When an older adult suddenly becomes confused, withdrawn, or agitated out of nowhere, it’s easy to assume it’s just aging-or dementia getting worse. But often, the real culprit is something simpler, and more dangerous: a medication. Medication-induced delirium is the most common reversible cause of sudden confusion in people over 65, and it’s happening far more often than most families and even doctors realize. Unlike dementia, which creeps in slowly, delirium hits fast-sometimes within hours of taking a new pill. And if it’s not caught, it can lead to longer hospital stays, permanent brain changes, or even death.
What Exactly Is Medication-Induced Delirium?
Delirium isn’t just being forgetful. It’s a sudden, serious change in mental function that comes on over hours or days. People with delirium struggle to focus, get easily distracted, and may not recognize family members or know where they are. Their thinking jumps around. They might talk nonsense, hallucinate, or become unusually quiet. The key sign? It fluctuates. One hour they’re alert and chatting; the next, they’re staring blankly at the wall. This isn’t normal aging. It’s a medical emergency.
Medications cause about 70% of all delirium cases in older adults, according to the American Geriatrics Society. The drugs most often to blame are those that block a brain chemical called acetylcholine-this is called anticholinergic activity. Think of acetylcholine as the brain’s GPS for attention and memory. When these drugs shut it down, confusion follows.
Top Culprits: The Medications That Trigger Delirium
Not all drugs are equal when it comes to risk. Some are far more dangerous than others, especially for older brains.
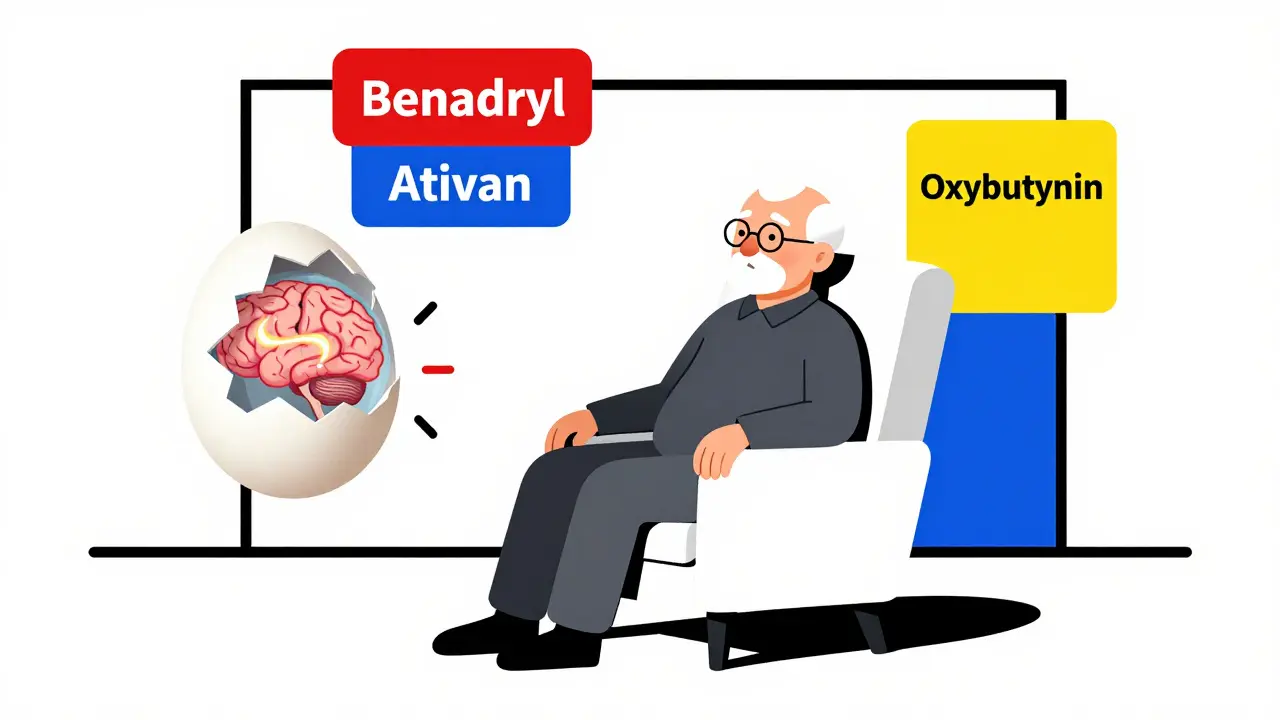
- First-generation antihistamines like diphenhydramine (Benadryl) are everywhere-cold medicines, sleep aids, allergy pills. They’re strong anticholinergics. Studies show every increase in anticholinergic burden raises delirium risk by nearly 80%. Yet, they’re still routinely prescribed to seniors for sleep or allergies.
- Benzodiazepines like lorazepam (Ativan) and diazepam (Valium) are used for anxiety, insomnia, or seizures. But they double or even triple delirium risk. In ICU patients, they can extend delirium by over two days. Even short-term use in hospitals increases the chance of confusion.
- Opioids, especially morphine and meperidine, are a major trigger. Meperidine’s metabolite, normeperidine, can overstimulate the brain, causing seizures and confusion. Hydromorphone is a safer alternative-it’s linked to 27% less delirium at the same pain-relieving dose.
- Bladder medications like oxybutynin and tolterodine, meant for overactive bladder, are packed with anticholinergic effects. They’re commonly prescribed to older women, but the brain pays the price.
- Antidepressants like amitriptyline and trazodone are also high-risk. Even though they help with mood or sleep, their anticholinergic properties make them dangerous for seniors.
The American Geriatrics Society’s Beers Criteria® lists 56 medications to avoid in older adults, including many of these. Yet, a 2023 study found 43% of hospitals still routinely give them to seniors.
The Silent Type: Hypoactive Delirium
Most people picture delirium as someone yelling, pacing, or hallucinating-that’s hyperactive delirium. But in older adults, the most common form is hypoactive delirium. These patients don’t act out. They sit quietly. They don’t respond when spoken to. They seem depressed, tired, or just “off.”
Doctors and nurses often mistake this for depression, fatigue, or dementia progression. In fact, 72% of medication-induced delirium cases in seniors are hypoactive, and 70% go undiagnosed. A 2020 study found that 89% of caregivers noticed a sudden, dramatic personality shift-like a once-chatty grandparent becoming silent and unresponsive-within 48 hours of starting a new medication. That’s not normal. That’s a red flag.
Who’s Most at Risk?
It’s not just about the drug-it’s about the person. Certain factors make delirium much more likely:
- Age over 85-risk jumps 2.3 times compared to those 65-74.
- Pre-existing dementia-delirium lasts nearly twice as long (8.2 days vs. 4.7 days).
- Taking three or more anticholinergic drugs-risk increases 4.7 times.
- Recent hospitalization or surgery-especially in intensive care.
- Dehydration, infection, or electrolyte imbalances-these often combine with medications to trigger delirium.
One 2021 analysis found that medication-induced delirium costs the U.S. healthcare system $164 billion each year. That’s not just money-it’s lost independence, longer recovery, and more nursing home placements.
How to Prevent It
The good news? Medication-induced delirium is one of the most preventable conditions in geriatric care. You don’t need fancy equipment or expensive tests. You just need awareness and action.
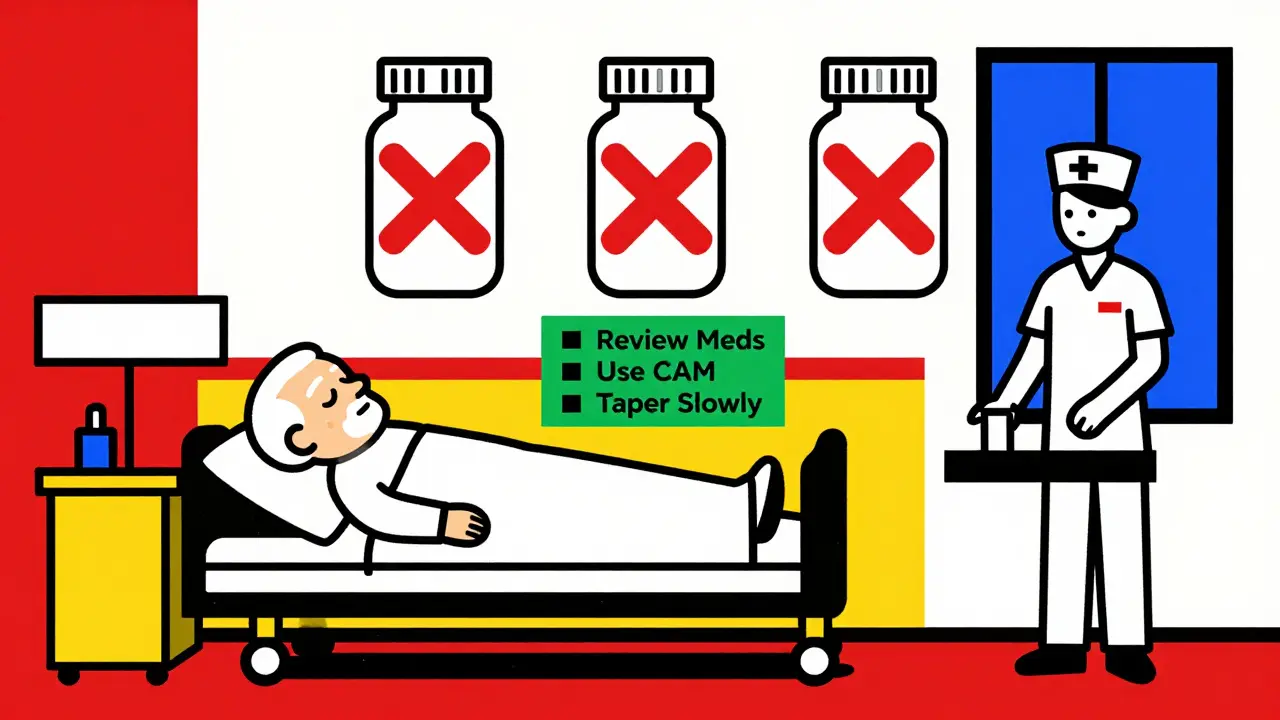
- Review every medication-including over-the-counter pills. Use the Anticholinergic Cognitive Burden (ACB) scale. A score of 3 or higher means high risk. Ask your pharmacist to run this check.
- Replace high-risk drugs. Swap diphenhydramine for loratadine (Claritin). Swap benzodiazepines for non-drug sleep strategies like light therapy or routine. For bladder issues, try pelvic floor exercises instead of oxybutynin.
- Use the STOPP/START criteria. This is a tool doctors use to find inappropriate prescriptions. One 2018 study showed it cut delirium rates by 26%.
- Manage pain without opioids. Use acetaminophen, ice packs, physical therapy, or massage. A 2019 study found multimodal pain care reduced opioid use by 37%, directly lowering delirium risk.
- Screen with CAM. The Confusion Assessment Method is a simple 2-minute tool hospitals use to spot delirium. Ask if your loved one’s hospital uses it. If not, request it.
- Taper slowly. Never stop benzodiazepines or anticholinergics suddenly. Withdrawal can trigger delirium tremens-a life-threatening condition. Always reduce doses over 7-14 days under medical supervision.
The Hospital Elder Life Program (HELP), developed at Yale, cuts delirium by 40% using simple steps: keeping seniors oriented, getting them out of bed, ensuring sleep, and avoiding unnecessary drugs. It’s free, evidence-based, and works.
What Families Can Do
You don’t need to be a doctor to protect your loved one. Here’s what you can do right now:
- Keep a list of every medication-name, dose, reason, and when it was started. Include vitamins and supplements.
- Ask the doctor: “Is this drug on the Beers Criteria list? Is there a safer alternative?”
- Watch for sudden changes: confusion, quietness, agitation, trouble sleeping, or new incontinence.
- If delirium is suspected, say: “Could this be from a medication? We’d like to review all prescriptions.”
- Don’t accept “It’s just old age” as an answer. Delirium is treatable-if caught early.
The Future Is Changing
Things are improving. In 2023, the FDA required stronger warning labels on anticholinergic drugs. The National Institute on Aging is funding real-time monitoring tools that flag high-risk drug combinations in electronic health records. AI systems now predict delirium risk with 84% accuracy by analyzing medication lists-currently being tested in 47 hospitals.
But progress is slow. Only 18% of hospitals systematically screen for anticholinergic burden. And since the U.S. population over 65 will grow from 56 million to 80 million by 2040, this problem is only getting bigger.
Medication-induced delirium isn’t inevitable. It’s preventable. It’s not a normal part of aging. It’s a signal that something in the medication plan needs to change. The next time a senior becomes suddenly confused, don’t assume it’s dementia. Ask: What did they start taking recently? That one question could save their brain-and their life.
Can medication-induced delirium be reversed?
Yes, if caught early. Once the triggering medication is stopped or replaced, most people improve within days to a few weeks. Recovery is faster in those without dementia. But if delirium lasts too long or isn’t treated, it can lead to permanent cognitive decline or increase the risk of developing dementia later.
Is Benadryl safe for older adults?
No, it’s not recommended. Diphenhydramine (Benadryl) is a strong anticholinergic and one of the top causes of medication-induced delirium in seniors. Even occasional use can cause confusion, dizziness, or urinary retention. Safer alternatives include loratadine (Claritin), cetirizine (Zyrtec), or fexofenadine (Allegra)-these have little to no anticholinergic effect.
Why do doctors still prescribe high-risk medications?
Many doctors aren’t trained in geriatric pharmacology. Some prescribe these drugs because they’re familiar, cheap, or easy to write. Others don’t realize how dangerous they are for older brains. Also, patients or families may ask for sleep aids or anxiety meds without knowing the risks. Education and better screening tools are slowly changing this, but the gap remains wide.
Can delirium lead to dementia?
Delirium doesn’t cause dementia, but it can accelerate it. People who have one episode of delirium are twice as likely to develop dementia within the next year. Those with existing dementia often suffer worse cognitive decline after delirium. Preventing delirium is one of the best ways to protect brain health in older adults.
What should I do if my loved one develops delirium in the hospital?
First, ask the medical team to review all medications-especially those started in the last 72 hours. Request a geriatric consultation. Ask if they’re using the Confusion Assessment Method (CAM) to screen for delirium. Push for non-drug care: keep the room quiet and well-lit, bring familiar items, encourage walking, and ensure hydration. Avoid sedatives unless absolutely necessary. Stay involved-your presence can calm them and help staff spot changes.
Comments (1)
Greg Scott
February 20, 2026 AT 17:43
My grandma went through this last year. Started on Benadryl for allergies, next thing you know she’s staring at the wall for hours. We thought it was dementia getting worse-turns out it was just one damn pill. Took her a month to bounce back after they pulled it. Why are these still OTC? They should be prescription-only for seniors.