Every year, more than 1.5 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these aren’t accidents-they’re preventable. The biggest reason? Patients don’t know the basic terms that could keep them safe. You don’t need to be a doctor to protect yourself. You just need to know a few key words and how to use them when you’re handed a new prescription or told to take a pill.
What You Need to Know Before You Take Any Pill
Medication safety isn’t just about following the label. It’s about asking the right questions and using the right language to make sure you’re getting exactly what you need, when you need it, in the way it’s meant to be taken. The foundation of this is the Eight Rights of Medication Administration. This isn’t just a checklist for nurses-it’s your personal safety toolkit.
- Right patient: They must confirm it’s you. Ask: "Can you check my name and date of birth?" Two identifiers are standard in hospitals and clinics. Never assume they already know who you are.
- Right medication: The pill or liquid you’re given should match the name on your prescription. Ask for both the brand name and the generic name. Why? Because drugs like "Hydromorphone" and "Hydrocodone" sound almost the same-and mixing them up can be deadly.
- Right dose: How much are you supposed to take? A teaspoon? A tablespoon? A pill? Liquid medications are especially tricky. One wrong decimal point can mean a 10x overdose. Always double-check the number and the unit (mg, mL, etc.).
- Right route: Is this meant to be swallowed, injected, inhaled, or put on your skin? Giving an IV medicine by mouth can cause serious harm. If you’re unsure, ask: "How is this supposed to be taken?"
- Right time: Are you supposed to take this with food? At bedtime? Every 6 hours? Timing matters. Missing a dose or taking two at once can throw off your whole treatment. Use your phone to set reminders or keep a simple paper log.
- Right reason: Why are you taking this? Not just "for pain"-but "for high blood pressure," "for infection," or "to prevent blood clots." If you can’t explain why you’re on it, you might be on the wrong one. Studies show patients who understand their reason for taking a drug reduce inappropriate use by nearly 30%.
- Right documentation: Who wrote down that you got this medicine? If it’s not recorded, the next provider might give you another dose-and you could end up with too much. Ask: "Will this be written in my chart?"
- Right response: What should you feel? What side effects are normal? What’s a red flag? If you’re on blood thinners, you should watch for unusual bruising. If you’re on insulin, you should know the signs of low blood sugar. Track how you feel. If something’s off, speak up.
Adverse Drug Event (ADE) - What It Really Means
You might hear "side effect" and think it’s just a minor annoyance-like dry mouth or drowsiness. But an adverse drug event (ADE) is anything harmful that happens because of a medicine. That includes allergic reactions, overdoses, drug interactions, and even mistakes made by the pharmacy or hospital.
The CDC says ADEs are one of the top causes of preventable hospital visits. Some ADEs are unavoidable-like a rare allergy. But many aren’t. A 2023 report found that 37% of ADEs in older adults were linked to poor communication between providers and patients. If you know what an ADE is, you’re more likely to notice early warning signs: nausea you didn’t expect, confusion after a new pill, or swelling where you weren’t swollen before.
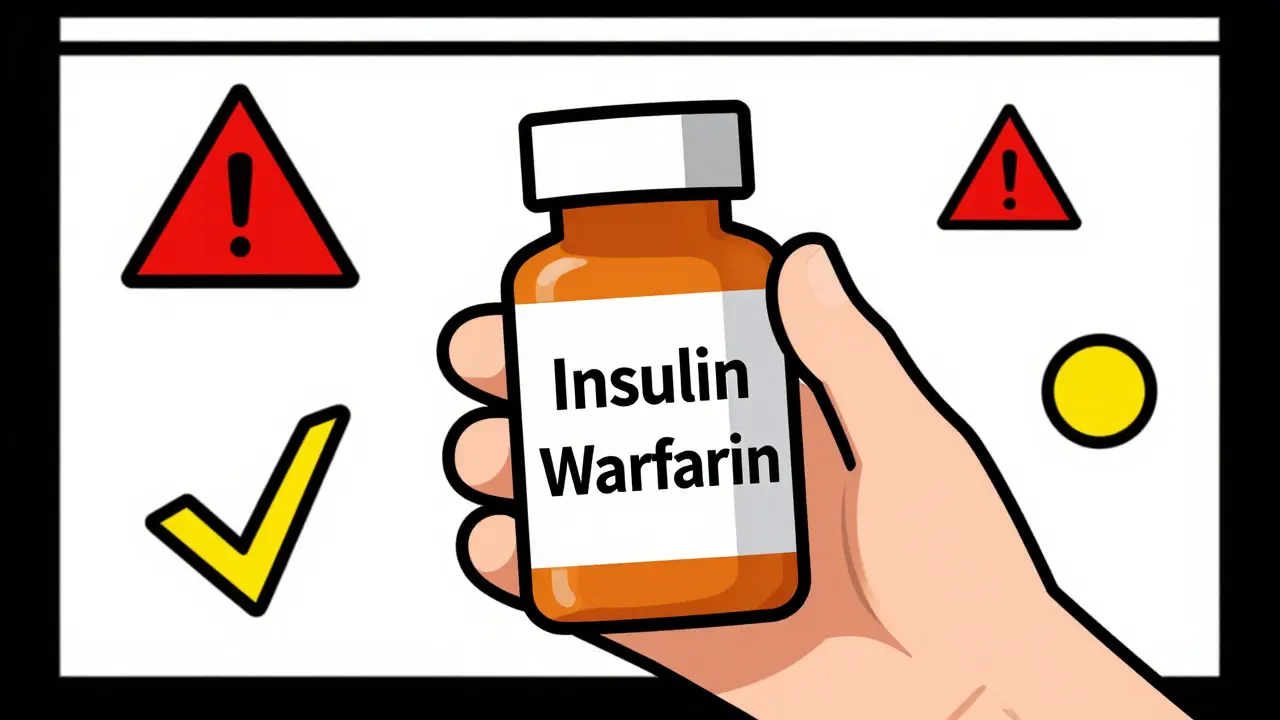
High-Alert Medications - When You Need to Be Extra Careful
Not all drugs are created equal. Some are so powerful that even a small mistake can lead to death. These are called high-alert medications. The Institute for Safe Medication Practices (ISMP) keeps a list. The most common ones include:
- Insulin (even a tiny bit too much can crash your blood sugar)
- Blood thinners like warfarin or apixaban (too much = internal bleeding)
- Opioids like oxycodone or fentanyl (too much = stopped breathing)
- IV potassium (can stop your heart if given too fast)
- Chemotherapy drugs (extremely toxic if dosed wrong)
These drugs account for 67% of fatal medication errors. If you’re prescribed one, don’t just take it. Ask: "Is this a high-alert drug?" Then ask how to spot trouble. For example, if you’re on warfarin, you should know your INR number and when to call your doctor. If you’re on insulin, you should always have a glucagon kit nearby.
Close Call - Why It Matters Even If Nothing Went Wrong
A close call is when something almost went wrong-but didn’t. Maybe the pharmacist caught the wrong dose before you left. Maybe the nurse double-checked your name before giving the shot. These aren’t "lucky escapes." They’re warnings.
When a close call happens, it means the system almost failed. And if it failed once, it could fail again. If you experience one-even if you didn’t get hurt-tell someone. Say: "I think there was a mistake, but it was caught." That feedback helps hospitals fix their processes. The VA reports that close calls are the best early warning system we have for preventing real harm.
Sentinel Events - When a Mistake Costs a Life
A sentence event is the worst-case scenario: a death or serious injury caused by a medical error. The Joint Commission defines it as an event that "should never happen." Medication errors are one of the leading causes of sentinel events. A patient getting the wrong drug, the wrong dose, or the wrong route can be fatal.
These aren’t rare. In 2023, the CDC reported that medication errors contributed to over 1,700 sentinel events in U.S. hospitals. That’s not just numbers-it’s someone’s parent, sibling, or friend. The good news? Most of these could have been stopped if the patient had known how to ask the right questions.
Why This Matters More Than Ever
More people are taking more medications than ever. The average American over 65 takes four prescription drugs. Many take five or more. That’s a recipe for mix-ups. Add in language barriers, low health literacy, or rushed appointments-and you’ve got a perfect storm.
Here’s the hard truth: Only 12% of U.S. adults have the health literacy needed to understand medication instructions. That means most people are guessing. But you don’t have to be one of them. Knowing these terms gives you power. You’re not just a passive receiver of pills-you’re a partner in your own safety.
Studies show patients who use these terms reduce their risk of harm by up to 50%. That’s not a guess. That’s from research by the American College of Obstetricians and Gynecologists. Dr. Michael Cohen of ISMP found that patients who could explain the "right reason" for their meds cut their risk of getting the wrong one by 37%.
What You Can Do Today
You don’t need to memorize every term. Just start with these three actions:
- When you get a new prescription, ask: "What is this for?" and "Is this a high-alert drug?"
- Before you take any pill, check the name, dose, and time against your list or app.
- If you feel something strange after taking a new medicine, write it down and call your provider the same day.
Use your phone. Download a free medication tracker like Medisafe (used by over 8 million people). Set reminders. Take a picture of your pill bottle. Keep a small notebook. These small steps add up.
And if you’re helping someone else-like a parent, spouse, or friend-help them learn these terms too. Medication safety isn’t just personal. It’s relational. It’s about who’s around you, who’s watching out for you, and who’s brave enough to ask: "Are you sure?"
What are the Eight Rights of Medication Safety?
The Eight Rights are: right patient, right medication, right dose, right route, right time, right reason, right documentation, and right response. These are verification steps patients and providers can use together to prevent medication errors. They go beyond the older Five Rights by adding focus on why the drug is needed and how the body responds to it.
What’s the difference between a side effect and an adverse drug event?
A side effect is a known, expected reaction to a drug-like drowsiness from an antihistamine. An adverse drug event (ADE) is any harm caused by a medicine, whether it’s an allergic reaction, overdose, interaction with another drug, or a mistake in how it was given. All ADEs are harmful; not all side effects are.
Why do I need to know the generic name of my medicine?
Generic names are the actual chemical names of drugs. Brand names change depending on the manufacturer. Knowing the generic name (like "lisinopril") helps you avoid getting the same drug twice under different brand names. It also helps you spot look-alike drugs-like "Hydromorphone" vs. "Hydrocodone"-which can cause dangerous mix-ups.
Can I refuse a medication if I’m not sure about it?
Yes. You have the right to ask questions before taking any medication. If you’re unsure about the name, dose, or reason, say: "I’d like to double-check this with my doctor before taking it." Providers expect this. Refusing to take a drug you don’t understand is a safety behavior-not a disruption.
How can I track my medications if I’m on several?
Use a simple list: write down the name (generic and brand), dose, time, and reason for each drug. Use a free app like Medisafe or MyTherapy to set alarms. Take a photo of your pill organizer. Bring this list to every appointment. Studies show patients who track their meds reduce dosing errors by 31% and improve adherence by 42%.
What’s Next?
Medication safety isn’t a one-time lesson. It’s a habit. Start small. Ask one question at your next appointment. Write down one thing you didn’t understand. Talk to someone you care about about their meds. The more you use these terms, the more natural they become. And the safer you’ll be.
The system isn’t perfect. But you don’t have to wait for it to fix itself. You can start protecting yourself today-with just a few words and the courage to ask: "Are you sure?"