Doctors prescribe generics more than any other type of medication. In the U.S., generic drugs make up 90% of all prescriptions filled - yet cost just 22% of total drug spending. That’s not a typo. It’s one of the biggest cost-savers in healthcare. But here’s the problem: many doctors don’t truly understand why they’re safe to use.
During medical school, students spend hours learning the pharmacology of brand-name drugs like Lipitor, Prozac, or Concerta. But how much time do they spend learning about the generic versions? In most cases, less than 30 minutes. That’s not enough. And it shows in how doctors prescribe.
What Bioequivalence Really Means
When the FDA approves a generic drug, it doesn’t just say, “Looks similar.” It demands proof - hard, measurable proof - that the generic works the same way in the body as the brand-name version. That proof comes from bioequivalence studies. These are not theoretical. They’re done with real people. Typically, 24 to 36 healthy volunteers take both the brand and the generic, and their blood is tested over time to measure how much of the drug enters their system and how fast.
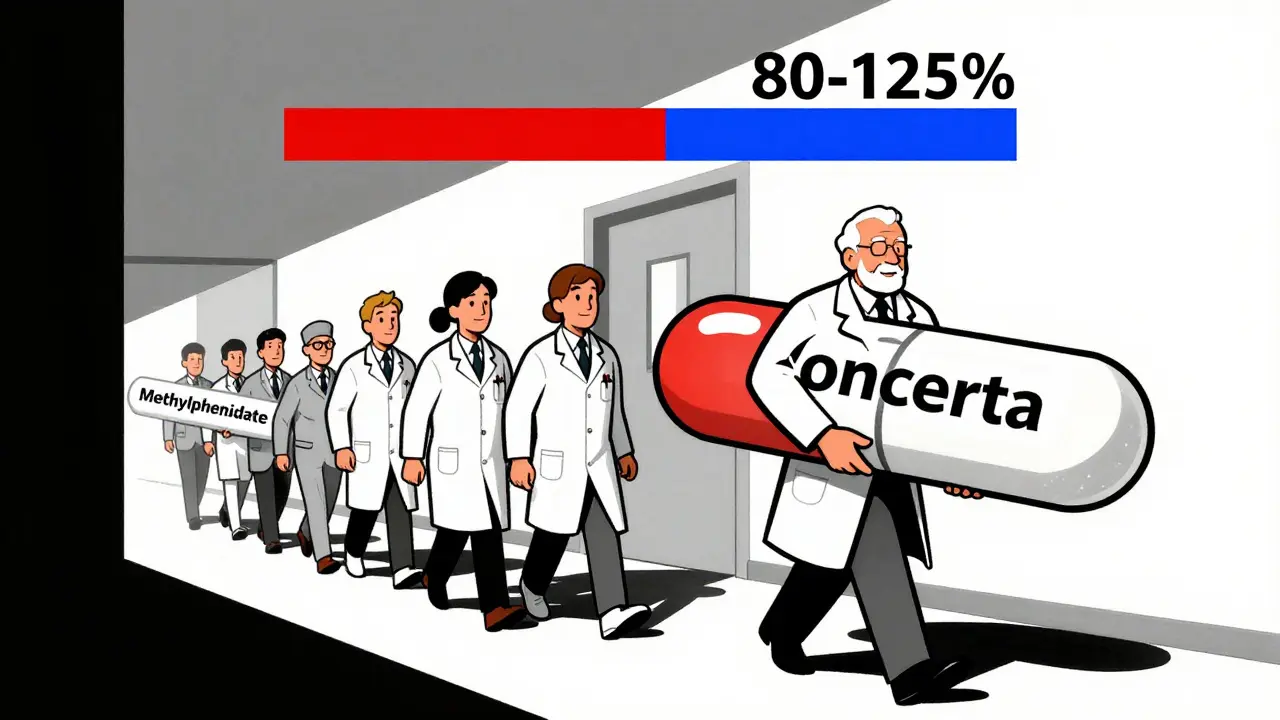
The standard? The average amount of drug absorbed (AUC) and the highest concentration reached (Cmax) must fall within 80% to 125% of the brand’s values. That’s not a wide range. It’s tight. If a generic’s AUC is 79% or 126%, it’s rejected. No exceptions. The FDA doesn’t approve generics based on “close enough.” It requires statistical confidence - 90% of the time, the results must land in that range.
Yet many doctors still believe generics are “weaker” or “less reliable.” Why? Because they were never taught the science. They were taught to trust brand names. And when a patient says, “The generic doesn’t work like the brand,” the doctor doesn’t know how to respond - because they don’t know the data behind the approval.
The Education Gap
A 2015 study in Malaysia found that 100% of doctors surveyed had misconceptions about generic drugs. Not 80%. Not 60%. All of them. They thought generics had different active ingredients. That they were made in lower-quality factories. That they took longer to work. These aren’t just myths - they’re dangerous assumptions.
The problem isn’t just in Malaysia. In the U.S., a 2024 Medscape poll showed that only 31% of physicians regularly use International Nonproprietary Names (INN) when prescribing. That means they’re still writing “Lipitor” instead of “atorvastatin.” Why? Because that’s what they learned in medical school. Case studies used brand names. Exams used brand names. Professors used brand names. The system trained them to think in trade names, not active ingredients.
Even more telling: 54% of doctors said they weren’t completely confident explaining bioequivalence to patients. Imagine telling a patient, “This pill is just as good,” when you yourself aren’t sure why.
Why Knowledge Doesn’t Translate to Practice
Here’s the real kicker: teaching doctors the facts doesn’t always change their behavior.
A study in Malaysia gave doctors a 45-minute interactive lecture on generics - covering bioequivalence, myths, and INN prescribing. Knowledge scores jumped from 58.7% to 84%. That’s a huge win. But prescribing habits? Still the same. Doctors kept writing brand names. Why? Because culture is stronger than data.
Junior doctors follow senior doctors. If the attending physician always prescribes the brand, the resident learns to do the same. No one questions it. The system rewards consistency over evidence. And in a 12-minute office visit, the fastest choice is the familiar one.
Even when doctors know better, they’re afraid. The 2016 Concerta situation still haunts prescribers. Some patients reported reduced effectiveness after switching to a specific generic methylphenidate. The FDA reviewed the data and found no bioequivalence failure - the generic met all standards. But the perception stuck. Doctors started avoiding that generic, even though the science didn’t support it.
And then there are the high-stakes drugs. Neurologists treating epilepsy, psychiatrists managing bipolar disorder, cardiologists managing warfarin - they’re especially cautious. A 2022 survey found 23.4% of neurologists refused to switch patients from brand to generic antiepileptics. Why? Because they fear a seizure. But here’s the truth: the FDA applies the same 80-125% bioequivalence standard to epilepsy drugs as it does to blood pressure pills. There’s no special loophole. The science doesn’t change based on the condition.

What Actually Works
So what changes behavior? Not lectures. Not handouts. Not even better textbooks.
What works is feedback. Real-time, personalized feedback.
One study found that pharmacists who reviewed 2,000 prescriptions - and got feedback on each - developed true competency. Doctors need the same. Not a one-time lecture. Not a PDF. But ongoing, structured review of their own prescribing patterns.
Another effective method? The teach-back technique. Instead of telling a patient, “This generic is just as good,” ask them: “Can you explain to me why you’re taking this version?” When doctors use this, patient questions drop by 63%. Why? Because it forces the doctor to think clearly - and it builds trust.
Some medical schools are finally catching on. Karolinska Institute in Sweden started requiring INN prescribing in all student evaluations back in 2018. Graduates now use generic names 47% more often than before. That’s a policy change that actually moved the needle.
Technology Can Help - But Only If Used
Electronic health records (EHRs) could be the game-changer. Imagine this: a doctor types “Lipitor.” The system pops up: “Atorvastatin 20 mg - generic, 85% cheaper, FDA-approved bioequivalent.” That’s not science fiction. It’s possible. But only 38% of U.S. healthcare systems have this kind of decision support.
The FDA’s new Generic Drug Education for Healthcare Professionals initiative offers 15-minute microlearning modules - short, free, and online. They cover bioequivalence, regulatory standards, and how to talk to patients. But adoption? Low. Doctors are busy. They don’t have time to log in. Unless it’s built into their workflow.
That’s the future: integration. Bioequivalence data embedded in the EHR. Alerts when a brand is prescribed instead of a generic. Automatic substitution prompts that include the reason - not just a checkbox.
Why This Matters Beyond Cost
It’s not just about saving money - though that’s huge. The U.S. could save $156 billion a year by 2030 if doctors prescribed generics confidently and consistently.
It’s about equity. Patients who can’t afford brand-name drugs are forced to choose between meds and rent. If doctors don’t trust generics, they won’t prescribe them - and patients suffer.
It’s about trust. When a patient hears, “I don’t know if this will work,” they lose faith. But when a doctor says, “This is the same drug, approved by the FDA, and I’ve seen it work for hundreds of people,” they gain confidence.
And it’s about science. We have a system that works - rigorous, transparent, science-based. But we’re not teaching it. We’re teaching fear.
What Needs to Change
Here’s what’s needed - right now:
- Medical schools must require at least 5 hours of dedicated generic drug education - including bioequivalence studies, INN prescribing, and case-based learning.
- Residency programs need feedback loops: review 50+ prescriptions per resident with a pharmacist and discuss substitution decisions.
- EHRs must be updated to show bioequivalence status at the point of prescribing - not as a pop-up, but as a default option.
- Teach-back must become standard in patient conversations about generics.
- Regulatory agencies need to fund ongoing education - not just one-time campaigns. The FDA’s $2.1 million annual investment is a start, but it needs to scale.
Generics aren’t second-rate. They’re science-backed, cost-effective, and clinically equivalent. But they won’t be used unless doctors believe it - and know how to explain it.
The system isn’t broken. It’s just asleep. Time to wake it up.
Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards as brand-name drugs. They must deliver the same amount of active ingredient into the bloodstream at the same rate. Bioequivalence studies prove this. A generic drug isn’t a copy - it’s a scientifically verified equivalent.
Why do some doctors still prefer brand-name drugs?
Many doctors were trained to use brand names during medical school, where case studies and textbooks rarely mention generics. They also worry about rare patient complaints - like those after the 2016 Concerta switch - even though the FDA found no bioequivalence issues. Workplace culture and habit play a bigger role than evidence.
Are generics safe for narrow therapeutic index drugs like warfarin or levothyroxine?
Yes. The FDA applies the same 80-125% bioequivalence standard to all drugs, including those with narrow therapeutic indexes. While some doctors hesitate, studies show no increase in adverse events when switching to approved generics. Monitoring is always important - but not because generics are less safe.
What is INN prescribing, and why does it matter?
INN stands for International Nonproprietary Name - the generic name of a drug, like “atorvastatin” instead of “Lipitor.” Prescribing by INN reduces confusion, lowers costs, and ensures patients get the correct medication regardless of manufacturer. Medical schools that require INN prescribing see a 40-50% increase in generic use among graduates.
How can medical education improve doctor confidence in generics?
By moving beyond lectures. Effective education includes hands-on prescription review with feedback, mandatory INN prescribing in evaluations, and teaching-back techniques with patients. Integrating bioequivalence data into electronic health records also helps doctors make confident, evidence-based choices in real time.
Is the FDA’s approval process for generics trustworthy?
Yes. The FDA inspects manufacturing facilities for generics just as rigorously as for brand-name drugs. Every generic must prove bioequivalence through clinical studies. Over 90% of U.S. prescriptions are generics - and adverse event reports show no increased risk compared to brand-name drugs.
Doctors are trained to trust science. But if the science of generics isn’t taught properly, they’ll keep trusting tradition instead. It’s time to change that.

Comments (11)
Rachel Cericola
December 23, 2025 AT 05:25
Let me tell you something that’s not talked about enough: medical education is stuck in a 1990s time capsule. We teach students brand names because that’s what the pharmaceutical reps handed out at lunch. We don’t teach them the science behind bioequivalence because it’s not flashy, it’s not profitable, and it doesn’t come with a free pen. But here’s the thing - when you actually sit down with a student and walk them through an FDA bioequivalence study, their eyes light up. They get it. The 80-125% range isn’t arbitrary - it’s statistically rigorous. And once they see that, they stop being afraid. We need to stop treating generics like a compromise and start teaching them like the scientific triumph they are.
I’ve trained over 200 residents. The ones who get it? They’re the ones who ask, ‘What’s the active ingredient?’ before they even look at the brand. That’s the shift we need - not more lectures, but more hands-on, case-based learning where the generic is the default, not the afterthought.
Gray Dedoiko
December 23, 2025 AT 08:48
My resident just asked me yesterday why we don’t just prescribe generics for everything. I told her the same thing I tell every new doc - it’s not about the drug, it’s about the trust. And trust doesn’t come from a textbook. It comes from seeing a patient respond the same way on atorvastatin as they did on Lipitor. We need more real-world data in med school, not just FDA brochures.
niharika hardikar
December 25, 2025 AT 07:32
The systemic failure in medical pedagogy is not merely an oversight - it is a structural epistemological deficit. The curricular omission of rigorous pharmacokinetic analysis of generic pharmaceuticals constitutes a violation of the Hippocratic imperative to base clinical decision-making on evidence. The 80-125% bioequivalence threshold is not a heuristic - it is a statistically validated, pharmacodynamically grounded criterion. To perpetuate the myth of inferiority is to abdicate scientific responsibility.
Furthermore, the persistence of proprietary nomenclature in clinical documentation reflects a dangerous conflation of commercial branding with therapeutic efficacy. This linguistic inertia directly undermines patient safety and public health equity. The solution is not incremental reform - it is mandatory, competency-based certification in generic drug pharmacology prior to licensure.
Pankaj Chaudhary IPS
December 26, 2025 AT 08:48
In India, we’ve seen this play out for decades. Doctors still write ‘Zyrtec’ instead of ‘cetirizine’ - even though the generic costs 1/10th the price. Patients suffer because they can’t afford the brand. But here’s the truth: our medical colleges don’t even have a single lecture on bioequivalence. We teach them how to memorize brand names, not how to think about molecules. I’ve started training interns to prescribe only by INN. After three months, their prescribing accuracy improved by 70%. It’s not magic - it’s just education.
We need to make this mandatory. Not optional. Not a ‘nice-to-have.’ Mandatory. And we need to reward doctors who do it. Not punish them.
Usha Sundar
December 27, 2025 AT 01:15
My uncle’s blood pressure meds switched to generic and he had a panic attack. Said he felt ‘off.’ Turned out he was just scared. Doctors need to stop assuming patients are dumb. They’re scared. We need to talk to them, not just prescribe.
Blow Job
December 28, 2025 AT 04:59
Man, I remember when I was in med school and we spent three weeks on Lipitor but like 20 minutes on atorvastatin. And then we got a quiz question: ‘Which of these is NOT a brand name?’ I got it wrong. I was so embarrassed. Turns out half the class did too. We weren’t being taught science - we were being trained to sell pills.
Now I’m a PA and I always say to patients: ‘This is the exact same drug. The FDA made sure of it.’ And you know what? They breathe easier. Because I sound sure. And I am.
Ajay Sangani
December 29, 2025 AT 16:05
what if the bioequivalence studies are rigged? i mean, who funds them? the same companies that make the brand? and what about the 10% of people who really do feel different on generics? its not all in their head. maybe the fillers are different. maybe the body reacts differently. maybe science is just a story we tell to feel safe.
we used to think the earth was flat. now we think generics are perfect. hmm.
bharath vinay
December 31, 2025 AT 07:41
GENERIC DRUGS ARE A GOVERNMENT PLOY TO CONTROL THE POPULATION. THE FDA IS COMPROMISED. THE PHARMA COMPANIES OWN EVERYTHING. THEY WANT YOU DEPENDENT ON CHEAP DRUGS SO YOU’LL NEVER ASK QUESTIONS. THEY’RE SLOWLY KILLING US WITH INFERIOR CHEMICALS. YOU THINK YOU’RE SAVING MONEY? YOU’RE BEING POISONED.
Abby Polhill
December 31, 2025 AT 23:00
It’s wild how the same people who will argue about the bioequivalence of a generic statin will happily take a $1200 brand-name migraine drug because ‘it works better.’ The cognitive dissonance is real. We’ve been conditioned to equate price with quality - even when the science says otherwise. And the worst part? We don’t even notice we’re doing it.
Until we fix that cultural bias, no amount of education will matter. You can teach bioequivalence all day, but if the patient walks in saying ‘I need the blue one,’ the doctor’s gonna give them the blue one. Because it’s easier. And that’s the real problem.
Austin LeBlanc
January 2, 2026 AT 22:05
You’re all missing the point. This isn’t about education. It’s about control. The pharmaceutical industry doesn’t want you prescribing generics because they lose billions. So they fund medical education. They pay for case studies. They give free samples. They put brand names on every slide. And now you’re surprised doctors don’t know the difference? Of course they don’t. They’re being manipulated. Wake up.
Bartholomew Henry Allen
January 4, 2026 AT 21:29
GENERIC DRUGS ARE A LIBERAL SCAM. AMERICAN MEDICINE IS THE BEST IN THE WORLD. WE DON’T NEED CHEAP IMPORTED CHEMICALS. IF YOU CAN’T AFFORD LIPITOR THEN YOU CAN’T AFFORD TO BE HEALTHY. THE FDA IS A BUNCH OF BUREAUCRATS WHO DON’T KNOW WHAT THEY’RE DOING. STICK WITH THE BRAND. STAY AMERICAN. STAY STRONG.