Multiple sclerosis isn’t just a brain or spine problem-it’s your immune system turning on itself. Imagine your nerves are like electrical wires, wrapped in a protective insulation called myelin. Now picture your body’s defense system, which is supposed to fight off viruses and bacteria, mistakenly tearing that insulation apart. That’s multiple sclerosis (MS). It’s not cancer. It’s not an infection. It’s an autoimmune neurological disease where your own cells become the enemy.
What Actually Happens Inside Your Body With MS?
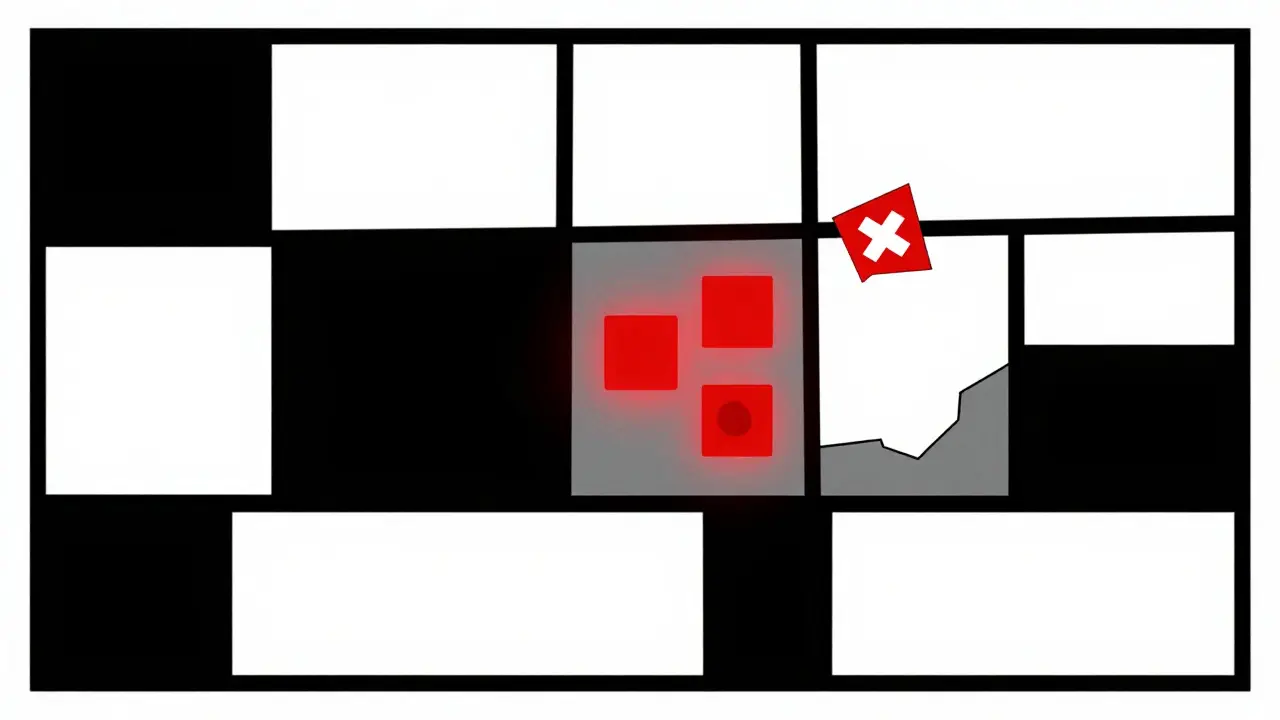
Your central nervous system-your brain and spinal cord-relies on myelin to send signals fast. Myelin lets nerve impulses zip along at speeds up to 120 meters per second. When MS attacks, the immune system sends T-cells and antibodies into the brain and spine. They target myelin, causing inflammation. Over time, the damaged areas harden into scar tissue, or plaques. These scars disrupt signals. A simple thought like “lift your foot” might not reach your leg. Or your hand might feel numb when you know you didn’t touch anything cold.
Doctors see these scars on MRI scans. Gadolinium dye highlights active inflammation-bright spots showing where the attack is happening right now. In relapsing-remitting MS, the most common form, these flare-ups come and go. But even when symptoms fade, damage keeps building. That’s why early treatment matters.
Who Gets MS-and Why?
Most people are diagnosed between ages 20 and 40. Women are two to three times more likely to be diagnosed than men. It’s not just gender. Geography plays a huge role. If you live near the equator, your risk is low-about 30 in 100,000. But if you’re in Canada, Scotland, or Scandinavia, that number jumps to 300 in 100,000. Sunlight exposure and vitamin D levels are strongly linked. People with vitamin D below 30 ng/mL have a 40% higher risk.
Genetics also matter. Over 230 gene variants are tied to MS risk. The biggest one, HLA-DRB1*15:01, triples your chance if you carry it. But genes alone don’t cause MS. Something else has to trigger it. The strongest suspect? Epstein-Barr virus-the virus that causes mononucleosis. A 2022 Harvard study found people who had infectious mononucleosis were 32 times more likely to develop MS later. Not everyone who gets mono gets MS, but nearly all MS patients have had EBV.
The Four Types of MS-and What They Mean
MS isn’t one disease. It’s four different patterns of progression.
- Clinically Isolated Syndrome (CIS): A single neurological episode-like sudden vision loss or leg weakness-that lasts at least 24 hours. If MRI shows lesions, 60-80% will go on to develop full MS within 10 years.
- Relapsing-Remitting MS (RRMS): The most common starting point-85% of cases. People have clear flare-ups (relapses) followed by periods of recovery (remission). Without treatment, they average 0.5 to 1 relapse per year.
- Secondary Progressive MS (SPMS): After 10 to 25 years, about half of RRMS patients start declining steadily, even without flare-ups. This isn’t a sudden switch-it’s a slow creep of worsening function.
- Primary Progressive MS (PPMS): 15% of cases. No relapses. Just steady decline from day one. Walking gets harder. Balance fades. Progression is slower than RRMS but relentless.
These aren’t just labels. They determine treatment. Drugs that work for RRMS often don’t help PPMS. That’s why getting the right diagnosis matters.
What Symptoms Do People Really Experience?
MS symptoms vary wildly. No two people have the same mix. But some show up over and over.
- Chronic fatigue: 78% of people with MS say it’s their worst symptom. Not just tired. Exhausting, bone-deep, doesn’t go away with sleep. One Reddit user described it as “feeling like you’re dragging a concrete block through your day.”
- Brain fog: Trouble finding words, forgetting names, losing focus. u/MSWarrior2020 posted on Reddit: “I know what I want to say. My mouth just won’t form the words.” That post got over 1,200 upvotes.
- Numbness or tingling: Often in hands, feet, or face. Sometimes it feels like pins and needles. Other times, it’s complete loss of sensation.
- Balance and coordination issues: Walking feels unsteady. You might trip more. Falls become common.
- Bladder and bowel problems: Urgency, leakage, constipation. These are rarely talked about but deeply affect daily life.
- Vision problems: Optic neuritis-painful vision loss in one eye-is a classic first sign.
And then there’s the invisible stuff-the anxiety, depression, and isolation. 82% of employed people with MS need workplace changes. Flexible hours. Remote work. Shorter days. These aren’t luxuries. They’re survival tools.
How Is MS Diagnosed?
There’s no single blood test. Diagnosis takes time-often 6 to 12 months. Doctors use the McDonald Criteria, updated in 2017. It requires proof of damage in two different areas of the central nervous system (dissemination in space) and evidence that damage happened at different times (dissemination in time).
That means:
- At least one lesion on MRI in the brain, spinal cord, or optic nerve.
- At least one lesion that’s active (gadolinium-enhancing) and one that’s old (non-enhancing), OR a new lesion on a follow-up scan.
- Ruling out other conditions like Lyme disease, lupus, or vitamin B12 deficiency.
MRIs are the star tool. A 3 Tesla machine catches 30% more lesions than older 1.5 Tesla scanners. That means earlier, more accurate diagnosis. But even with perfect scans, it’s still a puzzle. Doctors combine MRI with spinal fluid tests, nerve conduction studies, and clinical history.
Treatment: Slowing the Damage, Not Curing It
There’s no cure yet. But there are more tools than ever to slow progression and manage symptoms.
Disease-modifying therapies (DMTs) are the backbone. They don’t fix existing damage-they stop new attacks. There are six types:
- Injections: Interferon beta, glatiramer acetate. Used for decades. Side effects: flu-like symptoms, injection site reactions (76% of users report pain or redness).
- Oral pills: Fingolimod, teriflunomide, dimethyl fumarate. Easier to take. Risk of liver damage or lowered white blood cell count.
- Infusions: Ocrelizumab, ofatumumab, ublituximab. Given every few months. More effective. Higher cost-up to $87,000 a year.
But here’s the catch: 42% of people stop injectable therapies within a year because of side effects. That’s why newer drugs are changing the game. Ublituximab (Briumvi), approved in 2023, cut relapses by 50% compared to older pills. Ocrelizumab helped 68% of users stay relapse-free over two years.
Cost is a barrier. Most U.S. patients get copay help from drugmakers-90% do. But in low- and middle-income countries, half of people can’t access any DMTs at all.
Rehabilitation and Daily Living
Treatment isn’t just pills. Physical therapy, occupational therapy, and speech therapy are critical.
Balance training reduces falls by 47%. That’s huge. A simple program of standing on one foot, walking heel-to-toe, and using resistance bands can make the difference between staying independent and needing a cane-or worse.
Heat sensitivity is real. Hot showers, summer days, fever-they can make symptoms worse temporarily. Cooling vests, cold drinks, air conditioning aren’t luxuries. They’re medical tools.
And diet? No magic food cures MS. But people who eat more vegetables, omega-3s, and fiber report better energy and fewer flare-ups. The gut-brain connection is being studied. Early trials with fecal transplants show 30% drops in inflammation markers. It’s early, but promising.
What’s Next? Hope on the Horizon
Research is moving fast. Scientists are no longer just trying to stop attacks-they’re trying to repair damage.
- Remyelination therapies: Drugs like opicinumab aim to rebuild myelin. In trials, they improved nerve signal speed by 15%.
- Stem cell transplants: 127 active trials as of early 2024. Some patients with aggressive MS have gone years without relapses after resetting their immune system.
- Biomarkers: Measuring neurofilament light chain in blood now predicts flare-ups before symptoms appear.
- Estrogen-targeting drugs: ANV419, tested in 2024, reduced new lesions by 40% in early trials.
And prognosis? It’s improving. In Sweden, 70% of people diagnosed after 2010 are still walking without help 20 years later. Back in the 1980s, that number was 45%. Early diagnosis and aggressive treatment are making the difference.
Final Thoughts: MS Is Not a Death Sentence
It’s a lifelong condition. But it’s not a death sentence. People with MS live full lives-work, travel, raise families, run marathons. The key? Catch it early. Treat it aggressively. Manage symptoms daily. And don’t wait for a cure to live well today.
The science is advancing. The tools are better. The community is louder. And for the first time, people with MS aren’t just surviving-they’re thriving.
Is multiple sclerosis hereditary?
MS isn’t directly inherited like eye color, but genetics play a big role. If a parent has MS, your risk goes up to about 2-5%, compared to 0.1% in the general population. The HLA-DRB1*15:01 gene variant is the strongest known genetic link, tripling your risk. But even with this gene, most people never develop MS. Environmental triggers like Epstein-Barr virus and low vitamin D are just as important.
Can you get MS if you live near the equator?
Yes, but it’s rare. MS prevalence is lowest near the equator-about 30 cases per 100,000 people. In northern countries like Canada or Sweden, it’s 10 times higher. Sunlight exposure and vitamin D levels are major factors. People born and raised in low-sunlight areas have higher risk, even if they later move to sunny regions. Migration studies show moving before age 15 changes your risk to match your new location.
Do MS symptoms get worse with age?
Not always, but often. In relapsing-remitting MS, symptoms may stabilize during remissions. But over time, many people shift to secondary progressive MS, where damage accumulates and symptoms gradually worsen. Aging also brings its own changes-muscle loss, slower recovery, joint stiffness-that can make MS-related weakness feel worse. That’s why staying active, managing stress, and treating other health issues (like high blood pressure or diabetes) are crucial as you get older.
Can stress cause MS flare-ups?
Stress doesn’t cause MS, but it can trigger flare-ups. Studies show people who report high stress levels in the weeks before a flare are more likely to have one. It’s not the stress itself-it’s how it affects your immune system. Chronic stress raises cortisol and inflammatory markers, which can worsen nerve damage. Managing stress through sleep, mindfulness, therapy, or even just walking daily can reduce flare frequency.
Is there a cure for MS on the horizon?
There’s no cure yet, but the field is shifting from symptom control to repair. Researchers are now focused on remyelination-growing new myelin-and neuroprotection-shielding nerves from damage. Drugs like opicinumab and stem cell therapies are showing real promise in trials. Some patients have gone years without relapses after immune reset treatments. While a full cure may still be years away, the goal is no longer just slowing MS-it’s reversing it.
Are MS treatments safe for long-term use?
Most disease-modifying therapies are safe for long-term use, but they require monitoring. Infusion drugs like ocrelizumab lower certain immune cells, so doctors check blood counts regularly. Oral drugs may affect liver function or increase infection risk. The key is balancing benefit and risk. For most people, the benefit-fewer relapses, less disability-far outweighs the risks. Stopping treatment without medical advice is more dangerous than continuing it.

Comments (9)
Chris porto
December 19, 2025 AT 05:12
It's wild to think our own bodies can turn against us like this. I used to think autoimmune stuff was just 'bad luck,' but now I see it's this perfect storm of genes, environment, and maybe even viruses we didn't know were ticking time bombs. The EBV link is chilling. Not everyone gets MS after mono, but almost everyone with MS had it. Makes you wonder what else we're carrying around that we don't know about.
And the vitamin D thing? Makes sense. We're indoors too much, scared of the sun, and then wonder why our immune systems are confused. We treat symptoms like they're the problem, not the symptom of something deeper.
Danielle Stewart
December 20, 2025 AT 00:06
Thank you for writing this with such clarity. I’ve been living with RRMS for 12 years, and this is the first time I’ve seen someone explain the difference between relapses and progression without using medical jargon that makes me feel like I’m back in a doctor’s office.
For anyone new to this: yes, it’s scary. But you’re not alone. The community here is quiet, but it’s strong. And the treatments now? They’re lightyears ahead of what we had in 2010. Keep going. You’re doing better than you think.
jessica .
December 21, 2025 AT 23:55
They say it’s autoimmune but what if it’s just the vaccines? I read a guy on TruthFeed who said 87% of MS cases popped up after the jab. And why do they only test on rich countries? They’re hiding the real cause. Vitamin D? Pfft. It’s the fluoridated water and 5G towers. Look at the maps - MS hotspots line up with cell towers. Coincidence? I think not.
Also, why do they want you on drugs that cost 87k a year? They’re making bank off your fear. Don’t fall for it. Go outside. Get sun. Stop taking pills.
Ryan van Leent
December 22, 2025 AT 15:19
Why do people with MS get to have flexible work hours but I gotta show up at 9am and grind? I work 60 hours a week and I don't even have a single lesion. This whole thing feels like a scam. You're not tired you're just lazy. And why is everyone so obsessed with vitamin D? You think the government is giving you a free pass because you're sick? Newsflash: life isn't fair. Get over it.
Also that guy who said 'concrete block' - sounds like he just doesn't want to get out of bed.
Sajith Shams
December 23, 2025 AT 22:51
You people are missing the point. In India, we don’t have access to these $87,000 drugs. We don’t have 3 Tesla MRIs. We have one neurologist for every 500,000 people. You talk about remyelination like it’s a Netflix documentary. Meanwhile, my cousin in Delhi can’t even get interferon because the government says it’s ‘too expensive.’
Stop talking about your relapses like they’re a TED Talk. The real MS crisis is in the Global South. You’re not helping. You’re just performing empathy.
Glen Arreglo
December 25, 2025 AT 14:47
Sajith’s point hits hard. I grew up in rural Australia - no neurologist within 300km. My sister got diagnosed at 28 after 18 months of being told it was ‘stress.’ We didn’t have MRI access until she moved to Sydney.
It’s not just about drugs or science. It’s about equity. If your zip code determines your lifespan in MS, then we’ve failed. We need global access to diagnostics, not just fancy new drugs for the wealthy. This isn’t just medicine - it’s justice.
shivam seo
December 26, 2025 AT 00:13
So let me get this straight - we spend billions on drugs that don’t cure anything, people get fat on disability checks, and we still don’t know why it happens? This whole system is a money pit. Why not just fund research into why the immune system goes haywire instead of treating symptoms like we’re fixing a leaky faucet?
Also, ‘cooling vests’? That’s not medicine, that’s a luxury spa accessory. Get real.
benchidelle rivera
December 26, 2025 AT 02:22
Shivam, your tone is dismissive, but your frustration is valid. We do need to redirect funding toward root-cause research - not just symptom management. But dismissing people’s daily struggles as ‘luxury’ ignores how real and debilitating those symptoms are.
Heat sensitivity isn’t a ‘spa accessory’ - it’s a neurological event. A warm shower can paralyze someone for hours. That’s not laziness. That’s biology. We need both: better science AND better compassion. Not one or the other.
Isabel Rábago
December 26, 2025 AT 11:06
My brother had MS. He died at 42. They told him he’d have 20 years. He got 8. No relapses. No flares. Just… slow fade. No cure. No miracle. Just a quiet goodbye.
Don’t talk about thriving. Not everyone gets to.