Medication-Calcium Interaction Calculator
Calculate Safe Timing
Find out how long to wait between your medication and calcium-fortified drinks
Safe Waiting Time
You should wait at least before or after your medication.
Important: Calcium-fortified juices can reduce absorption of your medication by .
Why Timing Matters
Calcium binds tightly, making antibiotics ineffective
42% absorption reduction with calcium juice
35-55% absorption reduction
Calcium blocks absorption completely
Many people drink calcium-fortified orange juice to get more calcium, especially if they can’t drink milk. It’s marketed as a healthy alternative-same amount of calcium as a glass of milk, no lactose, and a tasty way to start the day. But here’s the problem: if you’re taking certain medications, that glass of juice could be making them useless.
Why Calcium-Fortified Juice Interferes with Medications
Calcium in these juices doesn’t just sit there. It actively binds to drugs in your stomach and intestines, forming big, insoluble clumps your body can’t absorb. This isn’t a myth or a rumor-it’s a well-documented chemical reaction backed by lab studies and real patient outcomes. When calcium ions meet drugs like ciprofloxacin or levothyroxine, they latch on tightly, creating complexes too large to pass through the gut lining. That means the medication doesn’t enter your bloodstream. It just passes through, unchanged and ineffective.The calcium concentration in these juices is high-typically 300 to 350 mg per 8-ounce serving. That’s enough to trigger a major interaction. The U.S. Pharmacopeia classifies this as a Class 1 food-drug interaction, meaning it’s serious enough to cause treatment failure. And it’s not just calcium alone. Calcium-fortified orange juice also contains citric acid, which changes the pH in your stomach. This double hit-calcium binding plus acidity-makes the problem worse. One study found that orange juice reduced ciprofloxacin absorption by 42%, while plain calcium water only cut it by 31%.
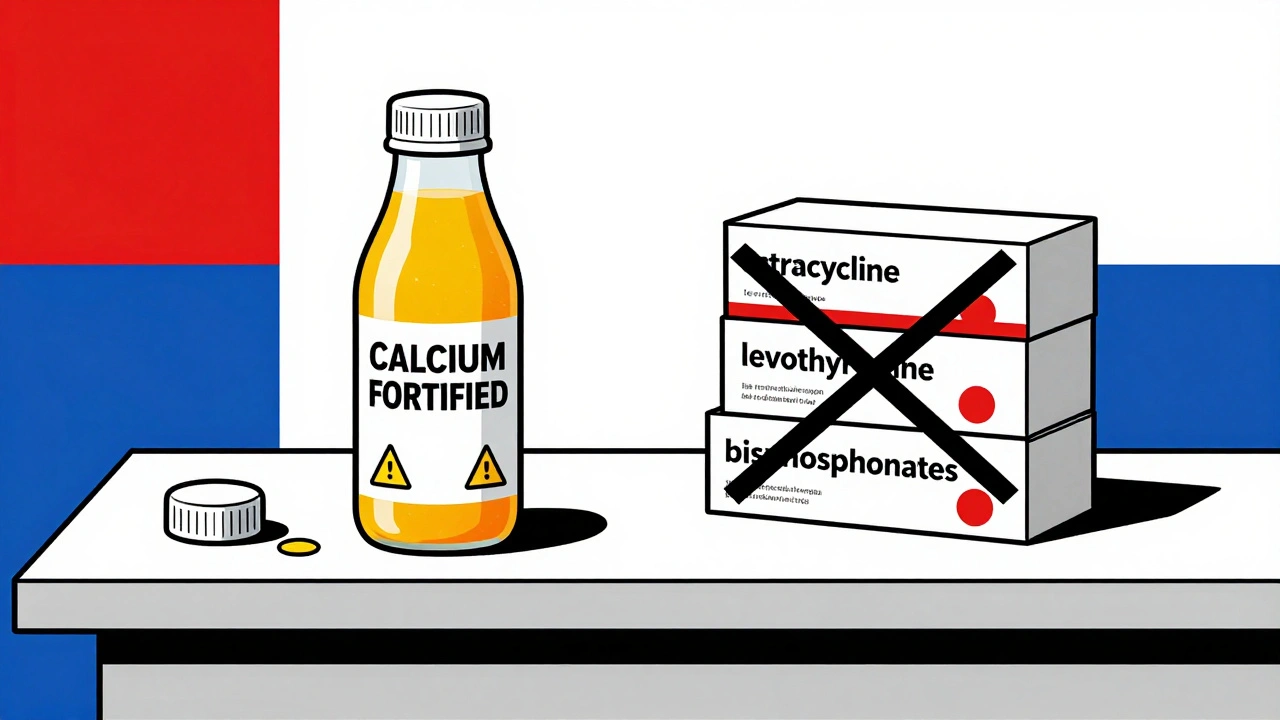
Medications That Are Affected
Not all medications are equally affected. But the ones that are? They’re critical. Here’s the short list of drugs you need to watch out for:- Tetracycline antibiotics (doxycycline, minocycline): Used for acne, Lyme disease, and respiratory infections. Calcium binds to these so tightly they become almost inactive.
- Fluoroquinolone antibiotics (ciprofloxacin, levofloxacin): Commonly prescribed for UTIs, sinus infections, and pneumonia. Taking them with calcium juice can lead to treatment failure. One study showed 25-30% of patients developed persistent infections when they drank calcium OJ with their pills.
- Bisphosphonates (alendronate, risedronate): Used to treat osteoporosis. These need an empty stomach and no calcium for 30 minutes to 2 hours after taking them. Calcium juice can block absorption completely.
- Levothyroxine: The main treatment for hypothyroidism. Calcium-fortified juice can reduce absorption by 35-55%. Patients often end up with sky-high TSH levels, meaning their thyroid isn’t working right-even if they’re taking the right dose.
- Ketoconazole: An antifungal used for serious fungal infections. Calcium reduces its absorption significantly, making it less effective.
These aren’t rare cases. A 2022 study of nearly 1,900 patients found that those who drank calcium-fortified juice with levothyroxine were more than twice as likely to have TSH levels outside the safe range. That’s not a small risk-it’s a major clinical issue.
How Long Should You Wait?
Timing matters. You can’t just take your pill and then drink juice an hour later. The waiting period depends on the drug:- Tetracyclines: Wait at least 2-3 hours before or after drinking calcium juice.
- Fluoroquinolones: Separate by 2-4 hours. Some experts recommend 4 hours to be safe.
- Bisphosphonates: Take on an empty stomach with plain water. Wait at least 30 minutes before eating or drinking anything else. Avoid calcium juice for at least 2 hours after.
- Levothyroxine: The American Thyroid Association recommends waiting 4 hours after taking the pill before consuming calcium-fortified products. Many patients take it first thing in the morning and don’t eat or drink anything except water for an hour. That’s fine-but if you’re drinking calcium juice, you need to wait until after lunch or dinner.
It’s not just about the juice. Other calcium sources like supplements, antacids, and even some cereals can cause the same problem. But fortified juices are especially tricky because they’re marketed as healthy, and people don’t think of them as “medicine disruptors.”

What Patients Are Saying
Real people are getting hurt because no one told them. On Reddit, a user wrote: “I drank two glasses of calcium OJ every morning with my doxycycline. My acne got worse. My doctor blamed stress.” Another on Drugs.com shared: “I took Synthroid for years. My TSH kept rising. I thought my dose was too low. Turns out, I was drinking calcium orange juice every day. Once I stopped, my levels normalized in 6 weeks.”Pharmacists are seeing this all the time. A 2023 survey of over 500 community pharmacists found that 73% regularly encounter patients taking calcium-fortified juice with medications that interact. But only 28% of those patients remembered being warned about it. That’s a huge gap.
Why Labels Don’t Warn You
You’d think the bottle would say “Do not take with medications.” But here’s the truth: 92% of calcium-fortified juice containers have no warning about drug interactions. The FDA requires drug labels to mention food interactions, but not the other way around. So the juice bottle tells you it has 30% of your daily calcium. It doesn’t say: “This will ruin your antibiotics or thyroid meds.”The FDA’s 2023 draft guidance calls for better labeling, but nothing’s changed yet. Meanwhile, the Institute for Safe Medication Practices added calcium-fortified beverages to its 2023 List of High-Alert Food-Drug Combinations. That means they’re now officially recognized as a serious risk.
What You Should Do
If you’re on any of the medications listed above:- Check your prescription. Look for warnings about calcium, dairy, or antacids.
- Ask your pharmacist. Don’t assume they’ll bring it up. Say: “I drink calcium-fortified orange juice. Is that safe with my meds?”
- Read the label. If it says “take on an empty stomach,” avoid all calcium-containing foods and drinks for the recommended time.
- Switch your morning drink. If you need calcium, get it from food-like broccoli, kale, or fortified tofu. Or take a calcium supplement at night, separate from your meds.
- Track your symptoms. If your infection isn’t clearing up, or your thyroid levels keep rising, ask if your diet could be the cause.
There’s no need to give up calcium-fortified juice forever. Just don’t take it with your meds. Separate them by hours, not minutes. And if you’re unsure, wait 4 hours. It’s better to be safe than to risk your treatment failing.
The Bigger Picture
This isn’t just about one juice. It’s about how we think about food and medicine. We assume if it’s healthy, it’s safe with everything. But calcium-fortified juice is a perfect example of how “healthy” doesn’t mean “harmless.”The cost of these interactions is real. A 2022 analysis estimated they cost the U.S. healthcare system $417 million a year in extra doctor visits, tests, hospital stays, and failed treatments. That’s money wasted because patients weren’t told.
There’s hope. Companies are working on new calcium forms that don’t bind to drugs. One patent from Nestlé describes “chelation-resistant calcium complexes.” And some pharmacies are testing QR codes on pill bottles that link to food interaction info. But until those become standard, the responsibility falls on you.
Know your meds. Know your juice. And if you’re not sure, ask. One conversation could save you from months of ineffective treatment.

Comments (12)
dan koz
December 3, 2025 AT 15:06
I drank calcium OJ with my doxycycline for months and my acne got worse. My doctor told me it was stress. Turns out, I was just poisoning my own treatment. Never again. This post saved me.
Mindy Bilotta
December 5, 2025 AT 10:20
OMG I just realized I’ve been drinking this juice with my levothyroxine for 3 years 😳 My TSH was always weird but I thought it was just ‘my body’. I switched to water and my levels normalized in 5 weeks. So simple. Why isn’t this on the bottle??
Brian Perry
December 6, 2025 AT 22:26
THIS IS A CONSPIRACY. The juice companies know this. They don’t warn you because they want you to fail so you go back to the doctor and get MORE meds. Big Pharma + Big Juice = your thyroid is toast. They’re making BILLIONS off this. I’m not taking my meds with anything but distilled water and a prayer now. 🙏
Chris Jahmil Ignacio
December 7, 2025 AT 22:38
People are idiots. You think just because it’s orange and has vitamin C it’s safe? No. You’re not special. Your ‘healthy’ habit is actively sabotaging your life. The FDA doesn’t regulate food labels for drug interactions because they don’t care about you. Your pharmacist doesn’t tell you because they’re overworked. You’re on your own. Stop being lazy and read the damn pamphlet. Or die.
Pamela Mae Ibabao
December 9, 2025 AT 14:18
Wait so if I take my bisphosphonate at 7am and drink my calcium OJ at 11am… is that okay? I’ve been doing that for years. I’m so scared now 😅
Palanivelu Sivanathan
December 10, 2025 AT 07:58
Life is a paradox, isn’t it? We seek health through fortification, yet we poison ourselves with the very thing meant to heal. Calcium, the mineral of bones, becomes the thief of absorption. The juice, a symbol of vitality, becomes the silent assassin. We are children playing with fire, calling it sunshine. The body remembers. The body always remembers.
Erik van Hees
December 10, 2025 AT 17:06
Actually there’s a newer study from Mayo Clinic in 2024 showing that calcium citrate in juice binds less than calcium carbonate in supplements. So if you’re gonna drink it, pick the kind with citrate. Also, timing matters more than you think - 4 hours is ideal but 2 hours with plain water before and after can work if you’re desperate. Don’t panic, just optimize.
Cristy Magdalena
December 12, 2025 AT 15:46
I cried reading this. I took Synthroid with OJ for 8 years. My hair fell out. I gained 40 pounds. My husband left me. I thought I was broken. Turns out I was just drinking poison every morning. I stopped 6 months ago. I’m finally me again. Thank you for writing this. I needed to know I wasn’t crazy.
May .
December 14, 2025 AT 09:47
So… can I just take my pill at night instead?
Sara Larson
December 15, 2025 AT 01:08
YES!! 💪 I started taking my levothyroxine at bedtime with water and it changed my life! No more morning rush, no juice conflicts, and my energy is UP! 🌞☕️ You got this!!
Josh Bilskemper
December 15, 2025 AT 12:20
If you’re taking levothyroxine and drinking fortified juice you’re not just irresponsible you’re intellectually deficient. The science has been known since the 90s. If you didn’t know this you shouldn’t be allowed to manage your own medication. Get a pharmacist. Or a brain.
Storz Vonderheide
December 16, 2025 AT 11:34
Just want to say thank you for posting this. I’m from Nigeria and we don’t have much access to good healthcare info here. I shared this with my cousin who’s on doxycycline and she’s already switched to almond milk. We’re all learning together. Knowledge is power, and you just gave us a flashlight in the dark. 🙏