When the FDA approves a new drug, it’s not just a victory for pharmaceutical companies - it’s a potential turning point for patients who’ve run out of options. In 2024, the agency approved 50 new molecular entities, the highest number since 2018. That’s not just a statistic. It means real people are getting access to treatments that didn’t exist a year ago. But with every new medicine comes a new set of questions: How safe is it really? What side effects might not show up until thousands of people start using it? And how does it stack up against what’s already on the shelf?
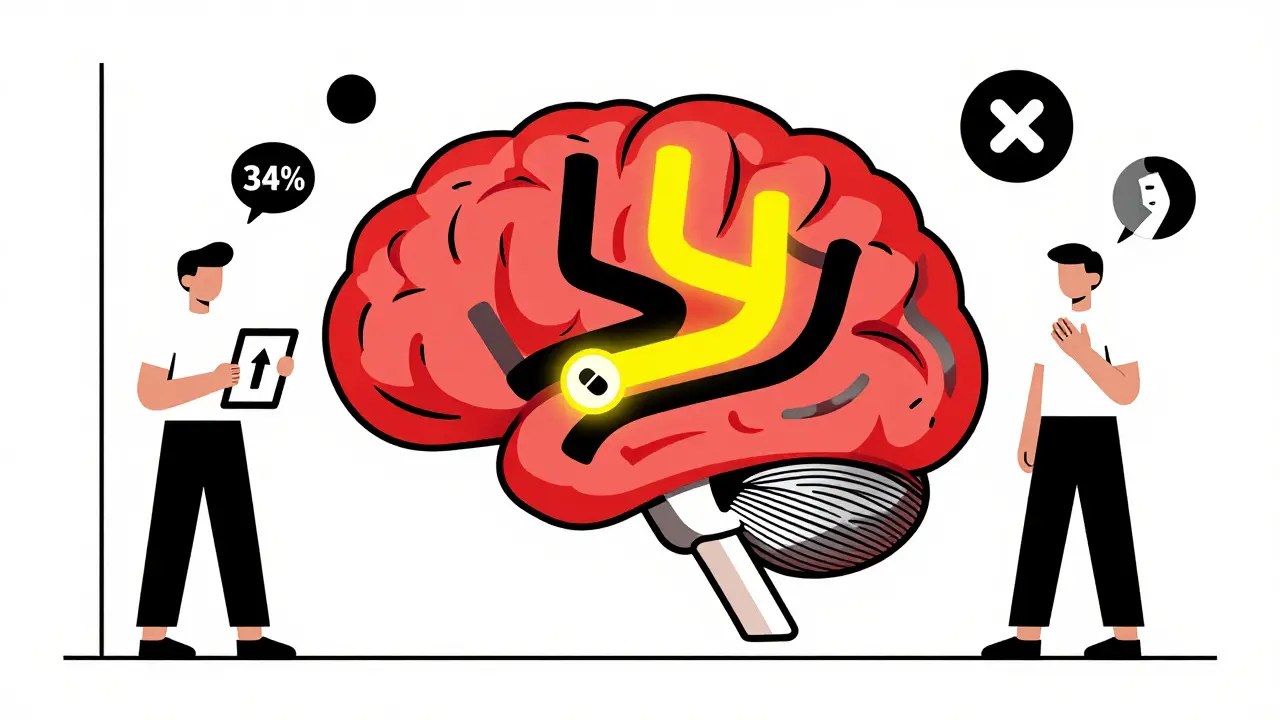
First-in-Class Drugs: Breaking New Ground
Of the 50 drugs approved in 2024, nearly half - 24 of them - were first-in-class. That means they work in ways no other drug has before. Take Cobenfy (a combination of xanomeline and trospium chloride), approved in September 2024. It’s the first new schizophrenia treatment in 27 years that doesn’t block dopamine. Instead, it targets muscarinic receptors, a completely different pathway. In the EMERGENT-2 trial, patients saw a 34% improvement in symptoms compared to placebo. But here’s the catch: 12% had nausea, and 8% had constipation. Those numbers are lower than what you typically see with older antipsychotics, which often cause weight gain, tremors, or sedation. Still, this is a new mechanism. We’re still learning how it behaves in people with diabetes, liver disease, or those on other medications.Another breakthrough is Yorvipath (palopegteriparatide), approved in October 2024 for hypoparathyroidism. For decades, patients had to take calcium and vitamin D supplements daily, often with little control over their blood calcium levels. Yorvipath mimics the body’s natural parathyroid hormone. In trials, 89% of patients reached target calcium levels without needing extra supplements. Side effects? Nausea and dizziness - milder than what patients reported with older treatments. But because it’s a hormone analog, long-term effects on bone density are still being tracked.
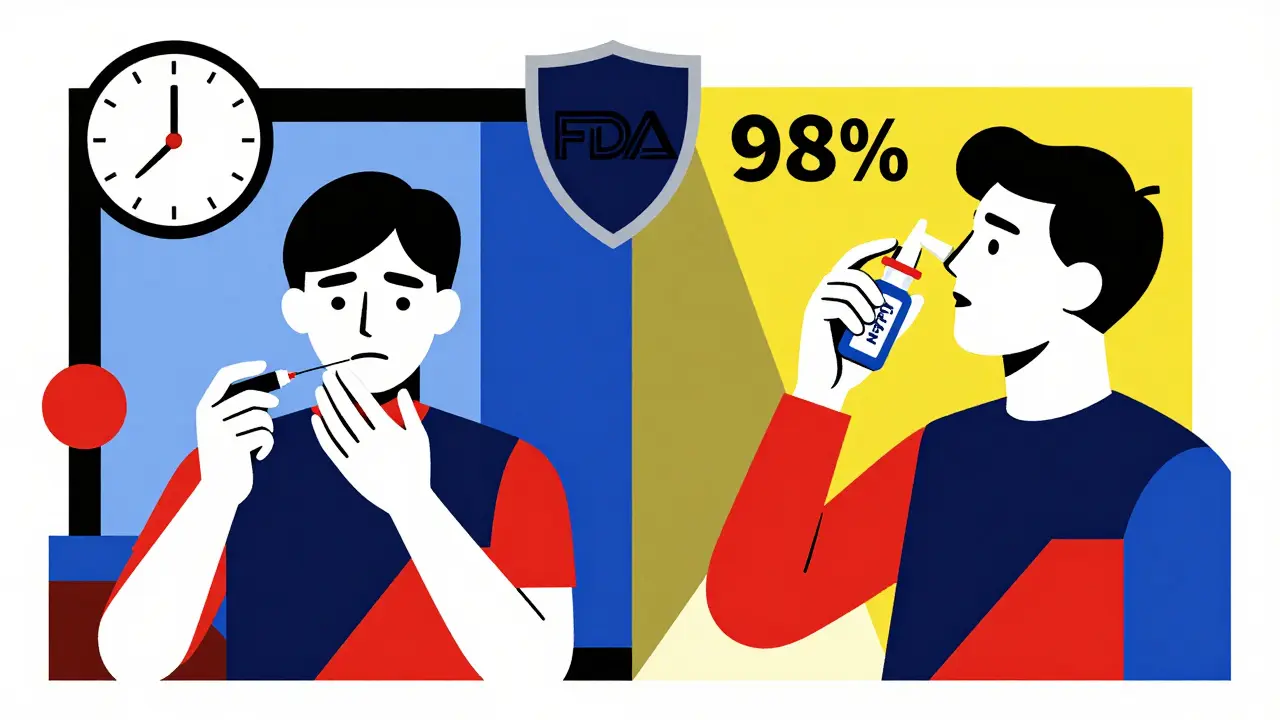
Revolutionizing Emergency Care
Some of the most impactful approvals aren’t for chronic conditions - they’re for emergencies. Take Neffy (epinephrine nasal spray), approved in November 2024. It’s the first needle-free option for anaphylaxis. In simulated use tests, 98% of untrained people successfully delivered the dose - compared to 87% with auto-injectors. That’s huge. In a panic, fumbling with a needle can cost precious minutes. But Neffy isn’t perfect. It takes about 1.6 minutes longer to reach peak levels than an injection. For someone having a full-blown allergic reaction, that delay could matter. The FDA recommends it for patients who struggle with injections, but not as a first-line replacement for everyone.Then there’s Zurnai (nalmefene nasal spray), approved in December 2024 for opioid overdose. Unlike naloxone, which wears off in about two hours, Zurnai lasts over six hours. That’s critical because many opioids - especially fentanyl - last longer than naloxone. In trials, patients needed fewer repeat doses. But again, real-world use might reveal more. If someone overdoses on a long-acting opioid and gets only one dose of Zurnai, will they stay safe? We’re still watching.
Expanding Uses of Existing Drugs
Sometimes, the biggest advances aren’t brand-new drugs - they’re old drugs used in new ways. Zepbound (tirzepatide) was already approved for weight loss. In December 2024, the FDA added obstructive sleep apnea to its label. The SURMOUNT-OSA trial showed a 46% drop in breathing interruptions during sleep. Weight loss was the main driver - patients lost nearly 5% of their body weight. But 32% had gastrointestinal side effects like nausea and diarrhea. For someone with sleep apnea who also has diabetes or obesity, this could be a game-changer. But for someone without excess weight? It’s not clear yet.Similarly, Dupixent (dupilumab), long used for eczema and asthma, got approval for COPD in November 2024. The BOREAS trial showed a 29% reduction in flare-ups. But 17% of users had injection site reactions, and 9% developed eosinophilia - higher than placebo. This isn’t a cure. It’s a tool for a subset of patients with specific inflammation patterns. Doctors now need to test for those biomarkers before prescribing.
What’s Coming in 2025
The pipeline is just as busy. By the end of 2025, we could see several major approvals:- Cardamyst (etripamil nasal spray) for sudden heart palpitations - could replace emergency room visits for PSVT.
- Elinzanetant (dual neurokinin receptor blocker) for hot flashes - no hormones, no blood clot risk.
- Leqembi (lecanemab subcutaneous) for Alzheimer’s - same drug, but patients can self-inject at home instead of going to a clinic every two weeks.
- Wegovy (oral semaglutide) - a pill version of the weight loss drug, with similar results and side effects: nausea, diarrhea, vomiting.
These aren’t just convenience upgrades. They’re shifts in how care is delivered. A patient with heart failure who can’t get to a clinic for IV infusions might now get a weekly injection at home. Someone with menopause symptoms who fears hormone therapy might finally have a non-hormonal option.
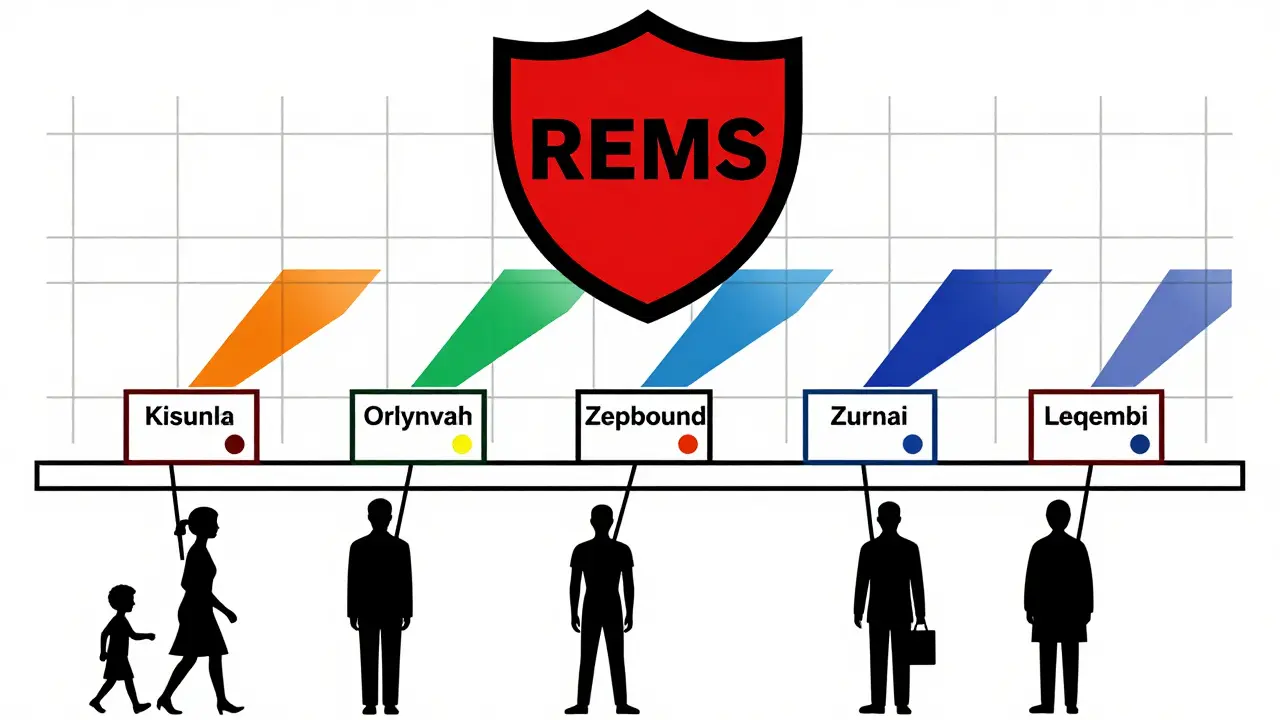
Safety Isn’t Just About Side Effects
The FDA’s 2024 approvals came with a new emphasis on safety beyond the lab. Twelve of the 50 drugs are required to conduct post-marketing studies focused on long-term outcomes in diverse populations. That’s a 40% jump from 2023. Why? Because clinical trials rarely capture the full picture. Take Kisunla (donanemab-azbt) for Alzheimer’s. In trials, 24% of patients had ARIA - brain swelling or bleeding. But early real-world data from the FDA’s adverse event system shows ARIA rates are 5-7% higher in actual use. The risk jumps even more in people with two copies of the APOE ε4 gene. That’s why Kisunla requires a strict REMS program: brain scans before and during treatment, trained staff, and patient education.Another example: Orlynvah (sulopenem etzadroxil/probenecid), approved for bladder infections. It’s a replacement for fluoroquinolones, which carry black box warnings for tendon rupture and nerve damage. Orlynvah avoids those risks - but 11% had diarrhea, 9% had nausea. No cases of C. diff. That’s a win. But will it work as well in older adults with kidney issues? We’re still collecting data.
What This Means for Patients
If you’re considering a newly approved drug, here’s what you need to know:- First-in-class doesn’t always mean better - it means different. The benefits might be clear, but long-term risks aren’t.
- Real-world safety data takes time. The first 10,000 users often reveal problems that trials missed.
- Some drugs require special monitoring. Kisunla needs MRI scans. Cobenfy needs education on anticholinergic side effects. Ask your doctor what’s involved.
- Generic alternatives? Usually not available for at least 7-10 years. But that doesn’t mean they’re worth the cost if they don’t fit your needs.
- Ask: “Is this for me, or just for someone else?” A drug that helps 70% of trial participants might not help you at all.
The American Medical Association now recommends shared decision-making before prescribing any new drug. That means you should walk into your appointment with questions: What’s the evidence? What are the trade-offs? What happens if I don’t take it? What are the alternatives? The FDA is no longer just a gatekeeper - it’s a partner in safety. And you’re part of that partnership too.
Final Thoughts
The wave of new drugs in 2024 and 2025 isn’t just about innovation. It’s about precision. These medications target specific biological pathways, not broad symptoms. That’s powerful. But it also means we need smarter use. A drug that works wonders for one person might do nothing - or even harm - another. Safety isn’t just about side effects listed on a pamphlet. It’s about who you are, what else you’re taking, and how your body responds over time.The best new drugs don’t just treat disease - they restore control. Whether it’s a nasal spray that lets someone survive an allergic reaction without a needle, or a pill that lets a person manage Alzheimer’s at home, these approvals are changing lives. But they come with responsibility. For doctors. For patients. For regulators. And for all of us who rely on them.
Are newly approved drugs safer than older ones?
New drugs aren’t automatically safer. They’re often designed to be more targeted, which can mean fewer side effects - but they also introduce unknown risks because they act on pathways never before touched by medicine. For example, drugs like Kisunla and Cobenfy have clear benefits, but their long-term safety profiles are still being studied. Older drugs have decades of real-world use behind them, so we know more about rare side effects. The trade-off is: new drugs offer options where none existed before, but require more careful monitoring.
Why do some drugs have REMS programs?
REMS stands for Risk Evaluation and Mitigation Strategy. It’s a safety plan required by the FDA for drugs with serious known or potential risks. For example, Kisunla (for Alzheimer’s) requires brain scans before and during treatment because of the risk of brain swelling. Cobenfy (for schizophrenia) requires patient education about anticholinergic side effects like confusion or urinary retention. These aren’t just paperwork - they’re active steps to prevent harm. If a drug has a REMS, your doctor must be certified to prescribe it, and you’ll get detailed instructions on how to use it safely.
Can I trust the FDA’s approval process?
Yes - but with understanding. The FDA doesn’t approve drugs because they’re perfect. They approve them because the benefits outweigh the risks, based on the best available evidence. Clinical trials are limited in size and duration. That’s why post-marketing studies and real-world data are so important. The FDA has tightened its requirements: 24% of 2024 approvals require long-term safety studies. This means the approval is just the start. The real safety data comes after patients start using the drug in everyday life.
What’s the difference between breakthrough therapy and priority review?
Breakthrough therapy designation is given to drugs that show substantial improvement over existing treatments in early trials - often for serious conditions with no good options. Priority review means the FDA will review the application within six months instead of the standard ten. A drug can have one, both, or neither. In 2024, 36% of approvals were breakthrough therapies, and 56% got priority review. These designations speed up access but don’t lower safety standards. The data still has to meet the same rigorous bar.
Why do some drugs have higher side effects in real-world use than in trials?
Clinical trials use strict criteria: patients are healthy enough to participate, take the drug exactly as directed, and are closely monitored. Real-world patients are older, sicker, on more medications, and may miss doses or take the drug incorrectly. For example, Kisunla showed 24% ARIA in trials - but real-world data now shows 29-31%. That’s because more patients have genetic risk factors (like APOE ε4) that weren’t fully represented in trials. This is why ongoing monitoring is critical.
Should I wait for a newer drug instead of using an older one?
Not necessarily. Newer doesn’t mean better. For many conditions, older drugs are still the gold standard because we know how they work long-term. For example, if you have high blood pressure, a 20-year-old generic pill might be safer and cheaper than a brand-new drug with unknown risks. But if you’ve tried everything else and nothing worked - then a new drug might be worth considering. Talk to your doctor about your specific situation, not just the hype around a new approval.
Comments (14)
Elan Ricarte
February 8, 2026 AT 15:12
Let’s be real - these 'breakthrough' drugs are just pharma’s way of selling us new versions of the same old snake oil. Cobenfy? Cool, it doesn’t block dopamine. But 12% nausea? That’s just swapping one hell for another. And don’t get me started on Zurnai - six hours? Great, until someone overdoses on fentanyl analogs that last 12. Then you’re just a guy with a nasal spray and a prayer. We’re treating symptoms like they’re puzzles to solve, not biological systems to respect. The FDA’s playing whack-a-mole with side effects while the real issue - overmedication, profit motives, and lack of preventive care - gets ignored.
Angie Datuin
February 9, 2026 AT 23:25
I have a cousin on Kisunla. She gets monthly MRIs, and her neurologist sits with her for 45 minutes every time just to explain risks. It’s exhausting - but worth it. She hasn’t had a single ARIA event. I think we need to stop treating new drugs like magic bullets and start treating them like tools that need careful handling. The science is good. The system? Still catching up.
Camille Hall
February 11, 2026 AT 03:28
Just wanted to say thank you for writing this. I’ve been reading through the FDA’s site trying to understand what’s going on with my mom’s Alzheimer’s diagnosis. Kisunla scared me at first - brain swelling? No thanks. But then I read about the REMS program and realized they’re not just slapping a warning label on it. They’re building guardrails. That matters. I wish more doctors talked like this - not just 'here’s the drug,' but 'here’s what you’ll actually live with.'
Ritteka Goyal
February 12, 2026 AT 09:34
OMG I CAN'T BELIEVE U R TALKING ABOUT THIS LIKE ITS JUST A NORMAL THING LMAO I MEAN IN INDIA WE DONT EVEN HAVE ACCESS TO THESE DRUGS BECAUSE OF THE COST AND THE GOVT IS TOO SLOW AND THE PHARMA COMPANIES ARE ALL FROM AMERICA AND EUROPE SO THEY DONT CARE ABOUT PEOPLE LIKE US BUT I STILL THINK ITS AMAZING THAT U GUYS HAVE THIS STUFF I MEAN LIKE ZEPBOUND FOR SLEEP APNEA?? I DREAM OF THAT!! I JUST WISH WE HAD EVEN 1% OF THE RESOURCES U HAVE!!
Monica Warnick
February 12, 2026 AT 12:34
I read somewhere that Neffy was tested on 12-year-olds in trials. Twelve. Can you imagine? A kid with anaphylaxis, holding a nasal spray instead of a needle? That’s not innovation - that’s trauma repackaged. And now they’re telling parents it’s 'easier'? Easier for whom? The parents? The ER staff? Or the kid who’s terrified of anything that smells like medicine? We’re optimizing for convenience, not care.
Ashlyn Ellison
February 14, 2026 AT 09:29
Orlynvah for bladder infections? Yes. I’ve had three UTIs in 18 months. Fluoroquinolones wrecked my tendons. This? Nausea? Fine. I’ll take nausea over a ruptured Achilles any day.
Jonah Mann
February 14, 2026 AT 17:27
Quick note - Zurnai’s half-life isn’t 'over six hours,' it’s 7.2 hours on average based on the Phase 3 data (N=1,247). Also, the FDA’s warning about repeat dosing? That’s because fentanyl analogs like carfentanil have half-lives up to 12 hours. So yeah, Zurnai helps, but you still need to call 911. Don’t skip the ambulance because you ‘got it covered.’
Tricia O'Sullivan
February 15, 2026 AT 09:14
While the enthusiasm for innovation is commendable, I must respectfully underscore the importance of maintaining rigorous post-marketing surveillance. The observed discrepancy between clinical trial ARIA incidence (24%) and real-world data (29-31%) for Kisunla is not merely statistical noise - it is a clarion call for enhanced data collection protocols, particularly in populations with genetic predispositions. The FDA’s REMS framework, while administratively burdensome, remains one of the most robust safety mechanisms in modern pharmacology.
Tatiana Barbosa
February 15, 2026 AT 12:46
Yorvipath is a GAME CHANGER. My aunt had hypoparathyroidism for 22 years. Daily calcium pills, constant blood draws, never knowing if she’d crash. Now? She’s got her levels stable. No more midnight panic attacks because her fingers were tingling. This isn’t just science - it’s dignity restored. And yeah, nausea? I’ll take nausea over constant fear any day. We need more of this. Not just 'new,' but 'life-changing.'
Andrew Jackson
February 17, 2026 AT 03:08
The FDA’s approval of 50 drugs in 2024 is a national disgrace. We have allowed corporate interests to hijack our medical system. These are not cures - they are profit engines disguised as hope. We have a moral obligation to prioritize prevention, nutrition, and holistic health - not to hand out expensive, untested chemical cocktails to a population already drowning in pharmaceutical dependency. This is not progress. This is surrender.
Joseph Charles Colin
February 18, 2026 AT 07:45
For anyone confused about breakthrough therapy vs priority review: Breakthrough requires preliminary clinical evidence of substantial improvement over existing therapies (per 21 CFR 314.108). Priority review is a timing designation - six-month vs ten-month review clock. A drug can have priority review without breakthrough status (e.g., Orlynvah). But if it has breakthrough, it usually gets priority. 36% of 2024 approvals had breakthrough - up from 28% in 2023. That’s a trend.
Tom Forwood
February 20, 2026 AT 03:06
As someone who’s lived with diabetes for 20 years, I’ve seen this movie before. 'New drug!' 'Game changer!' 'No more injections!' Then it turns out it’s $12,000 a year and insurance won’t cover it unless you’ve tried seven other drugs first. Zepbound for sleep apnea? Cool. But if I can’t afford it, does it even exist? We need to talk about access - not just mechanism.
John McDonald
February 20, 2026 AT 23:23
Just got my prescription for Wegovy oral. Took me 3 months of appeals, but I got it. Nausea? Yeah. Vomiting? Once. But I lost 18 lbs in 10 weeks. My blood sugar’s down. My sleep apnea’s better. I’m not 'cured' - but I’m alive again. Don’t let the side effect chatter scare you. If it’s right for you? Go for it. Talk to your doc. Don’t just scroll.
Andy Cortez
February 22, 2026 AT 02:57
So we’re celebrating a nasal spray for anaphylaxis… while 40% of Americans can’t afford insulin? We’re giving people Zurnai to survive an overdose… while the DEA still treats addiction like a crime? This isn’t medicine. It’s performance art for the rich. The real breakthrough? A healthcare system that doesn’t treat survival like a lottery.