Why Seniors Fall - And Why Medications Are Often the Hidden Cause
Every year, more than 14 million older adults in the U.S. fall. About 36,000 of them die from those falls. That’s more than car crashes. And while many assume it’s just aging, weakness, or poor vision, the real culprit is often something far more preventable: the medications they’re taking. Seniors don’t fall because they’re frail - they fall because drugs are making them dizzy, slow, or confused. And most of the time, no one ever checks.
Medications That Raise Fall Risk - The Big Five
It’s not one drug. It’s classes of drugs. And they’re everywhere. If you or a loved one is 65 or older, chances are at least one of these is on the list:
- Antidepressants - Especially SSRIs like sertraline and fluoxetine, and older tricyclics like amitriptyline. These don’t just lift mood - they lower blood pressure when standing, cause drowsiness, and impair balance. A 2018 meta-analysis found people on SSRIs are over twice as likely to fall as those not taking them.
- Benzodiazepines - Drugs like diazepam (Valium), lorazepam (Ativan), and alprazolam (Xanax). These are prescribed for anxiety or sleep, but they slow reaction time, blur vision, and make coordination worse. Long-acting versions are especially dangerous. Even short-term use increases fall risk by 42%.
- Antipsychotics - Used for dementia-related agitation or psychosis, drugs like risperidone and quetiapine (Seroquel) cause dizziness, muscle stiffness, and a condition called tardive dyskinesia. These aren’t meant for long-term use in seniors - yet they’re still prescribed for months or years.
- Blood pressure meds - Beta blockers (carvedilol), ACE inhibitors (lisinopril), and diuretics (hydrochlorothiazide) are common. But when doses are too high or changed too fast, they cause orthostatic hypotension - a sudden drop in blood pressure when standing up. That’s when people feel lightheaded, stumble, and fall. It’s not the disease. It’s the treatment.
- Opioids - Painkillers like oxycodone and hydrocodone. They cause drowsiness, dizziness, and confusion. But here’s the worst part: when opioids are mixed with benzodiazepines, fall risk jumps by 150%. That’s not a small risk. That’s a red flag.
And don’t forget the over-the-counter stuff. Diphenhydramine - found in Benadryl, Tylenol PM, and sleep aids - is an anticholinergic. It dries your mouth, blurs your vision, and slows your brain. One study found that seniors taking just one anticholinergic drug had a 50% higher chance of falling. Two? The risk doubles.
Why Polypharmacy Is a Silent Killer
Taking one risky drug? Dangerous. Taking three or four? Deadly. The National Council on Aging says seniors on four or more medications have a much higher chance of falling - not because each drug is bad alone, but because they interact. One drug lowers blood pressure. Another makes you sleepy. A third messes with your balance. Together, they create a perfect storm.
It’s not just the number. It’s the duration. Many of these drugs were prescribed years ago - for anxiety, insomnia, or chronic pain - and never reviewed. Doctors assume they’re still needed. Families assume they’re safe. But the body changes with age. What worked at 60 can be dangerous at 75.
Here’s the truth: 65% to 93% of seniors who fall and get hurt were taking at least one medication known to increase fall risk. And nearly half were taking two or more.
What the Experts Say - The Beers Criteria and STOPP/START
The American Geriatrics Society doesn’t guess. They track it. Since 1991, they’ve published the Beers Criteria - a list of medications that should be avoided or used with extreme caution in older adults. The 2023 update is clearer than ever: benzodiazepines? Avoid. Tricyclic antidepressants? Avoid. Anticholinergics like diphenhydramine? Avoid. Antipsychotics for dementia? Avoid unless absolutely necessary.
Doctors also use two tools: START (Screening Tool to Alert to Right Treatment) and STOPP (Screening Tool of Older Persons’ Prescriptions). STOPP finds drugs that shouldn’t be there. START finds drugs that should be added - like vitamin D or a fall prevention program. Together, they help flip the script: from prescribing more, to prescribing less.
Dr. Michael Steinman, one of the authors of the Beers Criteria, says: “Reducing or eliminating fall-risk-increasing medications can cut fall rates by 20% to 30%.” That’s not a small win. That’s life-changing.
How to Check Your Medications - A Simple 4-Step Plan
You don’t need a PhD to protect yourself or a loved one. You just need to ask the right questions.
- Get the full list. Write down every pill, patch, and liquid - including vitamins, supplements, and OTC drugs. Don’t trust your memory. Look in the pill bottles.
- Take it to your doctor or pharmacist. Don’t say, “Is this safe?” Say, “Could any of these be making me dizzy or unsteady?” Ask specifically about the drugs listed above.
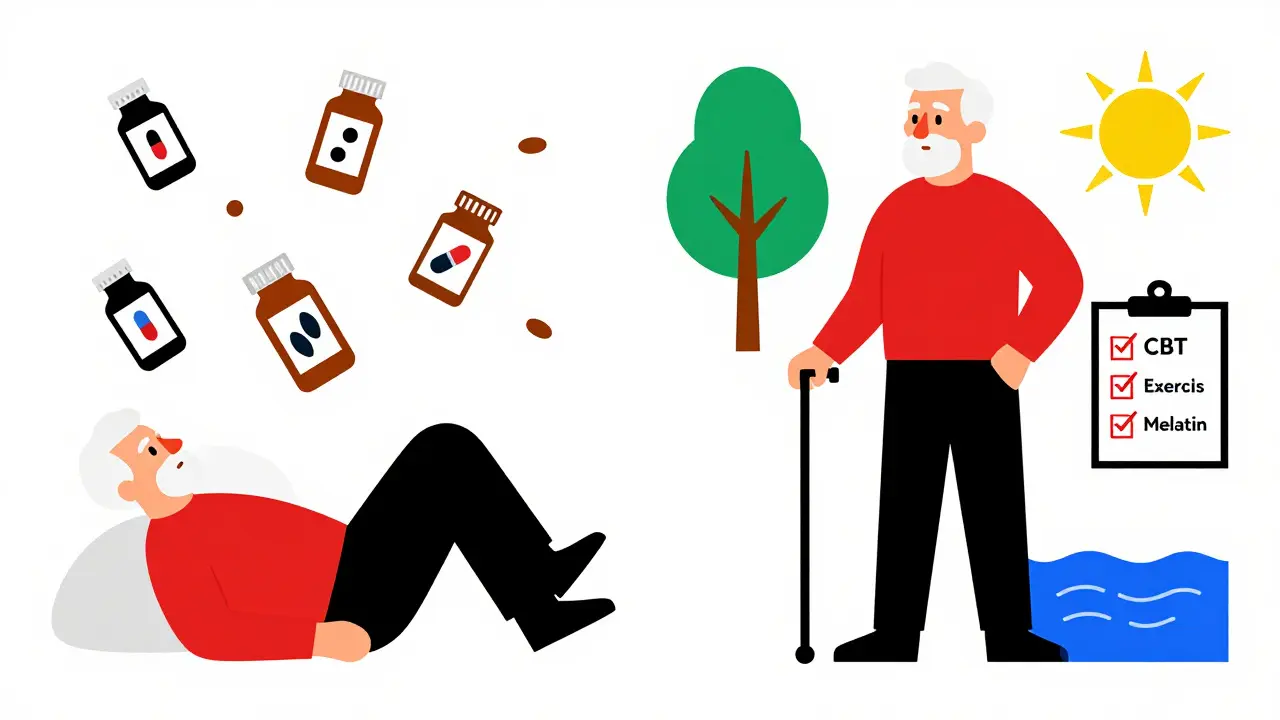
- Ask about deprescribing. Can any of these be stopped? Can the dose be lowered? Is there a safer alternative? For example, instead of a benzodiazepine for sleep, try cognitive behavioral therapy. Instead of diphenhydramine, try melatonin (with doctor approval).
- Check for orthostatic hypotension. Sit quietly for 5 minutes. Measure your blood pressure. Stand up. Wait 3 minutes. Measure again. If your systolic pressure drops 20 points or more, that’s a red flag. Tell your doctor. It’s often caused by meds - and it’s fixable.
Pharmacist-led reviews - like the HomeMeds program - have been shown to reduce falls by 22%. That’s not magic. That’s science.
What Happens When You Stop
Some people worry: “If I stop my meds, will I get worse?” The answer is often: no. You’ll get better.
One study followed seniors who stopped benzodiazepines. Within weeks, their balance improved. Their memory cleared. Their fall risk dropped. They didn’t relapse into anxiety - they learned other ways to cope.
Another found that seniors who stopped antipsychotics for dementia didn’t get more agitated - they became calmer, more alert, and more engaged. Their families noticed the difference.
Stopping doesn’t mean going cold turkey. It means working with your team to taper safely. Some drugs need weeks to come off. Others can be stopped quickly. But the key is: don’t assume you have to keep taking them forever.
The Bigger Picture - Why This Keeps Happening
Doctors aren’t careless. They’re overwhelmed. Most primary care visits last 15 minutes. Medication lists are long. There’s no time to dig into every pill.
And here’s the irony: we’ve gotten better at treating high blood pressure, depression, and pain - but worse at asking, “Is this still helping - or is it hurting?”
Only 42% of primary care doctors routinely check for medication-related fall risk. That’s not enough. We need better systems: electronic alerts when a senior is prescribed a high-risk drug. Pharmacist consultations built into routine visits. Insurance coverage for medication reviews.
But until then, you have power. You can ask. You can push. You can bring the list. You can say, “I don’t want to fall. What can we take off?”
What to Do Next
Don’t wait for a fall. Don’t wait for a hospital visit. Start today.
- Make a list of every medication you or your loved one takes.
- Bring it to your next appointment - doctor, pharmacist, or both.
- Ask: “Could any of these be causing dizziness or unsteadiness?”
- Ask: “Is there a safer option? Can we try lowering the dose?”
- Ask: “Can we stop one of these?”
Falls aren’t inevitable. They’re often preventable. And the easiest place to start? The medicine cabinet.
What are the most dangerous medications for seniors when it comes to falling?
The top offenders are antidepressants (especially SSRIs and tricyclics), benzodiazepines (like Valium and Xanax), antipsychotics (like Seroquel), blood pressure drugs (like lisinopril and hydrochlorothiazide), and opioids. Over-the-counter antihistamines like diphenhydramine (Benadryl) are also high-risk. These drugs cause dizziness, low blood pressure, drowsiness, or confusion - all leading to falls.
Can stopping a medication really reduce fall risk?
Yes. Studies show that carefully stopping or reducing high-risk medications can lower fall rates by 20% to 30%. One study found that seniors who stopped benzodiazepines improved their balance within weeks. Deprescribing isn’t about going without treatment - it’s about replacing risky drugs with safer options or non-drug approaches.
What is the Beers Criteria and why does it matter?
The Beers Criteria is a list of medications that experts say should be avoided or used with extreme caution in adults 65 and older. It’s updated every two years by the American Geriatrics Society. If a drug is on the list - like diphenhydramine or long-acting benzodiazepines - it means the risks (like falls, confusion, or death) outweigh the benefits for most seniors.
Should I stop my medication on my own if I think it’s causing falls?
No. Never stop a prescription drug suddenly - especially antidepressants, benzodiazepines, or blood pressure meds. That can cause dangerous withdrawal or rebound effects. Instead, bring your full medication list to your doctor or pharmacist. Ask for a review. Together, you can make a safe plan to reduce or stop the right drugs.
How do I know if my blood pressure drops when I stand up?
Sit quietly for 5 minutes. Have someone measure your blood pressure. Then stand up. Wait exactly 3 minutes. Measure again. If your top number (systolic) drops by 20 points or more, or your bottom number (diastolic) drops by 10 points or more, you have orthostatic hypotension. This is often caused by medications and is a major fall risk. Tell your doctor - it’s fixable.
Is it safe to take multiple medications if they were prescribed by different doctors?
No. When multiple doctors prescribe without knowing what others have written, dangerous interactions happen. A cardiologist might prescribe a blood pressure drug. A psychiatrist might add an antidepressant. A pain specialist might add an opioid. Together, they can triple your fall risk. Always have one provider - your primary doctor or pharmacist - review your full list.
Are there non-drug alternatives to these risky medications?
Yes. For anxiety or insomnia, cognitive behavioral therapy (CBT) is as effective as benzodiazepines - without the fall risk. For chronic pain, physical therapy, acupuncture, or mindfulness can help. For overactive bladder, pelvic floor exercises and timed voiding work better than anticholinergics. For depression, exercise and social engagement are powerful tools. Talk to your doctor about these options.

Comments (13)
Beth Cooper
January 31, 2026 AT 17:09
Okay but have you ever noticed how every time the government tries to 'protect seniors' they just add another pill to the mix? I'm telling you, Big Pharma owns the Beers Criteria. They wrote it themselves. That's why they keep pushing SSRIs and benzodiazepines-because they make more money off the side effects than the original condition. My aunt stopped all her meds and started drinking apple cider vinegar. She hasn't fallen since. Coincidence? I think not.
Donna Fleetwood
February 2, 2026 AT 15:42
This is so important. I just helped my mom go through her meds last month and we cut out three things-Benadryl, a sleeping pill, and a blood pressure med that was way too strong. Within two weeks, she was walking without her cane in the kitchen. It wasn't magic. It was just paying attention. You don't need to be a doctor to ask, 'Is this still helping?' I wish more people knew how powerful that question is.
Melissa Cogswell
February 4, 2026 AT 04:25
As a geriatric pharmacist, I see this every day. The biggest mistake? Assuming meds are permanent. I do HomeMeds reviews weekly. One woman was on 14 medications. We reduced her to 6. She went from needing help to stand to hiking with her grandkids. Deprescribing isn't about taking away care-it's about restoring function. The key is doing it slowly, with monitoring. And yes, OTC stuff like diphenhydramine is a silent killer. I tell patients: if it makes you sleepy, it's probably making you fall-prone too.
Diana Dougan
February 5, 2026 AT 08:39
Lmao so now we're blaming pills for old people falling? Next they'll say gravity is a conspiracy. My grandma was 92 and still walked 3 miles a day. She took exactly ZERO meds. Guess what? She didn't fall. Coincidence? Nah. It's called discipline. Everyone's so lazy they'd rather pop a pill than stand up straight or eat vegetables. And don't get me started on 'cognitive behavioral therapy'-sounds like a fancy way to say 'sit and think about your feelings'.
Bobbi Van Riet
February 5, 2026 AT 13:38
I just want to say how much this resonates. My dad was on five different meds for years-blood pressure, antidepressant, sleep aid, painkiller, and that sneaky Benadryl in his allergy pills. He started getting really clumsy, like he'd trip over nothing. We didn't connect it until his pharmacist said, 'You're basically giving him a sedative cocktail.' We tapered him off slowly over three months. The change was insane. He started remembering names again. He laughed more. He didn't just stop falling-he started living again. I wish someone had told us this sooner. Don't wait for a hospital visit. Just start the list. Even if you're scared. Just start.
Holly Robin
February 6, 2026 AT 01:32
THEY KNOW. THEY KNOW WHAT THEY'RE DOING. This isn't about safety-it's about CONTROL. Why do you think they push antidepressants on seniors? Because depressed people are easier to manage. Why benzodiazepines? Because they make you docile. Why antipsychotics for dementia? Because it's cheaper than hiring staff to actually talk to them. And don't think for a second that the FDA isn't in bed with the drug companies. The Beers Criteria? A distraction. They let you think you're safe while they keep prescribing. Wake up. Your meds are not your friends. They're your jailers.
Shubham Dixit
February 6, 2026 AT 18:06
In India, we don't have this problem because our elders don't take 12 pills a day. They take turmeric, ashwagandha, walk in the morning, and sit in the sun. Why do Americans think every problem needs a chemical solution? We treat aging like a disease. In our culture, elders are respected, not drugged. Your system is broken. You have specialists for everything but no one to look at the whole person. You need to go back to basics: food, movement, community. Not more prescriptions.
KATHRYN JOHNSON
February 8, 2026 AT 12:29
This article is dangerously misleading. Medications are not the primary cause of falls. Environmental hazards-loose rugs, poor lighting, lack of handrails-are far more significant. Blaming pharmaceuticals absolves caregivers and institutions of responsibility. The CDC data clearly shows environmental factors account for over 60% of falls. This narrative distracts from real solutions: home modifications, physical therapy, and proper supervision. Do not stop prescribed medications without medical oversight.
Sazzy De
February 9, 2026 AT 00:28
I just showed this to my mom. She's 78. She took one look at the list and said 'Oh. So that's why I feel like a zombie after lunch.' We're making an appointment next week. No drama. No panic. Just a list and a question: 'Can we try taking something off?'
Blair Kelly
February 9, 2026 AT 11:33
This is the most irresponsible article I've read all year. You're telling people to just stop their meds? Without supervision? That's not empowerment-that's malpractice. What happens when someone goes into withdrawal from an SSRI? Seizures. Suicidal ideation. Hallucinations. And you think they're just gonna 'get better'? This isn't wellness porn. This is a public health disaster waiting to happen. Someone should get sued for this.
Rohit Kumar
February 10, 2026 AT 02:41
The human body is not a machine to be optimized with pills. Aging is not a malfunction. It is a natural unfolding. Western medicine seeks to control, to suppress, to replace. But the body, when given space, rest, and dignity, finds its own balance. The Indian tradition speaks of 'prana'-life energy. When we flood the system with chemicals, we mute that inner rhythm. The fall is not just physical-it is spiritual. We must return to wisdom, not just science.
Lily Steele
February 10, 2026 AT 06:51
My grandma was on 8 meds. We cut 3. She started cooking again. She remembered my birthday. She didn't need to be 'fixed'. She just needed someone to listen. This isn't about being anti-med. It's about being pro-life.
Gaurav Meena
February 12, 2026 AT 04:31
I am a family physician in India and I see similar patterns. Many elderly patients come with 10+ prescriptions from multiple specialists. We use a simple approach: one doctor, one list, one conversation. We ask: 'What do you want to feel better at?' Not 'What's wrong with you?' Often, the answer is 'I want to walk to the temple without help.' Then we work backward. Sometimes that means stopping a pill. Sometimes it means adding a walk with a neighbor. Medicine should serve life-not the other way around.