Most people have moles. Some are harmless, others aren’t. The difference can be life-or-death. That’s why the ABCDE rule exists - not to diagnose melanoma, but to catch it early when treatment works best. It’s simple: look for Asymmetry, Border irregularity, Color variation, Diameter, and Evolution. But here’s the catch - many melanomas don’t follow these rules. And that’s where things get dangerous.
What the ABCDE Rule Actually Measures
The ABCDE rule was created in the 1980s by dermatologists to help both doctors and patients spot warning signs. It’s not a diagnosis. It’s a flag. Here’s what each letter means in real terms:
- A - Asymmetry: If you draw a line through the middle of the mole, both halves don’t match. A normal mole is usually round or oval and symmetrical.
- B - Border irregularity: The edges are ragged, blurred, or notched. Benign moles have smooth, even borders.
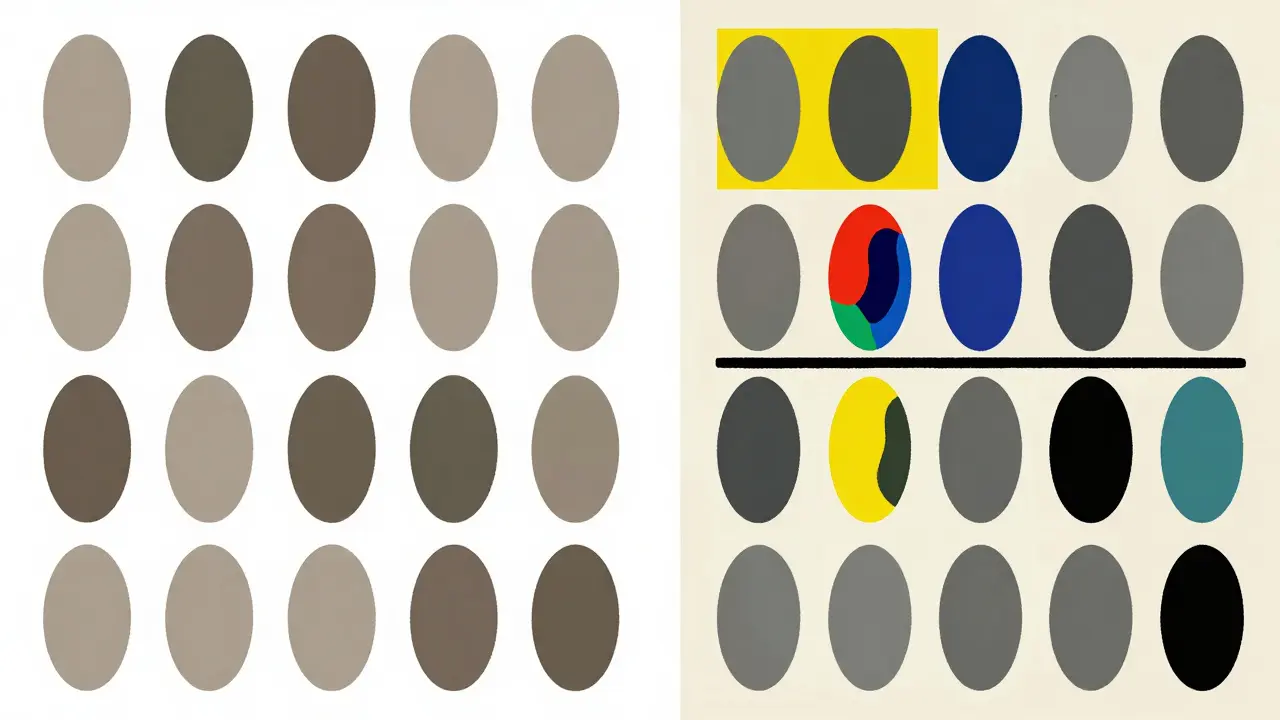
- C - Color variation: A mole with multiple shades - black, brown, red, white, or blue - is suspicious. Uniform color is normal.
- D - Diameter: Traditionally, anything larger than 6mm (about the size of a pencil eraser) raises concern. But newer guidelines from Phoenix Surgical Dermatology Group say 5mm is enough to worry about. And here’s the twist: 30% of melanomas are smaller than 6mm when found.
- E - Evolving: This is the most important one. Has the mole changed in size, shape, color, or texture? Has it started itching, bleeding, or crusting? Any change over weeks or months matters more than size or color alone.
Some experts now add an F for "Funny looking" and a G for "Growing rapidly." But even these expanded versions miss cases. A 2022 study in PubMed found that 36% of melanomas were in situ - the earliest stage - and nearly one-third of those showed no "E" sign at all.
Why the ABCDE Rule Isn’t Enough
The rule was never meant to be perfect. It was designed to raise awareness. But many people treat it like a pass/fail test. If a mole doesn’t meet three or four criteria, they wait. That’s a mistake.
Dr. Allan Halpern from Memorial Sloan Kettering says 20-30% of melanomas don’t fit the ABCDE pattern. Desmoplastic melanoma - a rare but aggressive type - shows classic signs in only 15% of cases. Childhood melanoma? Only 18% fit the rule. Even more troubling: a 2022 survey by the American Academy of Dermatology found that 42% of people delayed seeing a doctor because their mole didn’t meet enough ABCDE criteria. The average delay? Over seven months.
One Reddit user, u/SkinCancerSurvivor, shared their story: "My melanoma was perfectly symmetrical, uniform color, and only 3mm. None of the ABCDE criteria applied. It was stage IIB." That’s not rare. Dermatologists report that more than half of melanomas they find in their clinics had fewer than two ABCDE features.
The Ugly Duckling Sign: What Dermatologists Really Look For
Experts don’t just count ABCDE signs. They compare. The "ugly duckling" sign is often more reliable than the ABCDE rule. It means: "This mole looks different from all the others on your body."
A 2019 study in the British Journal of Dermatology showed this sign caught 73% of melanomas that ABCDE missed. Why? Because your body has patterns. Most moles look alike. One that stands out - darker, bigger, flatter, raised - is the one to check.
Think of it like a choir. If everyone’s singing the same note and one voice suddenly changes pitch, you notice it. That’s the ugly duckling. You don’t need to know the ABCDE rule to see it. You just need to know your own skin.
When Do You Get a Biopsy?
A biopsy isn’t automatic. Dermatologists don’t cut out every weird mole. They use a mix of tools:
- Three or more ABCDE signs - sensitivity 85%, specificity 72%. This is the baseline trigger.
- Documented change over 3-6 months - sensitivity jumps to 92%. This is the strongest predictor.
- Ugly duckling appearance - sensitivity 73%. Even if the mole looks "normal," if it’s the odd one out, biopsy.
But here’s the problem: most people don’t have photos of their moles from six months ago. The Skin Cancer Foundation says only 19% of patients bring baseline images to their appointment. Without them, it’s hard to prove evolution - the most important sign.
That’s why dermatologists use dermoscopy - a handheld magnifier with polarized light. It reveals patterns invisible to the naked eye. In 85% of U.S. dermatology practices, it’s standard. It raises diagnostic accuracy from 75% to 92%. But if you’re doing self-checks at home, you won’t have access to it.
The Cost of False Alarms
Every biopsy carries risk - scarring, infection, cost. And the ABCDE rule isn’t precise. A 2022 study in JAMA Internal Medicine found that for every one melanoma caught using ABCDE criteria, 4.7 benign moles are removed. That’s $417 million spent annually in the U.S. on unnecessary procedures.
That’s why dermatologists are moving beyond the rule. Digital tools are now being used to analyze moles with AI. The FDA approved SkinVision in 2022 - an app that uses ABCDE plus machine learning trained on 12 million images. It’s 95% sensitive. It’s not perfect, but it helps prioritize who needs to see a doctor.
Some centers now use molecular tests like DecisionDx-Melanoma, which analyzes gene expression in a small sample. It can tell if a suspicious mole is likely to be cancerous without cutting it out. Used in 68% of academic dermatology centers, it reduces unnecessary biopsies by 31%.
What You Should Do Right Now
You don’t need to be a dermatologist. You just need to be observant.
- Check your skin monthly. Use a mirror. Look at your back, scalp, between toes, under nails.
- Use the ABCDE rule as a starting point - not a final answer.
- Look for the ugly duckling. If one mole looks different from the rest, get it checked.
- Take photos of suspicious moles every 3 months. Compare them. Changes matter more than size.
- If it’s changing, bleeding, itching, or just "feels wrong," don’t wait for it to meet ABCDE criteria. Go.
Early-stage melanoma (in situ) has a 99% five-year survival rate. Stage IV? Just 32.6%. That gap isn’t about better treatments. It’s about catching it before it spreads.
The Future of Melanoma Detection
The ABCDE rule isn’t going away. But it’s evolving. The USPSTF’s 2023 draft update now emphasizes "change over time" as the #1 red flag. The International Dermoscopy Society launched ABCDE 2.0 in January 2023 - combining visual checks with AI analysis. By 2027, experts predict the rule will be just the first step in a multi-tool system: photos, dermoscopy, AI, and sometimes gene testing.
For now, though, your eyes are still the most powerful tool you have. Don’t wait for a mole to tick every box. If something feels off, it probably is. And that’s enough reason to see a doctor.
Can a mole be cancerous even if it’s small?
Yes. While melanomas are often larger than 6mm, 30% are found when smaller than that. Size alone isn’t a reliable indicator. A small mole that’s changing color, bleeding, or looks different from your other moles can still be melanoma.
Is the ABCDE rule reliable for everyone?
No. The ABCDE rule works best for common melanomas, but it misses many types - especially desmoplastic melanoma, childhood melanoma, and early in situ lesions. About 20-30% of melanomas don’t show classic ABCDE features. That’s why the "ugly duckling" sign and tracking changes over time are just as important.
Should I biopsy every mole that looks weird?
No. Dermatologists use a combination of factors: ABCDE signs, the ugly duckling sign, documented change, and dermoscopy. Most moles are benign. Biopsy is recommended only when multiple warning signs are present or there’s clear evolution over time. Unnecessary biopsies are common and costly.
How often should I check my moles?
Once a month. Use a full-length mirror and a hand mirror to check hard-to-see areas like your back, scalp, and between toes. Take photos of any suspicious moles every 3 months to track changes. If you have a history of skin cancer or many moles, see a dermatologist annually.
Can apps or AI replace a dermatologist?
No. Apps like SkinVision can help flag suspicious moles using AI and ABCDE criteria, but they’re screening tools - not diagnostic ones. They can miss cancers or give false reassurance. Only a dermatologist can perform a biopsy and give a definitive diagnosis. Use apps to decide when to go, not to avoid going.
Comments (12)
phara don
February 2, 2026 AT 18:40
Been checking my moles since I got sunburned at the lake last summer. One on my shoulder looks kinda weird now - not big, but it’s been slowly getting darker. Took a pic every month like the post said. Honestly? I didn’t know about the ugly duckling thing until now. That makes way more sense than counting letters.
clarissa sulio
February 3, 2026 AT 01:03
Why are we even talking about this like it’s a mystery? If your skin looks wrong, get it checked. No app, no rule, no fancy acronym replaces a doctor. America’s too lazy to care until it’s too late. I’ve seen it too many times.
Bridget Molokomme
February 3, 2026 AT 06:15
So let me get this straight - we’re supposed to trust a rule invented in the 80s that misses 30% of melanomas… but somehow AI apps are the future? 😂
Also, ‘ugly duckling’? That’s the best dermatologists got? Sounds like a Pinterest post title. At least the ‘change over time’ part makes sense. The rest feels like we’re just repackaging common sense with fancy labels.
Vatsal Srivastava
February 3, 2026 AT 17:07
ABCDE rule is for people who don't read journals
Real dermatologists use dermoscopy and histopathology
You think a layperson can diagnose cancer by looking at a mole?
Pathetic
Brittany Marioni
February 5, 2026 AT 14:08
Thank you so much for this post - seriously, thank you. I’ve been terrified of my moles for years, and I didn’t know whether to panic or ignore them. Now I get it: it’s not about ticking boxes. It’s about noticing what’s different. I started taking monthly photos of my back and legs - I had no idea how many moles I even had! One looked totally different from the others - I went in last week. It was benign, but I’m so glad I checked. You’re right - your body knows. Listen to it.
Monica Slypig
February 6, 2026 AT 23:32
Ugly duckling my ass. I dont even know what my moles look like cause I dont care. Why do people make this into some big thing? Just get a full body scan if you're that worried. All this ABCDE stuff is just to sell derm appointments. I saw a doc last year for a spot that was fine. They charged me 400 bucks to say 'it's fine'. So thanks, but no thanks.
Becky M.
February 8, 2026 AT 06:56
I’m from a rural town where no one talks about skin cancer. I didn’t even know what a biopsy was until I had one. My mom had melanoma. She waited because her mole didn’t look "bad enough." I’m 28 now and I check my skin every month. I take photos. I show my friends. I tell my cousins. We don’t have to be experts. We just have to care enough to look. And if you’re reading this? Look at your skin right now. Just once. Please.
jay patel
February 9, 2026 AT 10:20
Look, I get it - the ABCDE rule is a tool, not a gospel. But here’s the thing - most people don’t even know what asymmetry means, let alone track evolution over time. I’ve seen friends ignore spots because they’re "under 6mm" - and then they get diagnosed at stage 3. The ugly duckling sign? That’s gold. It’s intuitive. You don’t need a medical degree to notice one mole that looks like it crashed a party where everyone else is wearing jeans and a t-shirt - and it shows up in a tuxedo. Also, apps? They’re okay for nudging you, but they’re not magic. I use SkinVision to remind me to go see my derm - not to replace him. And yes, I’ve taken photos every 3 months since 2021. It’s weird, but it works. And if you’re not doing it? Start tomorrow. Your future self will thank you.
Ansley Mayson
February 11, 2026 AT 00:33
More biopsies = more money. More apps = more data. More rules = more fear. The real problem? We’ve turned skin checks into a performance. Who cares if your mole is symmetrical? If it itches, bleeds, or makes you go "huh," go see someone. Stop overcomplicating it. The system wants you confused so you keep paying.
Hannah Gliane
February 11, 2026 AT 17:30
OMG I just checked my back and one mole is literally glowing?? 🤯 I mean not literally but it looks like it’s lit from inside?? I’m going to the derm tomorrow!! I didn’t even know I had that one!! Thank you for this post!! 😭🙏 #SkinCancerAwareness #UglyDucklingIsReal
Murarikar Satishwar
February 12, 2026 AT 08:59
The ABCDE rule is a good starting point, but it's not a substitute for clinical judgment. The ugly duckling sign is more powerful because it's based on individual variation - not population averages. A mole that looks normal to a textbook might be abnormal for your skin. That's why dermatologists emphasize pattern recognition over checklist scoring. Also, the fact that 30% of melanomas are under 6mm is critical - size is not a safety net. And yes, AI tools like SkinVision are promising, but they're only as good as the data they're trained on. Still, if you're using one to prompt a visit, that's better than ignoring it. The goal isn't to diagnose yourself - it's to know when to get help.
Bob Hynes
February 13, 2026 AT 10:21
So I’m Canadian and we don’t have derm appointments on demand like y’all do. Took me 6 months to get in. I took pics. I tracked changes. I showed my GP. He said "eh, looks fine." But I kept going back. Third time? He referred me. Turns out it was stage 1. If I’d listened to the ABCDE rule and waited for it to tick 3 boxes? I’d be in chemo right now. Don’t wait for permission to worry. Your body’s screaming - listen.