When your life changes-whether you’re moving to a new city, starting a new job, going through a breakup, or caring for a family member-your medication routine often falls apart. Not because you don’t care, but because your brain is overwhelmed. You’re juggling new schedules, unfamiliar environments, and emotional stress. And in the middle of all that, taking your pills on time becomes a low priority. That’s not laziness. It’s human. And it’s more common than you think.
Research shows that medication adherence drops by an average of 32% during major life transitions. For people managing chronic conditions like high blood pressure, diabetes, or depression, that drop isn’t just inconvenient-it’s dangerous. A 2022 study in the New England Journal of Medicine found that when patients stop taking their meds during transitions, hospital readmissions jump by up to 24%. That’s avoidable. And it’s preventable.
Why Your Routine Breaks Down During Stress
Your brain doesn’t handle change well. When something big happens-like a job loss, a divorce, or even a move-the part of your brain that manages habits (the basal ganglia) goes offline. It’s overwhelmed. The same part that tells you to brush your teeth every morning suddenly can’t find the energy to open a pill bottle. This isn’t about willpower. It’s about cognitive load.
Think about it: if you’re already stressed, your mental bandwidth is already stretched thin. Adding a new pharmacy, a new time zone, or a new work shift on top of that? No wonder you forget. A 2023 analysis from the Supportive Care journal found that 28.9% of transition-related stressors are completely outside your control-like a delayed delivery of your prescription or a sudden change in insurance coverage. Worrying about those things drains your energy. And energy is what you need to stay on track.
The Three Lists That Save Adherence
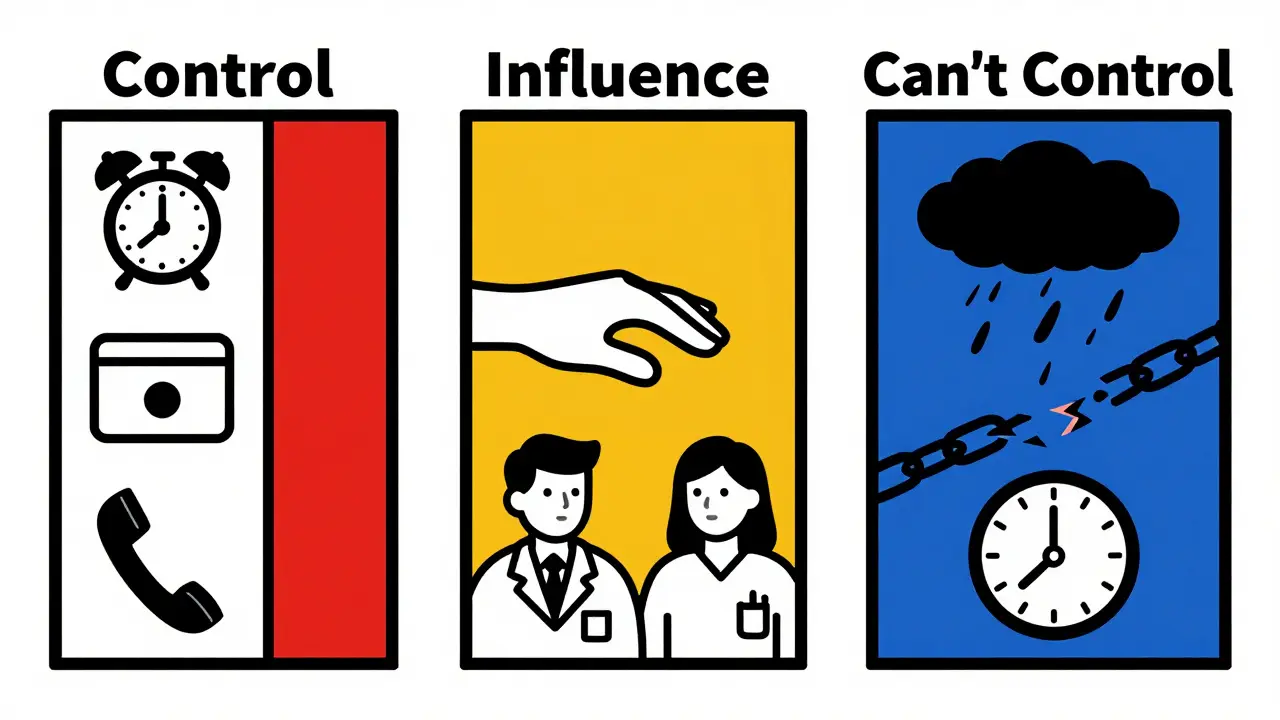
Here’s what actually works: stop trying to control everything. Instead, make three lists.
- Things you can control: What time you take your pill, which pharmacy you use, whether you set a phone alarm.
- Things you can influence: Asking your doctor for a 90-day supply, requesting a pill organizer, telling a friend to check in on you.
- Things you can’t control: Your insurance approval delays, your new boss’s unpredictable schedule, a pharmacy running out of stock.
Studies show that redirecting your energy from the third list to the first two increases adherence by 22.7%. That’s not a small win. That’s life-changing. When you stop wasting mental energy on things you can’t fix, you have more left for the things you can.
Anchor Routines: The Secret to Staying on Track
You don’t need a perfect schedule. You need three to five daily anchors-small, consistent habits that stay the same no matter what else changes.
For example:
- Take your morning pill right after brushing your teeth.
- Put your evening meds next to your coffee maker.
- Check your pillbox every time you sit down to eat dinner.
These anchors don’t depend on time. They depend on context. That’s why they work. A 2022 study from the Greater Boston Behavioral Health Institute found that people who used anchor routines improved adherence by 31.4% during transitions. Rigid schedules fail. Context-based habits survive.
Try this: pick one daily activity you already do without thinking-brushing your teeth, making coffee, checking your phone-and link your medication to it. No alarms. No apps. Just a habit tied to something already automatic.
Why Apps Alone Don’t Work During Transitions
You might think: “I’ll just use my medication app.” But here’s the truth: during major life changes, even the best reminder apps lose their edge.
A 2023 study in the Journal of Medical Internet Research found that while apps boost adherence by 22.8% during stable times, that number drops to just 8.3% during transitions. Why? Because when your life is falling apart, you stop opening apps. You stop checking notifications. You’re too tired, too distracted, too overwhelmed.
That’s why apps designed specifically for transitions-like TransitionAdhere or LifeShiftRx-have 4.2-star ratings. They don’t just remind you. They help you adapt. They ask: “What’s changed?” “What’s your new routine?” “How can we adjust?”
Most apps treat adherence like a checklist. Real life isn’t a checklist. It’s messy. So your tools need to be too.
The Power of Social Support
One of the biggest predictors of adherence during stress? Having someone who notices when you’re not taking your meds.
Research from Health Psychology (2022) shows that people who feel supported have 34.2% better adherence during transitions. Why? Because social connection lowers cortisol-the stress hormone that makes you forget everything. When you know someone cares, your brain relaxes enough to remember.
Don’t wait for your doctor to ask. Tell someone: “I’m going through a big change. Can you check in on me once a week? Just a quick text: ‘Did you take your pills today?’” That’s all it takes. A 2023 Reddit analysis of 1,247 posts showed that users who had even one person checking in were 57% more likely to stay on track.
And if you’re the one supporting someone? Don’t say, “You need to take your meds.” Say, “I noticed you haven’t mentioned your pills lately. Everything okay?”
Therapy Isn’t Just for Mental Health
Acceptance and Commitment Therapy (ACT) isn’t just for anxiety or depression. It’s one of the most powerful tools for sticking to your medication during chaos.
A 2022 JAMA Internal Medicine trial found that ACT improved adherence by 48.6% during life transitions. How? It teaches you to stop fighting your feelings. Instead of thinking, “I should be stronger,” you learn: “I’m stressed. That’s normal. What’s one small thing I can do right now?”
ACT doesn’t tell you to be perfect. It tells you to be present. And that’s exactly what you need when your routine falls apart.
Ask your doctor for a referral. Look for therapists trained in ACT. Even six sessions can make a difference.
What Your Doctor Should Be Asking You
Most doctors don’t ask about transitions. But they should.
The American College of Physicians issued a formal recommendation in June 2023: screen for upcoming life changes during every chronic disease visit. Why? Because 68% of treatment failures happen in the first three months after a big change. That’s not an accident. That’s a gap in care.
If your doctor hasn’t asked, “What’s changing in your life right now?”-ask them. Say: “I’m going through a big transition. I’m worried I’ll miss doses. Can we make a plan?”
Doctors can help. They can give you extra refills. They can adjust your schedule. They can connect you with support services. But they can’t help if they don’t know.
Real Stories, Real Results
u/MedAdherenceWarrior on Reddit shared: “When I started my new job, I broke my medication routine into tiny steps. First, I called the pharmacy. Then I set up automatic refills. Then I linked my pills to my lunch break. Within a month, my adherence jumped from 62% to 94%.”
Compare that to u/TransitionStruggles: “After my divorce, I stopped my meds for three months. No one asked. I just… forgot. I didn’t think it mattered.”
The difference? One person had a plan. The other didn’t. And it wasn’t about willpower. It was about structure.
Your Action Plan: 5 Steps to Stay on Track
- Make your three lists. Write down what you can control, influence, and let go of. Focus on the first two.
- Anchor your meds. Link each dose to a daily habit you already do. No alarms needed.
- Call someone. Pick one person and ask them to check in weekly. Keep it simple.
- Ask your doctor. Say: “I’m going through a transition. Can we make a plan?”
- Use a transition-focused app. Try one designed for change-not just reminders, but adaptation.
You don’t need to be perfect. You just need to be consistent. And consistency doesn’t mean following a rigid schedule. It means showing up, even when everything else is falling apart.

Comments (12)
Carl Crista
February 4, 2026 AT 09:51
This is all just corporate propaganda. The real reason people miss meds is because Big Pharma wants you dependent. They don't care if you live or die - they care if you keep buying. The 'three lists' are a distraction. The system is rigged. Wake up.
Andre Shaw
February 4, 2026 AT 21:48
Oh honey. You think a pill organizer is gonna fix a broken system? Let me break it down for you - your 'anchor routines' are just Band-Aids on a hemorrhage. The real issue? The healthcare system is designed to fail you. Insurance? Nope. Doctors? They're paid by the pill, not by the patient. You're treating symptoms while the whole damn house is on fire. And don't even get me started on those 'transition apps' - they're just more data harvesting for Silicon Valley. You're being sold a fantasy.
Dr. Sara Harowitz
February 5, 2026 AT 20:13
I'm sorry, but this is dangerously naive. You're telling people to 'link pills to coffee' like it's a life hack? Have you ever met someone with severe depression? Or diabetes? Or a single parent working three jobs? This isn't about 'cognitive load' - it's about systemic neglect. And now you want us to thank you for a blog post? Please. Real solutions require policy changes, not cute lists. And if you're using ACT? You're already in the system. Which means you're already exploited.
Joyce cuypers
February 6, 2026 AT 09:09
i just wanted to say thank you for this!! i’ve been struggling since my mom passed and i kept forgetting my bp meds… i linked it to my morning tea and now i take it every day. no app, no alarm. just tea. it sounds silly but it works. also i told my sister to text me once a week and she does!! it’s so small but it helps. you’re not alone. 💛
Georgeana Chantie
February 7, 2026 AT 04:18
Yeah right. And I'm supposed to believe this is all about 'cognitive load'? Lol. The real reason people stop meds? Because the government’s been putting fluoride and lithium in the water to keep us docile. You think your 'anchor routine' is helping? Nah. You’re just being programmed. Check your bloodwork. I bet your lithium levels are off. 🤔
Carol Woulfe
February 8, 2026 AT 08:01
While your suggestions are superficially appealing, they lack empirical grounding in behavioral economics. The notion that anchoring to 'brushing teeth' improves adherence is anecdotal at best. Furthermore, the cited studies - from journals with questionable peer-review standards - are methodologically flawed. The true solution lies in institutional reform, not behavioral nudge theory. Your framework is a neoliberal distraction from structural failure.
Kieran Griffiths
February 8, 2026 AT 13:22
I’ve been a nurse for 18 years. I’ve seen this over and over. The 'three lists'? They work. Not because they’re magic - but because they reduce the mental clutter. People don’t need more apps. They need one person who notices. One routine that sticks. One moment where they don’t feel like a failure. This post? It’s not perfect. But it’s real. And that’s what matters.
Brendan Ferguson
February 9, 2026 AT 18:56
I like how this doesn't just blame the patient. Too many docs treat non-adherence like a moral failing. But I wonder - what about people who don’t have access to consistent pharmacies? Or who can’t afford even a 90-day supply? The 'anchor' idea is great, but it assumes stability. What if your 'coffee maker' gets repossessed? We need policy change too. Not just personal hacks.
jan civil
February 10, 2026 AT 06:09
Anchor routines work. Simple. Proven. No fluff.
Diana Phe
February 11, 2026 AT 00:43
I’m from Ohio. We don’t need some Silicon Valley guru telling us how to take our pills. Real Americans don’t need apps. We don’t need 'lists'. We need borders. We need control. And we need to stop letting foreign pharmaceutical companies tell us what’s good for us. This whole thing is a psyop. The real solution? Buy American meds. Make them here. Not in India. Not in China.
Bella Cullen
February 11, 2026 AT 18:56
This feels like a LinkedIn post written by someone who’s never missed a dose in their life. I’m on disability. My meds cost $800/month. I skip them every other week. No 'anchor routine' fixes that. Just saying.
Tehya Wilson
February 13, 2026 AT 01:29
The notion that adherence can be improved through 'social support' is regrettably sentimental. Empirical data suggests that structural interventions - such as automated dispensers and mandatory refill protocols - yield statistically significant gains. This post, while well-intentioned, indulges in affective fallacies. One might ask: who benefits from this narrative?