Orthostatic Hypotension Risk Calculator
How Likely Are You to Experience Dizziness When Standing?
This tool helps you understand your risk of orthostatic hypotension based on medications you're taking and other factors. Results are based on clinical research and the information provided in our article.
Your Risk Assessment
Recommendations
Standing up and feeling like the room is spinning? That sudden wave of dizziness, blurred vision, or even fainting isn’t just bad luck-it could be your medications. This isn’t rare. In fact, orthostatic hypotension from drugs is one of the most common, yet overlooked, side effects in older adults and people taking multiple prescriptions. It’s not just annoying-it’s dangerous. Every year, tens of thousands of falls, hospital visits, and even deaths are tied to this simple, preventable reaction to standing up too fast.
What Exactly Is Orthostatic Hypotension?
Orthostatic hypotension, also called postural hypotension, is when your blood pressure drops sharply the moment you stand. The medical definition is clear: a systolic drop of 20 mm Hg or more, or a diastolic drop of 10 mm Hg or more, within three minutes of standing. That’s not a small fluctuation. That’s enough to starve your brain of blood for a few critical seconds. The result? Dizziness, lightheadedness, tunnel vision, nausea, or worse-passing out.It’s not a disease itself. It’s a warning sign. Your body normally compensates for standing by tightening blood vessels and speeding up your heart to keep blood flowing to your brain. When medications interfere with that system, the balance breaks. And in many cases, it’s not the aging process-it’s the pills.
Which Medications Cause This?
Not all drugs do this. But some are notorious. If you’re taking any of these, your risk goes up significantly:- Antipsychotics-especially clozapine, quetiapine, and chlorpromazine. Up to 40% of people on these report dizziness on standing. One Reddit user shared, “After starting quetiapine for anxiety, I fainted twice within three weeks.”
- Tricyclic antidepressants-like amitriptyline and nortriptyline. These block nerve signals that help control blood pressure. Studies show they raise OH risk by over 3 times.
- Alpha-blockers-used for high blood pressure and enlarged prostate. Drugs like doxazosin and terazosin relax blood vessels so hard they can’t react fast enough when you stand.
- Diuretics-water pills like hydrochlorothiazide. They reduce blood volume, making it harder to maintain pressure when upright.
- Opioids-morphine, oxycodone, hydrocodone. About 1 in 5 elderly patients on these experience dizziness. The risk doubles if you’re also taking benzodiazepines or drinking alcohol.
- Levodopa-used for Parkinson’s. Up to half of patients on this drug develop orthostatic hypotension because it affects the autonomic nervous system.
Here’s the kicker: many of these drugs are prescribed for legitimate, serious conditions. But when you’re on four, five, or six medications-which is common in people over 70-their effects stack up. People taking four or more drugs have nearly six times the risk of OH compared to those on one or two.
Why Does This Happen?
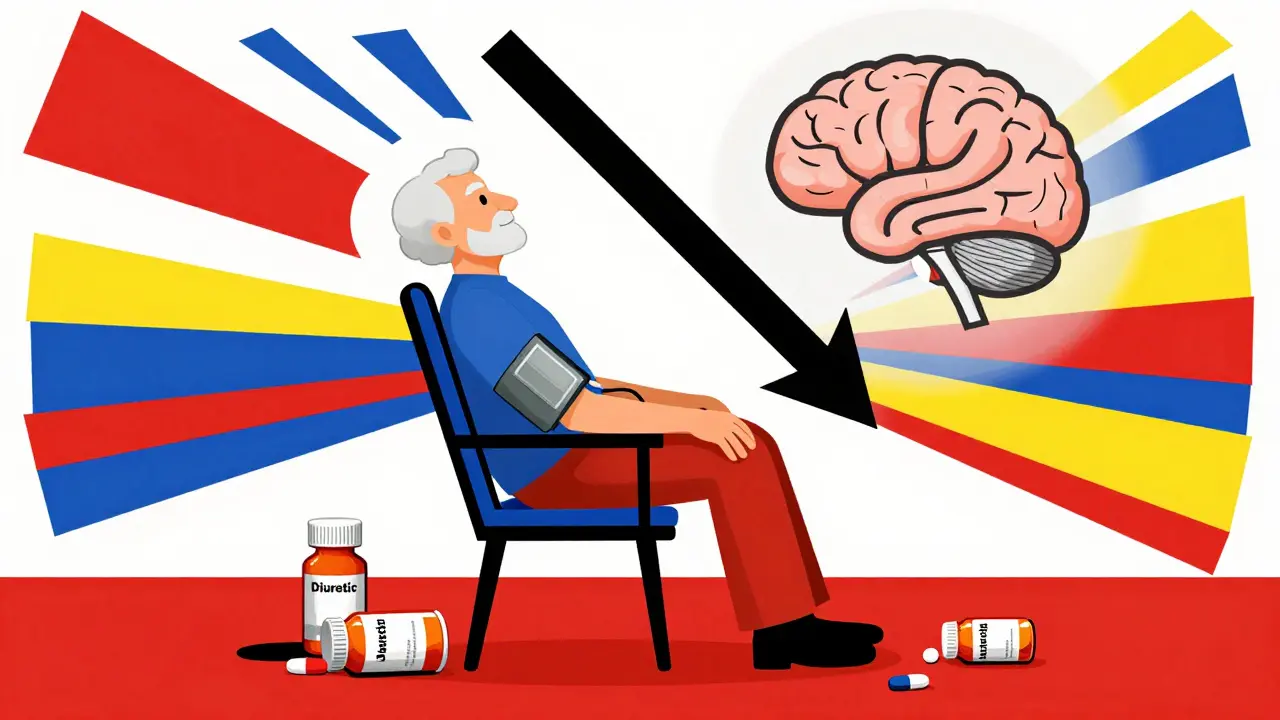
Your body has a built-in system to keep blood pressure steady when you move. When you stand, gravity pulls blood down into your legs. Sensors in your neck (baroreceptors) detect the drop and signal your heart to beat faster and your blood vessels to tighten. That’s how you stay upright without passing out.Medications disrupt this in different ways:
- Alpha-blockers stop blood vessels from tightening.
- Diuretics reduce total fluid in your system, so there’s less blood to pump.
- Antidepressants and antipsychotics interfere with nerve signals that tell your body to react.
- Opioids depress the central nervous system, slowing the reflex response.
It’s not just about the drug itself-it’s about timing, dosage, and your body’s ability to adapt. Older adults naturally have slower reflexes. Combine that with a medication that blunts your body’s natural response, and you’ve got a recipe for dizziness.
Who’s Most at Risk?
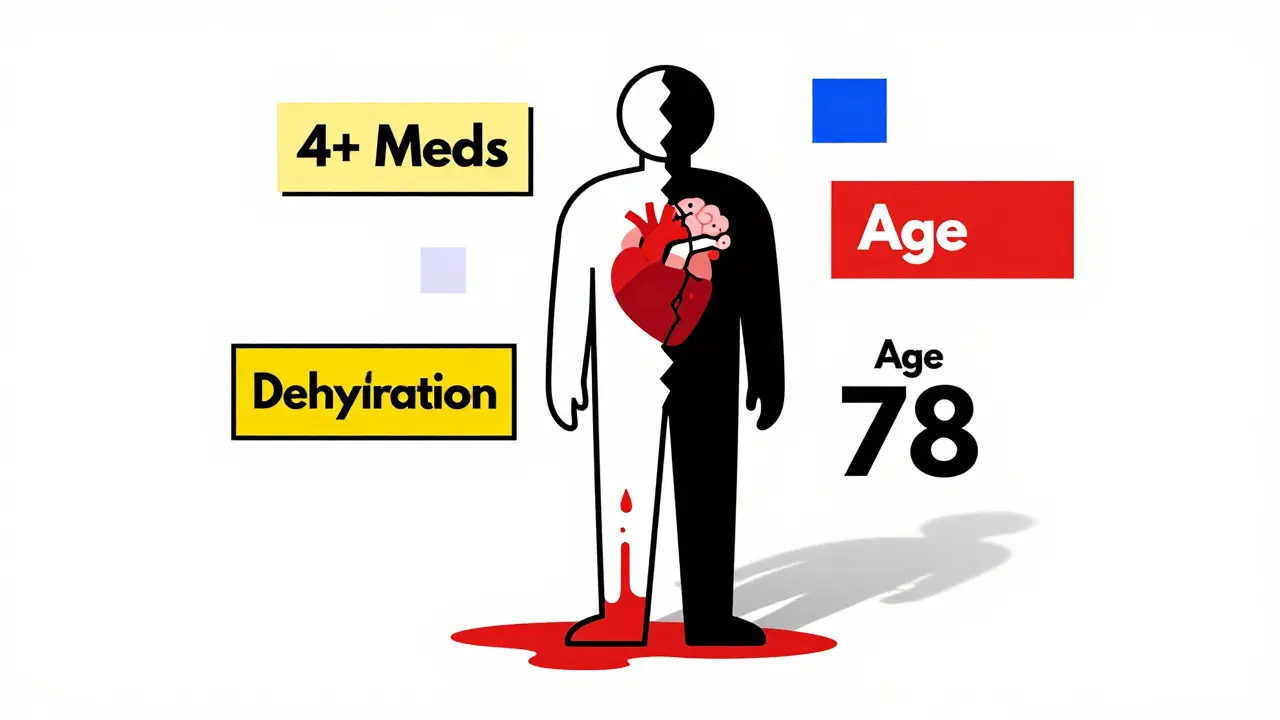
It’s not just seniors, though they’re most affected. Here’s who’s most vulnerable:- People over 70-3.2 times more likely than younger adults.
- Those on four or more medications-5.7 times higher risk.
- People with diabetes, Parkinson’s, or heart failure-these conditions already stress the autonomic nervous system.
- People who are dehydrated-even mild dehydration makes OH worse.
Here’s a real case: a 78-year-old woman on hydrochlorothiazide (a diuretic) and lisinopril (a blood pressure pill) kept falling. Her doctor thought it was aging or balance issues. Turns out, removing the diuretic resolved her dizziness completely in under 72 hours. That’s how powerful medication adjustment can be.
How Is It Diagnosed?
It’s simple, but often skipped. Your doctor should check your blood pressure while you’re lying down, then again after you stand up. The standard is to measure at 1, 2, and 3 minutes after standing. If your systolic pressure drops 20 points or more, and you feel dizzy at the same time-you have medication-induced orthostatic hypotension.Here’s the problem: many doctors don’t check. In one Mayo Clinic study, 55% of patients had symptoms for over two months before anyone connected it to their meds. If you’re feeling dizzy when you stand, say something. Don’t assume it’s normal.
What Can You Do About It?
The good news? This is often fixable. In 65-80% of cases, symptoms improve or disappear after adjusting medications. Here’s how:- Review your meds-Talk to your doctor or pharmacist. Ask: “Could any of these be causing dizziness when I stand?” Don’t stop anything on your own, but do ask if a lower dose or alternative drug is possible.
- Stand up slowly-Pause for 10-15 seconds after sitting up before standing. Sit on the edge of the bed for a moment. Use a cane or handrail if needed.
- Hydrate-Drink 2-2.5 liters of water daily. Dehydration makes OH worse. A glass of water before standing can help.
- Wear compression stockings-These help push blood back up from your legs. They’re not glamorous, but they work.
- Avoid alcohol and large meals-Both can lower blood pressure further.
- Consider midodrine-If lifestyle changes aren’t enough, your doctor might prescribe midodrine, a drug that tightens blood vessels. It’s not a first-line fix, but it helps 65% of patients who still struggle.
One Stanford Healthcare study found 78% of patients felt significantly better within one to two weeks after adjusting their meds. That’s not a miracle-it’s smart medicine.
Why This Matters More Than You Think
This isn’t just about feeling dizzy. Orthostatic hypotension increases your risk of falls by 15-30%. Falls lead to fractures, hospital stays, loss of independence, and even death. In 2022, falls related to OH cost Medicare $31 billion. About a third of those costs came from drug-induced cases.And it’s getting worse. By 2040, nearly 81 million Americans will be over 65. More people on more drugs means more cases of OH. That’s why the American Geriatrics Society now lists 12 high-risk medications in their Beers Criteria-and why FDA labels now include OH warnings if a drug causes it in more than 5% of users.
What’s Next?
Researchers are working on better tools. Some are testing genetic tests to predict who’s more likely to develop OH from certain drugs. Others are designing new medications that treat conditions like high blood pressure or depression without affecting blood pressure control. In the meantime, awareness is your best defense.If you or someone you care about is taking multiple medications and feels lightheaded when standing, don’t ignore it. Don’t assume it’s just getting older. Ask for a medication review. Ask for blood pressure checks in both positions. Small changes can prevent big problems.
Can orthostatic hypotension go away on its own?
Yes, in many cases. If the cause is medication-related, adjusting or stopping the drug often resolves symptoms within days to weeks. For example, removing a diuretic or lowering the dose of an alpha-blocker can lead to full recovery in 65-80% of patients. However, if OH is caused by nerve damage from diabetes or Parkinson’s, it’s less likely to resolve without treatment.
Is dizziness when standing always a sign of something serious?
Not always-but it shouldn’t be ignored. Mild, occasional dizziness might be due to dehydration or standing too fast. But if it happens regularly, especially with vision changes, nausea, or near-fainting, it’s a red flag. Up to 40% of people with orthostatic hypotension have no symptoms, but those who do are at higher risk of falls and long-term complications.
Can I still take my blood pressure medication if I have orthostatic hypotension?
Yes, but the type and dose may need to change. Some blood pressure drugs are more likely to cause OH than others. For example, diuretics and alpha-blockers are higher risk, while ACE inhibitors like lisinopril are less likely to cause it. Your doctor can switch you to a safer option or lower the dose while still controlling your blood pressure.
How long does it take for dizziness to improve after stopping a medication?
It varies. For short-acting drugs like certain diuretics or alpha-blockers, symptoms can improve within 24-72 hours. For longer-acting drugs or those that affect nerve function (like antidepressants), it may take one to two weeks. Always follow your doctor’s advice on tapering-never stop suddenly without medical guidance.
Are there any home tests I can do to check for orthostatic hypotension?
Yes. Use a home blood pressure monitor. Lie down for five minutes, take your reading, then stand up slowly. Wait three minutes and take another reading. If your systolic pressure drops 20 mm Hg or more, and you feel dizzy at the same time, you likely have orthostatic hypotension. Write down the numbers and show them to your doctor. It’s a simple step that can save you from a fall.
Comments (14)
Christina Widodo
January 12, 2026 AT 01:48
I used to get dizzy every time I stood up after starting amitriptyline-thought it was just me being clumsy. Turns out, it was the med. My doctor didn’t even ask about it until I brought it up. Now I’m on something else and I haven’t fallen in months.
Sona Chandra
January 12, 2026 AT 01:59
THIS IS WHY PEOPLE DIE IN NURSING HOMES. DOCTORS JUST PRESCRIBE LIKE THEY’RE BUYING GROCERIES. MY GRANDMA WAS ON 8 DRUGS AND THEY NEVER CHECKED HER BP WHEN SHE STOOD UP. SHE BROKE HER HIP AND NO ONE CARED. THIS IS MURDER BY MEDICATION.
Alice Elanora Shepherd
January 12, 2026 AT 16:13
It’s remarkable how often this is dismissed as ‘just aging.’ I’ve seen patients in my clinic who’ve been dizzy for over a year-no one thought to check orthostatic vitals. The 20/10 mmHg drop is a hard diagnostic threshold, but even smaller drops with symptoms matter. Always document standing BP-it’s a 30-second test that can prevent a lifetime of consequences.
Lauren Warner
January 12, 2026 AT 22:16
Let’s be real-this is just another example of pharmaceutical companies pushing drugs with known side effects because they’re profitable. Alpha-blockers? Diuretics? They’ve been around for decades. The fact that we’re still not screening for OH routinely shows how broken our system is. And don’t get me started on how doctors blame patients for ‘not moving slowly enough.’
Rinky Tandon
January 13, 2026 AT 16:23
Look, if you're over 70 and on more than 3 meds, you're basically a walking pharmacology experiment. The autonomic nervous system isn't some magical system-it's a fragile network of receptors and neurotransmitters that get wrecked by polypharmacy. Your doctor doesn't care because they're paid per script, not per outcome. You're a statistic. And you're going to fall.
Jennifer Phelps
January 15, 2026 AT 05:16
My mom had this after starting hydrochlorothiazide. We didn't know what it was until she passed out in the kitchen. Took us three months to connect it to the med. The doctor said 'it's common in seniors' like that was an excuse. It's not normal it's dangerous
beth cordell
January 17, 2026 AT 00:14
Compression socks are a game changer 🧦 I know they look boring but I wear mine every morning and I haven't had a dizzy spell since. Also drink water like your life depends on it 💧 (it kinda does)
Bryan Wolfe
January 18, 2026 AT 19:04
Thank you for writing this. So many people suffer in silence thinking it’s just ‘getting older.’ I’ve coached older patients through med reviews and the difference is night and day. One lady stopped her diuretic and started walking her dog again-she cried because she hadn’t felt safe standing up in years. Small changes save lives.
Katherine Carlock
January 20, 2026 AT 13:23
I’m a nurse and I can’t tell you how many times I’ve seen this. Someone comes in after a fall, and the first thing we do is check their med list. Nine times out of ten, it’s a combo of an alpha-blocker and a diuretic. We need to make standing BP checks routine-not optional. It’s not rocket science.
Lelia Battle
January 21, 2026 AT 15:24
There’s a deeper philosophical question here: when medicine becomes a system of managing symptoms rather than restoring balance, we lose sight of the body’s innate wisdom. Orthostatic hypotension isn’t an isolated event-it’s a systemic signal. The body is asking us to reconsider the weight of our interventions. Perhaps the most effective treatment is not another drug, but a pause.
Prachi Chauhan
January 23, 2026 AT 08:13
so like if you're on meds and you feel like you're gonna pass out when you stand... it's probably the pills? wow. who knew. also i'm from india and my grandma took like 10 pills a day and no one ever checked her bp when she stood up. everyone just said oh she's old. but she was fine until the falls started. now she's on one med and walks without a cane. it's not magic it's common sense
Craig Wright
January 24, 2026 AT 08:54
As a British man who has spent decades in the NHS, I find it deeply concerning that this issue is still being treated as an afterthought. In our system, we are supposed to be proactive. Yet here we are, allowing elderly patients to be medicated into fragility. This is not medical care-it is negligence dressed in white coats. The Beers Criteria exist for a reason. Use them.
laura manning
January 26, 2026 AT 01:43
It is imperative to underscore that the diagnostic criteria for orthostatic hypotension, as delineated by the American Heart Association and the American College of Cardiology, require standardized measurement protocols. Failure to obtain supine and standing readings at one, two, and three minutes post-stand constitutes a diagnostic omission of significant clinical consequence. Moreover, the temporal relationship between symptom onset and medication initiation must be rigorously evaluated in all cases of suspected drug-induced orthostatic hypotension.
steve ker
January 27, 2026 AT 13:30
Wow. So many words. Just stop the meds if you feel dizzy. Done. Also why are you on so many pills anyway? You’re not a pharmacy.