.S. healthcare providers to give patients immediate access to their clinical notes without charge or delay. This includes doctor’s notes, lab results, and discharge summaries. You can access them through your provider’s patient portal or request them in writing. This law was created to improve transparency and patient engagement.

Comments (8)
shalini vaishnav
December 3, 2025 AT 22:29
Let’s be real-this whole ‘plain language’ movement is just another Western liberal fantasy. In India, we’ve been managing diabetes for generations without someone translating ‘E11.9’ into ‘you feel thirsty.’ If you can’t read a medical chart, that’s your problem, not the system’s. Medical terminology exists for a reason: precision. Diluting it for emotional comfort doesn’t improve outcomes-it just breeds ignorance.
Joykrishna Banerjee
December 4, 2025 AT 03:39
Actually, the real issue is that patients lack the intellectual rigor to engage with clinical nomenclature. ICD-10 isn’t designed for laypeople-it’s a taxonomic framework honed over decades by epidemiologists and coders. If you can’t parse ‘polyneuropathy’ without a glossary, perhaps you shouldn’t be self-diagnosing on WebMD. This isn’t elitism-it’s epistemic responsibility.
Albert Essel
December 5, 2025 AT 07:59
There’s merit to both sides. Medical jargon serves a functional purpose in clinical workflows, but ignoring patient comprehension is a failure of care design. The fact that 32% of patients skip care due to confusion isn’t just a statistic-it’s a moral indictment. Systems that offer dual-view notes (provider + patient) aren’t ‘dumbing down’ medicine-they’re democratizing it. Precision doesn’t require obscurity.
Gavin Boyne
December 5, 2025 AT 18:39
Oh wow, so now we’re treating patients like toddlers who need a cartoon version of their own diagnosis? Next they’ll replace ‘myocardial infarction’ with ‘heart got mad and stopped working.’ Meanwhile, in the real world, a patient who can’t understand ‘HbA1c’ probably can’t understand ‘take your pill twice a day’ either. Maybe the real fix isn’t rewriting notes-it’s teaching people how to read.
Rashi Taliyan
December 6, 2025 AT 14:45
I cried reading this. My doctor wrote ‘non-adherence’ next to my name and I thought I was a monster. I was skipping pills because I couldn’t afford them, not because I didn’t care. No one ever asked. No one ever explained. When I finally read my own note and saw ‘poorly controlled DM’-I thought I’d failed God, my family, myself. This isn’t about jargon. It’s about shame. And someone needs to stop making patients feel like criminals for being sick.
Kara Bysterbusch
December 7, 2025 AT 03:43
It is profoundly disconcerting to observe that, in an era where data interoperability and patient autonomy are heralded as cornerstones of modern healthcare, we persist in maintaining a linguistic chasm between the clinician and the layperson. The adoption of FHIR and ICD-11’s dual-labeling architecture represents not merely a technical advancement, but a philosophical recalibration: medicine must serve the human being, not the algorithm. To withhold intelligible information is not to preserve professionalism-it is to perpetuate inequity.
Rashmin Patel
December 9, 2025 AT 02:57
Look, I get it-doctors use codes because they’re efficient. But here’s the thing: if your patient doesn’t understand what’s written about them, efficiency doesn’t matter. I’ve seen people stop insulin because they thought ‘DM’ meant ‘diabetic monster’ and felt guilty. I’ve seen elderly folks skip appointments because they thought ‘Stage 2 Hypertension’ meant they were dying tomorrow. This isn’t just about translation-it’s about dignity. And honestly? If your EHR can’t spit out a plain-language version alongside the code, it’s broken. I’ve been using MyChart for years and when they added the ‘what this means for you’ pop-ups? My dad finally started taking his meds. That’s not magic. That’s basic human respect.
sagar bhute
December 10, 2025 AT 03:13
This whole article is a joke. You think patients want to be coddled? They want results. I’ve been in ERs across three countries. The ones who survive are the ones who learn the language, not the ones who whine because ‘colitis’ sounds scary. Stop infantilizing people. If you can’t handle medical terms, don’t go to the doctor. Or better yet-don’t get sick.