When cancer turns everyday life into pain, palliative care isn’t giving up - it’s fighting for comfort
Imagine waking up every morning not to the sound of your alarm, but to a dull ache in your bones, a sharp sting in your side, or a burning sensation that won’t fade no matter how you move. For 70 to 90% of people with advanced cancer, this isn’t imagination - it’s reality. And yet, most of that pain can be controlled. Not just eased. Controlled. The truth is, we have the tools. We just don’t always use them.
Palliative care in cancer isn’t about end-of-life decisions. It’s not something you wait for until there’s nothing left to cure. It’s about living as fully as possible while you’re fighting. It’s about making sure your pain doesn’t steal your sleep, your appetite, your time with family, or your will to keep going. And the best part? It works - when it’s done right.
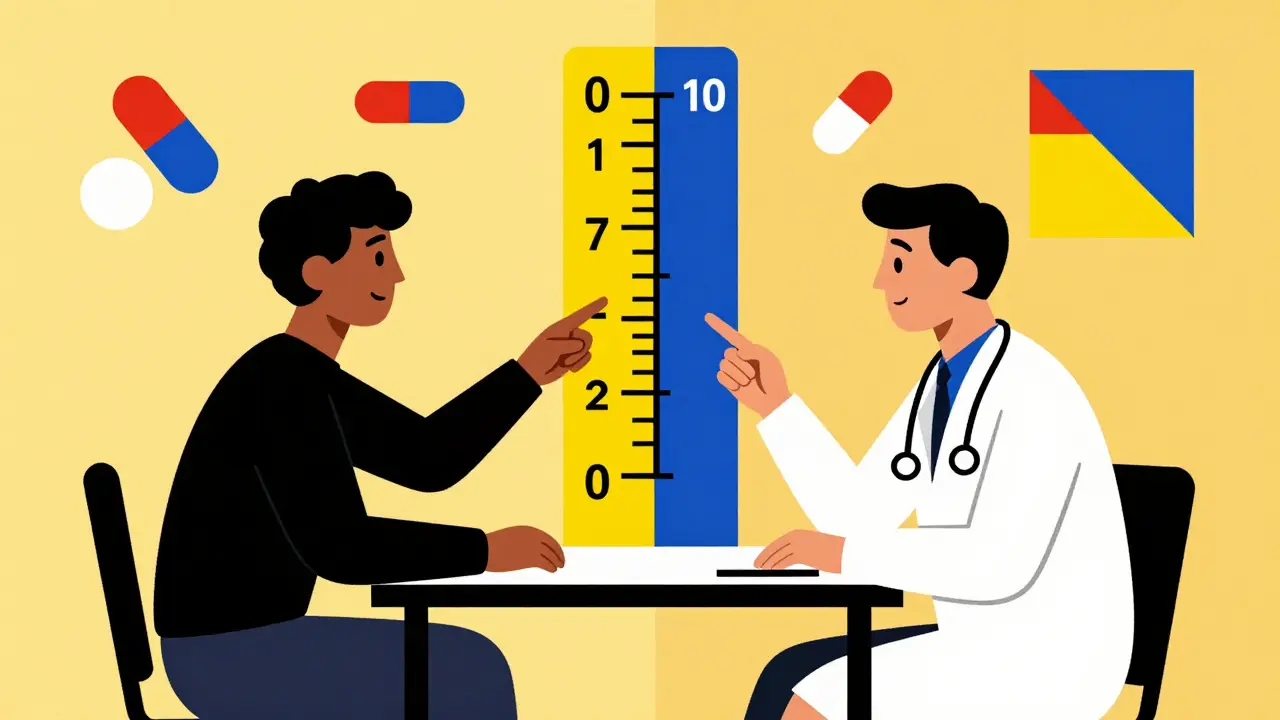
How cancer pain is measured - and why it matters
Doctors don’t guess how much pain you’re in. They ask. Every time. And they use a simple scale: 0 to 10. Zero means no pain. Ten means the worst pain you can imagine. That’s it. No fancy machines. No blood tests. Just you telling the truth.
This number isn’t just for paperwork. It’s the key to getting you the right dose of medicine. If your pain is a 3, you might get acetaminophen or ibuprofen. If it’s a 7 or higher, you’ll likely need an opioid like morphine. But here’s what many don’t realize: if you don’t report your pain, they can’t treat it. And too many people stay quiet - afraid of being seen as weak, or worse, addicted.
Studies show 65% of cancer patients worry about addiction. But in cancer, addiction is rare when opioids are used properly. What’s dangerous isn’t taking the medicine - it’s not taking enough. Pain that’s ignored becomes harder to control. And it doesn’t just hurt your body. It drains your spirit.
The three-step ladder to pain control - and what each step really means
The World Health Organization’s three-step analgesic ladder has guided cancer pain treatment since 1986. It’s simple, proven, and still the gold standard today.
- Step 1 (Mild pain): Acetaminophen (up to 4,000 mg a day) or NSAIDs like ibuprofen (400-800 mg every 8 hours). These work for aching joints or headaches from treatment.
- Step 2 (Moderate pain): Add a weak opioid like codeine (30-60 mg every 4 hours). This isn’t just extra strength Tylenol - it’s a step up when the first drugs aren’t enough.
- Step 3 (Severe pain): Strong opioids like morphine. Starting dose? 5-15 mg every 4 hours. But here’s the catch: it’s not about hitting a number. It’s about finding the dose that lets you sleep, eat, and talk with your kids without wincing.
And you don’t just take these pills once. They’re scheduled - every 4 to 6 hours, like clockwork - to keep pain from coming back. Plus, you get extra doses for breakthrough pain: sudden spikes that sneak in between scheduled pills. That’s usually 10-15% of your total daily dose.
Doctors adjust doses every 24 to 48 hours until you’re comfortable. No waiting. No “let’s see how it goes.” If you’re still hurting after two days, the dose goes up. That’s the rule.
When opioids aren’t enough - and what else works
Opioids are powerful, but they’re not the whole story. Some pain isn’t from tumors pressing on nerves - it’s from nerves firing on their own. That’s neuropathic pain. It feels like electric shocks, burning, or tingling. For that, you need different tools.
- Gabapentin or pregabalin for nerve pain. Doses start low - 100 mg three times a day - and slowly increase. It takes weeks to work, but for some, it’s the difference between lying still and sitting up.
- Duloxetine, an antidepressant, helps with both nerve pain and the low mood that often comes with chronic illness.
- Dexamethasone, a steroid, reduces swelling around tumors - especially in bone metastases. A daily 4-16 mg dose can turn a 9/10 pain into a 3/10.
And for bone pain? Radiation works wonders. A single 8 Gy treatment - just one session - can cut pain in half for many. It’s quick. It’s safe. And it’s often overlooked.
For patients on high-dose opioids who develop side effects - nausea, confusion, or even more pain from opioid-induced hyperalgesia - switching opioids helps. You don’t just crank up the dose. You switch to fentanyl or methadone. That’s not failure. That’s smart medicine.
Quality of life isn’t just about pain - it’s about being able to live
Quality of life sounds vague. But in cancer, it’s concrete. Can you hug your grandchild? Eat your favorite meal? Walk to the mailbox? Talk without crying? Those are the real measures.
Research shows that when palliative care starts early - within 8 weeks of diagnosis - patients report 20 to 30% better quality of life. Not just less pain. Better sleep. Less anxiety. More time doing what matters.
And here’s something most people don’t know: early palliative care doesn’t shorten life. It extends it. One major study found metastatic cancer patients who got early palliative care lived 2.5 months longer than those who didn’t. Why? Because they weren’t exhausted by uncontrolled pain. They could tolerate treatment better. They had more energy to fight.
Palliative teams don’t just hand out pills. They check in on depression. They help families talk about hard things. They connect you with social workers, chaplains, or physical therapists. They make sure your care plan matches your values - not just the protocol.
Why pain control still fails - and how to fix it
Even with all the guidelines, pain is still undertreated. Why?
- Doctors don’t ask enough. A 2017 study found 40% of oncology nurses weren’t certified in pain management. If your provider doesn’t know the ladder, they won’t use it.
- Patients don’t speak up. Cultural beliefs, fear of addiction, or not wanting to “be a burden” keep people silent. In some Asian and Hispanic communities, up to 28% underreport pain because stoicism is valued.
- Insurance won’t cover non-drug help. Physical therapy, acupuncture, counseling - these work. But many plans won’t pay for them unless they’re tied to a “curative” treatment.
What can you do? Ask for a palliative care consult. Right now. Don’t wait until you’re in crisis. Tell your oncologist: “I’m having pain. I want help managing it.” If they say no, ask for a second opinion. You have the right to comfort.
Use a pain diary. Write down when it hurts, where, how bad, and what helped. Bring it to every appointment. It’s your best tool.

What’s new in cancer pain care - and what’s coming
Technology is changing how we track pain. Apps now let patients log pain levels in real time. One 2021 study showed this improved documentation accuracy by 22%. That means doctors see patterns you might miss - like pain spikes after chemo or at night.
Genetic testing is starting to help too. Some people metabolize morphine too fast or too slow because of their CYP450 genes. Testing can tell your doctor: “This drug won’t work for you. Try this one.”
And new drugs are coming. Twelve are in late-stage trials targeting cancer-specific pain pathways - like nerve compression or bone destruction - without opioids. These could be game-changers.
But the biggest shift? The CDC now recognizes cancer pain is different. Their 2022 guidelines include a clear exception: for cancer, higher opioid doses are okay if they’re needed for comfort. That’s huge. It means doctors can treat pain without fear of punishment.
Final truth: You deserve to be comfortable
Palliative care isn’t surrender. It’s strength. It’s saying: “I’m still fighting - and I won’t let pain win.”
You don’t have to suffer. You don’t have to be brave by staying quiet. You don’t have to choose between pain relief and being “normal.”
The tools exist. The guidelines are clear. The evidence is overwhelming. If your pain is holding you back - from laughter, from touch, from life - speak up. Ask for help. Demand a plan. Because you’re not just a patient. You’re a person who deserves to feel human.
Is palliative care only for people who are dying?
No. Palliative care is for anyone with a serious illness - including cancer - at any stage. It’s not about giving up. It’s about adding support to your treatment. Many people start palliative care right after diagnosis to manage side effects, pain, and stress. Studies show early care improves quality of life and even extends survival.
Will opioids make me addicted if I use them for cancer pain?
Addiction is rare in cancer patients using opioids for pain under medical supervision. The goal isn’t to get high - it’s to be comfortable enough to sleep, eat, and be with loved ones. Physical dependence (needing the drug to avoid withdrawal) is normal with long-term use, but that’s not addiction. Addiction involves compulsive use despite harm - something very uncommon in this context.
What if my pain medicine stops working?
If your current pain control isn’t working, it’s not because you’ve built up a tolerance - it’s because your pain has changed. Your tumor may have grown, nerves may be involved, or your body’s responding differently. Talk to your doctor. You may need a higher dose, a different opioid, or an adjuvant like gabapentin or dexamethasone. Opioid rotation - switching from morphine to fentanyl or methadone - is a common and safe strategy when one drug stops working.
Can radiation really help with cancer pain?
Yes. For bone metastases - which cause severe, constant pain - radiation is often very effective. A single 8 Gy treatment can reduce pain by half in many patients, with relief lasting months. It’s quick, non-invasive, and doesn’t interfere with other treatments. If you have pain in your spine, hips, or ribs, ask if radiation could help.
How do I know if I need a palliative care team?
You don’t need to wait for a crisis. If your pain isn’t controlled with standard meds, if you’re feeling overwhelmed by symptoms, if you’re anxious or depressed, or if your family is struggling to help - that’s when you need palliative care. The NCCN recommends referral if pain is above 4/10 despite treatment, or if you have high distress on a simple screening tool. Ask your oncologist for a consultation. You don’t need permission - just a request.
What to do next
If you or someone you love has cancer and is in pain, don’t wait. Start with these steps:
- Rate your pain daily on a scale of 0-10. Keep a simple log.
- Ask your oncologist: “Can we refer me to a palliative care team?”
- Request a pain assessment - not just a quick check, but a full evaluation of location, type, and triggers.
- If opioids are prescribed, ask about breakthrough doses and side effect management.
- Ask if non-drug options like physical therapy, acupuncture, or radiation are appropriate.
Pain doesn’t have to be part of your cancer journey. It’s a symptom - and symptoms can be treated. You deserve to live well, even while fighting.

Comments (11)
Alec Stewart Stewart
February 3, 2026 AT 10:30
This hit me right in the chest. My dad went through this last year. They didn't bring up palliative care until he was barely able to stand. I wish we'd known sooner. You're right-it's not giving up. It's fighting smarter. 💙
Samuel Bradway
February 4, 2026 AT 11:22
I’ve seen too many people suffer in silence because they think opioids = addiction. It’s not true. My aunt was on morphine for 8 months and still danced at her granddaughter’s wedding. Pain control isn’t weakness-it’s dignity.
Caleb Sutton
February 5, 2026 AT 13:29
They’re hiding the truth. Big Pharma pushed opioids because they make billions. They don’t want you to know about the real cures-like cannabis oil or frequency therapy. The system is rigged to keep you dependent. 0/10 trust.
pradnya paramita
February 6, 2026 AT 20:42
The WHO analgesic ladder remains the most evidence-based framework, but adjuvant pharmacotherapy is often underutilized. For neuropathic pain, gabapentinoids require titration over 7–14 days to reach therapeutic plasma concentrations. Also, dexamethasone’s anti-edema effect in spinal metastases is dose-dependent-4 mg q24h is often subtherapeutic; 8–16 mg is more effective. Don’t forget to monitor for hyperglycemia and insomnia.
Jamillah Rodriguez
February 8, 2026 AT 04:53
Okay but like… why is this post 5000 words? I just wanted to know if my mom should ask for morphine. Can we get a TL;DR? 😩
Susheel Sharma
February 8, 2026 AT 23:06
The clinical elegance of opioid rotation is breathtaking-yet most oncologists are still operating on 1998 protocols. Meanwhile, the CDC’s 2022 exception for cancer pain is a quiet revolution. Still, insurance denials for acupuncture and PT? Pathetic. We treat cancer like a math problem, not a human experience.
Prajwal Manjunath Shanthappa
February 9, 2026 AT 17:51
I’m sorry-but this is exactly why Western medicine is failing… You reduce human suffering to a 0–10 scale? You quantify dignity? You commodify agony into dosing schedules? You’re not healing-you’re administrating. Where’s the soul in this? Where’s the silence? Where’s the grace?
Alex LaVey
February 10, 2026 AT 13:42
To anyone reading this who’s scared to speak up: you’re not a burden. Your comfort matters. Your joy matters. Your quiet nights, your favorite tea, your granddaughter’s laugh-all of it is worth fighting for. Ask for help. You’ve earned it.
Joy Johnston
February 12, 2026 AT 01:20
The integration of palliative care into oncology workflows remains suboptimal despite NCCN guidelines. A prospective cohort study from Memorial Sloan Kettering (2020) demonstrated that early referral (≤6 weeks post-diagnosis) correlated with a 31% reduction in emergency department visits. Systemic barriers include lack of provider training and reimbursement limitations. A multidisciplinary team approach is non-negotiable.
Shelby Price
February 12, 2026 AT 05:56
I didn’t know radiation could help with bone pain. That’s wild. I thought it was just for killing tumors. 🤯
Nathan King
February 13, 2026 AT 22:06
While the empirical support for the WHO analgesic ladder is robust, the generalizability of its efficacy across diverse cultural cohorts-particularly those exhibiting somatic expression of distress-is inadequately addressed in the literature. The implicit assumption of patient self-reporting as a reliable metric warrants critical reevaluation.