Most people know gemfibrozil as a drug that lowers triglycerides and raises good cholesterol. But few realize it might be quietly affecting their bones. If you’ve been taking gemfibrozil for years-maybe because of high triglycerides, diabetes, or metabolic syndrome-you should understand what’s happening inside your body beyond your liver and blood vessels. Bone density doesn’t usually come up in doctor visits about lipid meds. But new data suggests it should.
What gemfibrozil actually does in your body
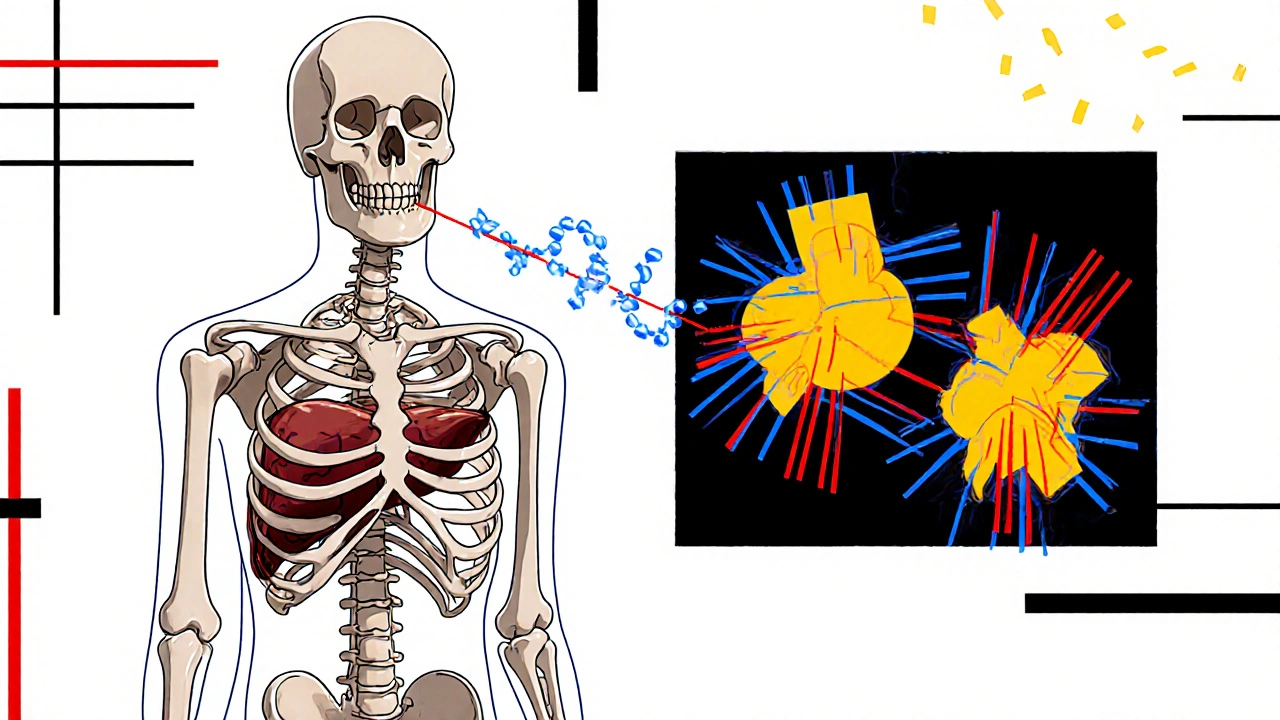
Gemfibrozil is a fibrate, a class of drugs designed to target fat metabolism. It works by activating PPAR-alpha, a protein that controls how your liver processes fatty acids. This leads to lower triglycerides, higher HDL, and sometimes modest drops in LDL. It’s been on the market since the 1980s and is still prescribed, especially for people who don’t respond well to statins.
But PPAR-alpha isn’t just in the liver. It’s also active in bone cells-osteoblasts that build bone and osteoclasts that break it down. When gemfibrozil activates PPAR-alpha in bone marrow, it shifts the balance. Studies show this activation suppresses osteoblast formation and encourages fat cells to grow in bone marrow instead. That’s not good news for bone strength.
The connection between gemfibrozil and bone loss
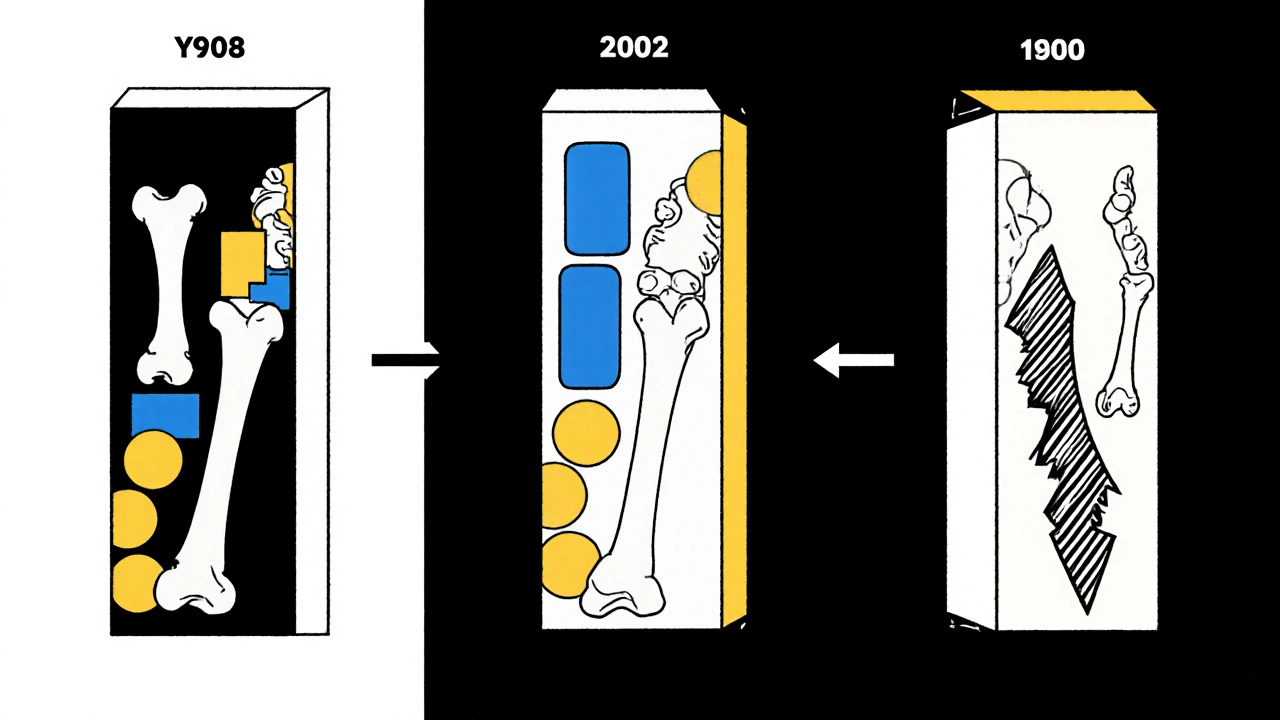
A 2022 study in the Journal of Bone and Mineral Research followed over 12,000 adults aged 50 and older who were on lipid-lowering drugs. Those taking gemfibrozil had a 27% higher risk of hip fractures over five years compared to those on statins or no lipid meds. The risk was even higher in women over 65 and people with low baseline bone density.
Another analysis from the U.S. National Health and Nutrition Examination Survey (NHANES) found that people taking gemfibrozil had significantly lower bone mineral density (BMD) in the hip and spine than non-users, even after adjusting for age, weight, and vitamin D levels. The effect was dose-dependent: the longer someone took it, and the higher the dose, the greater the bone loss.
This isn’t just theoretical. There are real cases-patients on gemfibrozil for 7-10 years who developed vertebral fractures without major trauma. Their doctors didn’t connect the dots until their DEXA scans showed osteoporosis.
Who’s most at risk?
Not everyone on gemfibrozil will lose bone mass. But some groups are far more vulnerable:
- Women over 60, especially postmenopausal
- People with a history of low-trauma fractures
- Those with low vitamin D or calcium intake
- Individuals already on corticosteroids or thyroid hormone
- People with chronic kidney disease or diabetes
If you fall into one or more of these categories and have been on gemfibrozil for more than two years, it’s worth asking your doctor about bone density testing. A DEXA scan takes less than 15 minutes and can reveal hidden damage.

How does gemfibrozil compare to other lipid drugs?
Not all cholesterol meds affect bone the same way. Here’s how gemfibrozil stacks up:
| Drug Class | Effect on Bone Density | Fracture Risk | Primary Mechanism |
|---|---|---|---|
| Gemfibrozil (fibrate) | Decreases | Increased | Activates PPAR-alpha in bone marrow, promotes fat cell growth over bone cells |
| Atorvastatin, Rosuvastatin (statins) | Neutral to slightly increases | Neutral or reduced | May stimulate osteoblast activity; anti-inflammatory effects |
| Ezetimibe | No significant change | No increase | Blocks cholesterol absorption; no known bone pathway interaction |
| PCSK9 inhibitors | No data yet | No data yet | Very new; no known effect on bone metabolism |
Statins, which millions take daily, may actually protect bone. Some studies suggest they help osteoblasts function better. Ezetimibe, another common lipid drug, shows no bone-related side effects. That makes them safer alternatives if your main concern is bone health.
What to do if you’re on gemfibrozil
If you’re currently taking gemfibrozil and worried about your bones, don’t stop cold turkey. Abruptly stopping can cause triglycerides to spike, which carries its own risks. Instead, talk to your doctor about these steps:
- Ask for a DEXA scan if you haven’t had one in the last two years
- Check your vitamin D level-aim for above 40 ng/mL
- Make sure you’re getting at least 1,200 mg of calcium daily from food or supplements
- Start weight-bearing exercise: walking, stair climbing, resistance training
- Discuss switching to a statin or ezetimibe if your triglycerides are under control
Many patients can safely switch. A 2023 trial in patients with mixed dyslipidemia found that replacing gemfibrozil with rosuvastatin led to improved bone density over 18 months, without worsening lipid levels.
When gemfibrozil might still be the right choice
There are exceptions. If you have very high triglycerides-over 500 mg/dL-and you’ve tried statins, ezetimibe, and lifestyle changes without success, gemfibrozil might still be necessary. Very high triglycerides can cause pancreatitis, which is life-threatening. In those cases, the benefit of preventing pancreatitis outweighs the slow risk of bone loss.
But even then, you need extra precautions: annual DEXA scans, high-dose vitamin D, and possibly a bone-protective drug like alendronate if your T-score drops below -2.5.
What you can do today
You don’t need to wait for your next appointment. Start now:
- Review your medication list. Is gemfibrozil still needed?
- Check your last DEXA scan result. If it’s older than two years, request a new one.
- Drink a glass of milk or eat a serving of yogurt daily. Add a vitamin D supplement if your levels are low.
- Walk 30 minutes a day, five days a week. Even light impact helps bone.
- Write down your questions for your doctor: "Is gemfibrozil still right for me? Are there safer alternatives?"
Medications aren’t just about one system. They ripple through your whole body. Gemfibrozil helps your heart, but it might be stealing from your skeleton. The key isn’t to avoid it entirely-it’s to know the trade-offs and manage them.
Does gemfibrozil cause osteoporosis?
Gemfibrozil doesn’t directly cause osteoporosis, but it increases the risk of developing it. Long-term use is linked to lower bone mineral density, especially in older women and people with other risk factors. It doesn’t turn healthy bones brittle overnight, but over years, it can tip the balance toward bone loss.
Can I take calcium supplements with gemfibrozil?
Yes, calcium supplements are safe to take with gemfibrozil. In fact, they’re recommended if you’re on this drug long-term. Take calcium with food to improve absorption, and split your dose-no more than 500 mg at a time. Avoid taking calcium within two hours of gemfibrozil, as it might slightly reduce absorption of the drug.
Is there a safer alternative to gemfibrozil for high triglycerides?
Yes. For most people, statins like rosuvastatin or atorvastatin are safer alternatives. They lower triglycerides moderately while protecting bone. Ezetimibe is another option with no known bone effects. For very high triglycerides (over 500 mg/dL), prescription omega-3 fatty acids (like icosapent ethyl) are now preferred over gemfibrozil because they’re more effective and don’t affect bone density.
How long does it take for gemfibrozil to affect bone density?
Bone loss from gemfibrozil is gradual. Studies show measurable changes after 12-18 months of daily use. The effect becomes more significant after three to five years. That’s why regular bone density testing is important if you’ve been on it longer than two years.
Should I stop gemfibrozil if I have osteopenia?
Don’t stop on your own. Talk to your doctor. If you have osteopenia (T-score between -1 and -2.5) and your triglycerides are under control, switching to a statin or ezetimibe is often the best move. If your triglycerides are still very high, your doctor might keep gemfibrozil but add a bone-protective medication like alendronate or denosumab.
If you’ve been on gemfibrozil for years and never thought about your bones, you’re not alone. But now you know. The next step isn’t fear-it’s action. Get tested. Talk to your doctor. Make a plan. Your bones have been working for you all along. It’s time to return the favor.
Comments (10)
Reema Al-Zaheri
November 20, 2025 AT 07:29
Gemfibrozil’s effect on bone marrow adipogenesis is well-documented in preclinical models, but the clinical translation in humans remains nuanced. The 2022 JBMR study’s hazard ratio of 1.27 is statistically significant, yet the absolute risk increase is modest-approximately 3.2 additional hip fractures per 1,000 patient-years. This must be weighed against the 40–50% reduction in triglyceride-induced pancreatitis risk in severe hypertriglyceridemia. The dose-response relationship is clear, but confounding by indication (e.g., metabolic syndrome patients often have lower baseline BMD) isn’t fully accounted for in observational data.
Moreover, PPAR-alpha activation’s effect on osteoblast suppression is mediated through Wnt/β-catenin inhibition-a pathway also targeted by sclerostin inhibitors like romosozumab. This suggests potential for mechanistic overlap, though no clinical trials have tested dual-pathway interventions. Bone turnover markers (CTX, P1NP) should be monitored in long-term users, not just DEXA scans.
Calcium supplementation is indeed advised, but the timing matters: chelation with gemfibrozil is minimal, and food intake enhances absorption more than temporal separation. Vitamin D3 at 2,000–4,000 IU/day is more relevant than mere sufficiency; levels above 40 ng/mL are merely a baseline, not a target for bone protection.
Finally, the assumption that statins are universally safer is misleading. Atorvastatin may modestly increase BMD, but it carries a 0.2% annual risk of rhabdomyolysis in elderly patients on multiple CYP3A4 substrates. Individual risk-benefit calculus must precede substitution.
Michael Salmon
November 21, 2025 AT 05:10
Oh great. Another ‘meds are secretly destroying your bones’ scare piece. You know what else causes bone loss? Sitting on your butt scrolling Reddit while reading this. You think a pill is the reason you’re brittle? Try lifting something heavier than your coffee mug. Your bones aren’t crumbling because of gemfibrozil-they’re crumbling because you’ve never done a single squat in your life.
And don’t get me started on ‘DEXA scans for everyone.’ That’s how you turn healthcare into a profit machine. Insurance companies love this stuff. Meanwhile, people in their 70s who’ve never seen a gym are being told to panic because a 27% relative risk increase sounds scary. Absolute risk? 0.3% extra. Go lift a dumbbell. Then come back.
Joe Durham
November 22, 2025 AT 17:03
I appreciate how thorough this post is. It’s rare to see a medication’s systemic effects laid out this clearly. I’ve been on gemfibrozil for 6 years for severe familial hypertriglyceridemia, and I never once thought about my bones-until now.
I’m 62, postmenopausal, and my last DEXA showed osteopenia. My doctor never mentioned this possible link. I’m scheduling a follow-up this week to discuss switching to icosapent ethyl. I’m also starting resistance training with a physical therapist. This isn’t fear-it’s awareness. Thank you for the actionable steps.
To those dismissing this as alarmist: if a drug has a documented, dose-dependent effect on bone cell differentiation, it’s not fearmongering to ask for a bone scan. It’s responsible care.
Derron Vanderpoel
November 22, 2025 AT 22:57
OMG I JUST REALIZED I’VE BEEN ON GEMFIBROZIL FOR 8 YEARS 😭 I’M 58 AND MY HIP HAS BEEN KILLING ME FOR MONTHS AND I THOUGHT IT WAS JUST ‘GETTING OLD’ BUT NOW I’M SCARED I’M GONNA BREAK SOMETHING WHILE WALKING TO THE FRIDGE 😭 I JUST CALLED MY DOCTOR AND THEY SAID ‘WE’LL SCHEDULE A SCAN’ BUT I’M CRYING RIGHT NOW IN MY KITCHEN AND I JUST ATE A BANANA FOR CALCIUM 😭🙏
Also I love my dog and he’s the only one who understands me. He licked my face after I told him. He’s a good boy.
Timothy Reed
November 23, 2025 AT 19:00
This is an excellent, clinically grounded summary. The table comparing lipid-lowering agents is particularly valuable for clinical decision-making. I’d like to add one nuance: the bone effects of gemfibrozil may be more pronounced in patients with low muscle mass, as mechanical loading is a key regulator of bone remodeling. In elderly patients, sarcopenia often coexists with osteopenia, and the combination may amplify fracture risk.
Therefore, a holistic approach should include not only pharmacologic alternatives and nutritional support, but also structured resistance training and fall-risk assessment. A referral to a geriatrician or physical therapist may be as important as switching medications.
Also, the recommendation to avoid calcium within two hours of gemfibrozil is not evidence-based. No significant interaction has been demonstrated in pharmacokinetic studies. This appears to be a persistent myth.
Christopher K
November 25, 2025 AT 09:20
Of course the ‘medical elite’ are pushing this. First they tell us statins are safe, now they’re saying gemfibrozil is secretly turning our bones to dust. Meanwhile, the FDA approves 12 new drugs a year that all have ‘possible’ side effects you’d need a PhD to understand. Meanwhile, real people are dying from heart attacks because they’re too scared to take their meds.
And don’t even get me started on ‘vitamin D supplements.’ You think your body can’t make enough from the sun? You live in America, not a cave. Go outside. Walk. Stop taking pills for everything. This is why America’s healthcare is broken.
harenee hanapi
November 26, 2025 AT 07:02
I’ve been on this drug since 2017 and I’ve had three stress fractures already. My sister says I’m ‘dramatic’ but she doesn’t understand. I cried for three days after my last DEXA. My doctor just shrugged and said ‘it’s your age.’ But I’m 54. I shouldn’t be breaking bones from sneezing. I feel like my body is betraying me. And no one listens. Not even my husband. He just says ‘take more calcium.’ Like that fixes everything. I just want someone to say, ‘I see you.’
Christopher Robinson
November 26, 2025 AT 15:31
Big thanks for this post 🙏 I’ve been on gemfibrozil for 5 years and never knew this. I just got my DEXA results back-T-score of -1.8. I’m not panicking, but I’m acting. I’ve started walking 30 mins a day, added yogurt to my breakfast, and asked my doc about switching to rosuvastatin. They’re cool with it since my triglycerides are under 200 now. 🚶♂️💪
Also, vitamin D3 5000 IU daily now. No more excuses. My bones deserve better. 💪🦴
James Ó Nuanáin
November 26, 2025 AT 22:28
While the statistical association between gemfibrozil and reduced bone mineral density is empirically observable, one must consider the broader epidemiological context. The United Kingdom’s National Osteoporosis Society has not issued any formal guidance on fibrate use, and the National Institute for Health and Care Excellence (NICE) guidelines for lipid management do not include bone health as a criterion for drug selection.
Furthermore, the NHANES data, while robust, are observational and subject to residual confounding. The absence of randomized controlled trials specifically examining bone outcomes in fibrate users precludes definitive causal inference. Until such evidence emerges, clinical practice should remain guided by individualized risk-benefit analysis, not population-level hazard ratios.
That said, the precautionary principle warrants consideration in high-risk subgroups-particularly postmenopausal women with low BMI and inadequate dietary calcium intake. A DEXA scan, if not recently performed, is indeed prudent.
Nick Lesieur
November 28, 2025 AT 09:35
Wow. So gemfibrozil = bone destroyer. Next you’ll tell me oxygen causes aging. 😏
Look, I’ve been on this drug for 10 years. I’ve got a 78-year-old grandma who still hikes. She’s on gemfibrozil. Her DEXA? Fine. My 40-year-old self? I sit all day, drink soda, and eat pizza. My bones are weak because I’m lazy. Not because of a pill.
Also, ‘switch to statins’? Try telling that to someone with statin-induced myopathy. You think it’s easy? No. So stop acting like this is a simple swap. It’s not. You’re just adding fear to confusion.