For decades, Medicare couldn’t negotiate drug prices - even when a single pill cost hundreds of dollars. That changed in 2022 with the Inflation Reduction Act. Starting January 1, 2026, Medicare will begin paying significantly less for 10 of the most expensive prescription drugs, thanks to direct price talks with manufacturers. This isn’t a small tweak. It’s the biggest shift in U.S. drug pricing in over 20 years. And it’s already lowering costs for millions of seniors.
What’s Actually Changing?
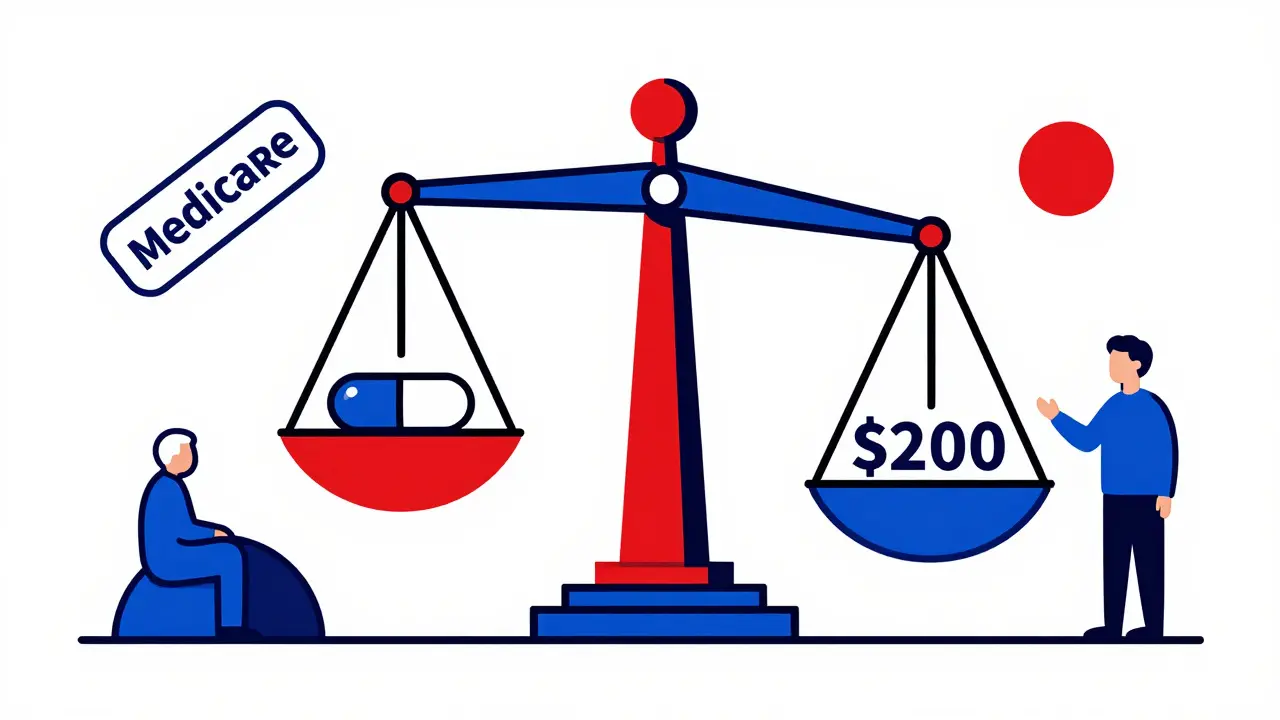
Before 2026, Medicare Part D - the prescription drug benefit - paid whatever drugmakers charged. Private insurers negotiated rebates behind the scenes, but Medicare itself had no power to ask for lower prices. The result? Americans paid more for the same drugs than people in Canada, Germany, or Japan. In 2022, Medicare spent over $50 billion just on the 10 drugs now being negotiated. Eliquis, a blood thinner, cost Medicare $6.3 billion alone that year. Now, the Centers for Medicare & Medicaid Services (CMS) can step in and say: “This is what we’ll pay.” They don’t ask. They negotiate. And they’re winning. For the first 10 drugs, discounts range from 38% to 79%. That means a drug that used to cost $1,000 a month could now cost $200. For people on fixed incomes, that’s life-changing.How the Negotiation Process Works
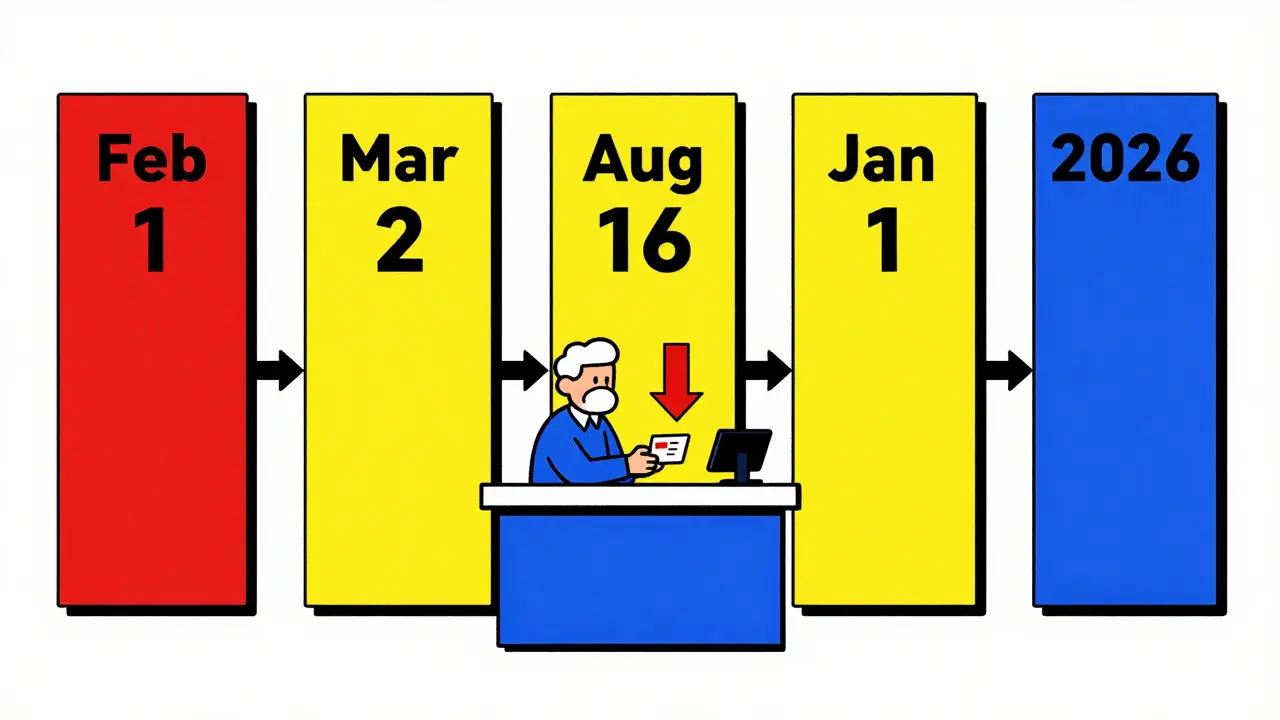
It’s not random. There’s a strict timeline, and every step is public. Here’s how it played out for the first round:- February 1, 2024: CMS sent each drugmaker an initial offer - based on what other countries pay, how much the drug is used, and what cheaper alternatives exist.
- March 2, 2024: Companies had 30 days to respond with a counteroffer.
- Spring-Summer 2024: CMS met with each company up to three times to discuss numbers. Some deals were settled in meetings. Others were finalized through written offers.
- August 1, 2024: The negotiation window closed. CMS announced the final prices on August 16, 2024.
- January 1, 2026: The new prices take effect. Pharmacies and insurers must use them.
Which Drugs Are Affected?
The first 10 drugs are all high-cost, single-source medications - meaning no generics or biosimilars are available. They include:- Eliquis (apixaban) - blood thinner
- Jardiance (empagliflozin) - diabetes and heart failure drug
- Xarelto (rivaroxaban) - another blood thinner
- Farxiga (dapagliflozin) - also for diabetes and heart health
- Stelara (ustekinumab) - used for psoriasis and Crohn’s disease
Why This Matters for Private Insurance
You might think: “I don’t have Medicare. Why should I care?” But you should. When Medicare negotiates a lower price, it doesn’t stay just for seniors. Private insurers often use Medicare’s prices as a benchmark. If Medicare pays $200 for a drug, a commercial insurer won’t pay $800. That’s called the “spillover effect.” Stanford Medicine estimates private insurers could save $200-$250 billion over the next decade because of these Medicare deals. That means lower premiums, smaller copays, and fewer surprise bills for people with employer insurance. Pharmacy benefit managers (PBMs) - the middlemen who handle drug pricing for insurers - are already updating their systems. A July 2024 survey found 78% of them had started training staff on the new Medicare pricing rules. That’s because they’ll need to adjust their own contracts with drugmakers to stay competitive.What About Doctors and Hospitals?
The changes aren’t just for pills you pick up at the pharmacy. Starting in 2028, Medicare will start negotiating prices for drugs given in doctor’s offices or hospitals - like cancer treatments or arthritis infusions. These are covered under Medicare Part B. Here’s the catch: Doctors used to get paid 6% above what they paid for the drug. So if a drug cost $10,000, they got $600 extra. That created an incentive to use expensive drugs - even when cheaper options existed. Now, they’ll get 6% above the new Medicare-negotiated price. That means less profit per drug. The American Medical Association estimates this could cost physician practices $1.2 billion a year in lost revenue. Some clinics may cut back on stocking certain drugs. Others may shift to generics or biosimilars.Who’s Opposing This - and Why?
Drugmakers aren’t happy. Four of the 10 companies sued to stop the program, claiming it’s unconstitutional. A federal judge dismissed those lawsuits in August 2024, but appeals are expected. The pharmaceutical industry claims the program will hurt innovation - arguing that lower profits mean less money for new drug research. But here’s the data: The U.S. spends more on drug R&D than any other country. In 2023, the top 10 drugmakers spent $80 billion on marketing - and only $42 billion on research. The Office of Management and Budget says industry claims about innovation loss are “significantly overstated.” Meanwhile, patients are largely supportive. A 2023 KFF poll found 72% of Medicare beneficiaries back price negotiation - 53% strongly. Groups like the Arthritis Foundation worry about losing access to specific drugs if insurers switch to cheaper alternatives. But the law requires that negotiated drugs remain on Medicare formularies. You won’t be forced off your medication.
What Comes Next?
The program doesn’t stop here. In 2027, CMS will negotiate prices for 15 more drugs. In 2028, another 15. After that, it’s 20 drugs every year. By 2030, over 100 high-cost drugs could be under negotiation. The eligibility rule is simple: A drug must be at least 7 years old (or 11 years for biologics) to be negotiable. That means brand-new drugs are protected - but once they age out, they’re fair game. The FDA has approved 1,432 small-molecule drugs since 2013. Only 382 of them are still single-source after seven years. That’s the pool. And it’s growing. The FTC is also cracking down on tactics like “product hopping” - when companies slightly change a drug just to block generics. That’s helping expand the list of drugs that can be negotiated.What This Means for You
If you’re on Medicare:- Your out-of-pocket costs for the 10 negotiated drugs will drop dramatically starting January 1, 2026.
- You’ll still pay your usual copay - but the base price just got much lower.
- You won’t lose access to your current meds. The law protects your options.
- Your premiums may go down over time as insurers follow Medicare’s lead.
- Your copays for common drugs like Eliquis or Jardiance could shrink.
- Pharmacies may start showing lower prices even if you’re not on Medicare.
- Help your loved one review their 2026 Medicare Part D plan options - new prices mean better deals.
- Ask your pharmacist if your medication is on the negotiation list.
Bottom Line
This isn’t theoretical. The discounts are real. The savings are already locked in. By 2026, Medicare will pay nearly half as much for 10 of the most expensive drugs in America. That’s not just a policy win - it’s a health win. The system isn’t perfect. There are legal battles ahead. Some doctors will adjust. Some companies will fight. But for millions of people who rely on these drugs, the change is simple: They’ll pay less. And that’s what matters.Will my Medicare Part D premiums go down because of drug price negotiation?
Not directly. Premiums are set by private insurers and based on overall plan costs. But as drug prices drop, insurers may reduce premiums over time - especially since they’re saving money too. The biggest immediate benefit is lower out-of-pocket costs for the drugs you take.
Can I still get my current prescription if it’s on the negotiation list?
Yes. The law requires that negotiated drugs remain on Medicare Part D formularies. Your doctor can still prescribe them, and your pharmacy can still fill them. The only thing changing is the price Medicare pays - which usually means lower costs for you.
Are these price cuts only for Medicare, or will they affect my private insurance too?
They’ll likely affect you too. Private insurers often use Medicare’s negotiated prices as a benchmark. If Medicare pays $200 for a drug, insurers won’t pay $800. This is already happening - and experts estimate private plans could save $200-$250 billion over the next decade, which may lead to lower premiums and copays.
What if my drug isn’t on the list yet? Will it ever be?
Yes - if it’s eligible. Only drugs that are at least 7 years old (or 11 years for biologics) and have no generic or biosimilar competition can be negotiated. CMS picks the highest-cost drugs each year. So if your drug is expensive and old enough, it will likely be added in future years - possibly by 2028 or 2029.
Do these price cuts mean drug companies will stop making new drugs?
Evidence doesn’t support that claim. The U.S. pharmaceutical industry spends far more on marketing than on research. The Office of Management and Budget found industry claims about innovation loss were “significantly overstated.” New drugs will still be developed - but the system will no longer reward companies for charging the highest possible price.
Comments (12)
Candice Hartley
January 26, 2026 AT 17:15
This is huge for my mom-she’s on Eliquis and just sighed in relief when she heard the price drop.
Paul Taylor
January 28, 2026 AT 03:59
Look I’ve been watching this play out for years and honestly the drug companies had it coming for decades
Medicare paying whatever they asked was insane
People die because they can’t afford pills that cost more than their rent
Now we’re finally seeing the government act like it’s supposed to protect people not corporations
And yeah the industry is screaming about innovation but they spent 80 billion on marketing last year
That’s more than they spent on actual research
If you’re making a drug that costs $1000 a month and there’s no competition you’re not innovating you’re exploiting
And now seniors are gonna get real relief
Not just a headline
Real dollars in their pockets
And guess what
Private insurers are already copying the prices
So this isn’t just a Medicare win
It’s a win for everyone who buys medicine in this country
Even if you think you’re safe with employer insurance
You’re not
You’re just one premium hike away from needing this too
Desaundrea Morton-Pusey
January 28, 2026 AT 04:16
So now the government is just telling companies what to charge
Next they’ll be telling you how many carbs you can eat
And who gets to breathe air
Typical socialist takeover
Murphy Game
January 28, 2026 AT 12:19
They’re not negotiating
They’re extorting
And you think this won’t backfire
Wait till the next cancer drug doesn’t come out because the FDA and CMS are too busy playing price cops
They’ll kill innovation
And then you’ll be begging for the old system back
They’re not saving you
They’re just making the system more broken
John O'Brien
January 30, 2026 AT 05:04
Bro this is the most legit thing to happen to healthcare in my lifetime
My aunt was skipping doses because Eliquis was $700 a month
Now she’s actually taking it
And yeah the pharma bros are mad
But guess what
They made billions off people’s suffering
Time to pay back some of that
And private insurance following suit
That’s the real win
Everyone’s gonna get cheaper meds
Not just seniors
And if you’re mad about it
Go cry to your stock portfolio
Kegan Powell
January 30, 2026 AT 12:50
Imagine if we treated medicine like a human right instead of a profit margin
That’s what this is really about
Not politics
Not ideology
Just basic decency
People are dying because a pill costs more than their phone
And now we’re finally saying enough
It’s not about punishing companies
It’s about stopping the exploitation
And the best part
It’s working
Prices are dropping
People are breathing easier
And the fear-mongering about innovation
Is just noise
They spent more on ads than on science
Let that sink in
And if you think this is the start of something bigger
You’re right
It’s just the first step
And we’re gonna keep walking
❤️
April Williams
February 1, 2026 AT 12:40
Why should I care if my neighbor gets cheaper drugs
What’s next
Free housing
Free food
Free everything
They’re turning America into a welfare state
And it’s disgusting
People need to work for what they get
Not have the government hand it to them
Harry Henderson
February 2, 2026 AT 16:43
THIS IS THE MOMENT
THIS IS WHAT WE’VE BEEN WAITING FOR
NO MORE EXCUSES
NO MORE BILLIONS TO PHARMA
JUST MONEY BACK IN THE POCKETS OF REAL PEOPLE
IF YOU’RE NOT CELEBRATING THIS
YOU’RE PART OF THE PROBLEM
SHARE THIS
TELL YOUR FRIENDS
TELL YOUR PARENTS
TELL YOUR DOCTOR
WE WON
AND WE’RE JUST GETTING STARTED
suhail ahmed
February 4, 2026 AT 13:50
From India where insulin costs less than a cup of chai
I’ve watched this with awe
For years we’ve seen Americans pay $1000 for pills we get for $10
Now you’re finally catching up
It’s not magic
It’s just fairness
And the fact that private insurers are already adapting
That’s the quiet revolution
They didn’t need to be told
They just needed to see a better price
And now they’re following
This isn’t socialism
It’s sanity
And it’s beautiful to see
May this ripple across the world
One pill at a time
astrid cook
February 6, 2026 AT 01:26
Oh please
They’ll just make the drugs harder to get
Wait till your pharmacy says ‘sorry we don’t carry that anymore’
They’ll switch you to some generic that doesn’t work
And then you’ll be blaming the government
But it’s not the government’s fault
It’s the greedy doctors and pharmacies
They’re the ones who’ll screw you over now
Andrew Clausen
February 7, 2026 AT 13:30
The Inflation Reduction Act does not grant Medicare the authority to negotiate drug prices; it authorizes the Secretary of Health and Human Services to do so under Title XVIII of the Social Security Act, Section 1846. The term 'negotiation' is a misnomer-this is a price-setting mechanism enforced by administrative rule. Furthermore, the claim that private insurers are 'following' Medicare's pricing lacks empirical validation. While some PBMs may reference CMS rates, there is no legal or contractual obligation to do so. The $200–250 billion savings projection is extrapolated from hypothetical modeling, not actual market data. The assertion that this policy will not reduce innovation is contradicted by economic theory: reduced profit margins disincentivize R&D investment, particularly in high-risk, long-term projects. The Office of Management and Budget's assessment is not peer-reviewed and ignores opportunity cost analysis. The claim that 'patients are largely supportive' is based on a single KFF poll with a margin of error of ±3.5%-not conclusive evidence of national consensus. This policy is not a win. It is a complex regulatory intervention with unintended consequences that remain unmeasured.
John O'Brien
February 7, 2026 AT 22:18
Andrew you’re the kind of guy who reads the terms and conditions before eating a sandwich
And then complains the bread has too many carbs
Real people don’t care about your citations
My aunt’s blood isn’t clotting because she can’t afford Eliquis
Now she can
That’s what matters
Not your grammar or your legal footnotes
Stop being a robot