Most people don’t realize how much they’re missing until their hearing starts slipping away. You keep asking people to repeat themselves. The TV volume is always too loud. Conversations in crowded rooms feel like a puzzle you can’t solve. These aren’t just signs of aging-they’re red flags that your hearing needs a proper checkup. That’s where audiometry testing comes in. It’s not a simple ear check. It’s a precise, science-backed way to measure exactly how well you hear-and what’s going wrong inside your ears.
What Audiometry Testing Actually Measures
Audiometry testing doesn’t just ask, “Can you hear me?” It answers: What’s the quietest sound you can detect at each pitch? This is measured in decibels hearing level (dB HL), a standardized scale where 0 dB HL represents the softest sound a healthy young adult can hear. If you can’t hear a tone until it’s at 30 dB HL, that’s a hearing loss of 30 dB at that frequency.
The test covers a range of frequencies-from 250 Hz (low rumbles) to 8,000 Hz (high-pitched birds or birdsong). These aren’t random numbers. They match the range of human speech. If you struggle with high frequencies, you might hear someone talking but miss words like “s,” “t,” or “th.” That’s why people say, “I can hear you, but I can’t understand you.”
The test uses two methods: air conduction and bone conduction. Air conduction sends sound through earphones, testing your entire hearing pathway-from outer ear to inner ear. Bone conduction bypasses the outer and middle ear by placing a small vibrator on your mastoid bone (behind the ear) or forehead. It sends vibrations straight to the cochlea. If air conduction shows worse hearing than bone conduction, that’s a clear sign of a conductive issue-like earwax buildup, fluid behind the eardrum, or a damaged ossicle.
The Hughson-Westlake Method: How Thresholds Are Found
There’s a reason audiometry is trusted by doctors worldwide. It follows a strict, repeatable method called the modified Hughson-Westlake technique. It’s not guesswork. It’s a step-by-step process designed to find your exact hearing threshold-the quietest sound you can detect half the time.
Here’s how it works: The audiologist starts at a frequency you can easily hear-usually 1,000 Hz-and plays a tone at 40 dB HL. If you respond, they drop the volume by 10 dB. If you don’t hear it, they increase it by 5 dB. They keep going up and down until they find the point where you hear it 50% of the time. That’s your threshold. They repeat this for each frequency, building a map of your hearing.
This method is precise because it accounts for human error. You might miss a tone because you were distracted, or you might press the button too soon. By using the “down 10, up 5” pattern, the test confirms your real threshold-not a lucky guess.
What Your Audiogram Tells You
The results of your test are shown on an audiogram-a graph that plots frequency on the horizontal axis and loudness (in dB) on the vertical axis. Lower numbers mean better hearing. Higher numbers mean more hearing loss.
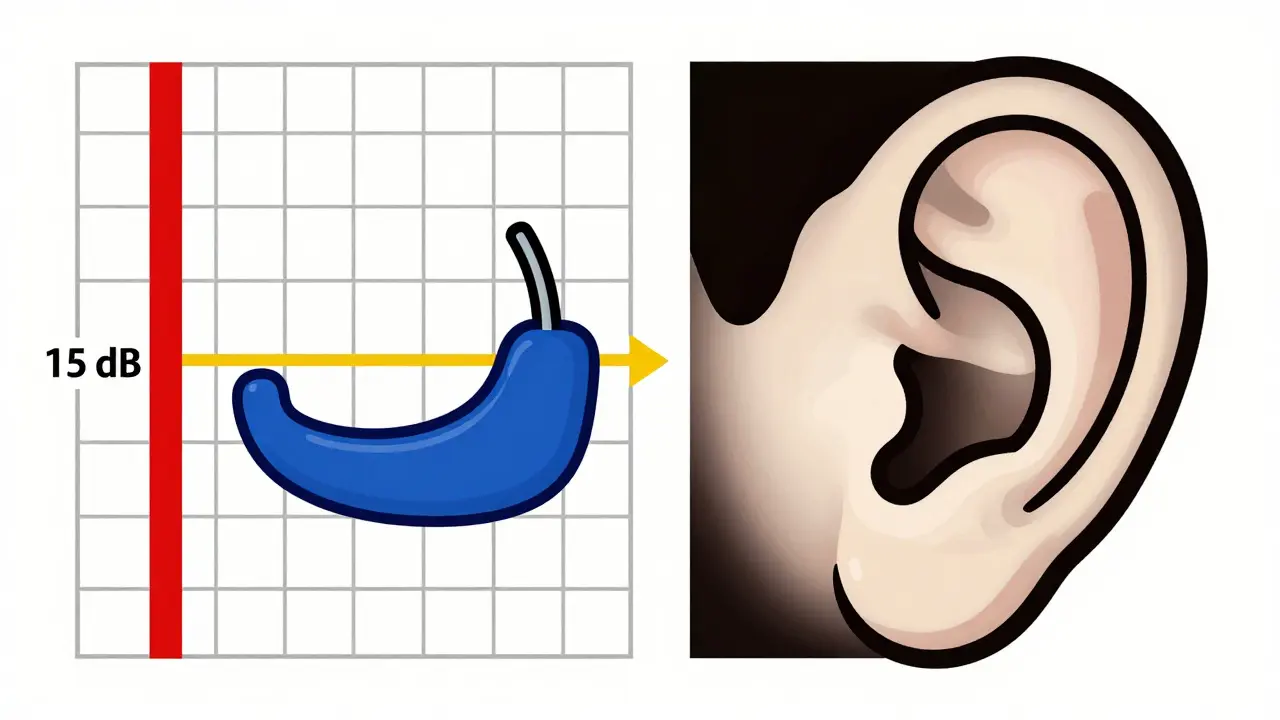
Standard symbols are used: circles (○) for your right ear’s air conduction, X’s (X) for your left ear’s air conduction. Bone conduction is marked with brackets ([ ]) for the right ear and angled brackets (<) for the left. If you see a gap between the air and bone lines, that’s an air-bone gap. A gap of 15 dB or more means conductive hearing loss. If both lines are low and close together, it’s sensorineural hearing loss-damage to the inner ear or nerve.
Doctors classify hearing loss by degree:
- Normal: 0-25 dB HL
- Mild: 26-40 dB HL
- Moderate: 41-55 dB HL
- Moderately severe: 56-70 dB HL
- Severe: 71-90 dB HL
- Profound: 91+ dB HL
If your audiogram shows a 45 dB loss at 2,000 Hz, you’re in the moderate range. You’ll struggle with speech clarity, especially in noise. This is why hearing aids are often recommended at this stage-not to restore perfect hearing, but to make conversation possible again.
Speech Testing: Why Hearing Isn’t Just About Volume
Audiometry doesn’t stop at tones. A key part of the test is speech audiometry. This includes two parts: the speech reception threshold (SRT) and word recognition.
SRT measures the softest level at which you can repeat 50% of two-syllable words like “baseball” or “hotdog.” Your SRT should match your average pure-tone threshold at 500, 1,000, and 2,000 Hz-within 10 dB. If it doesn’t, something’s off. Maybe the test was inaccurate, or maybe there’s a neurological issue.
Word recognition testing asks you to repeat single-syllable words like “cat,” “pin,” or “ship” at a volume 25-40 dB above your threshold. A healthy ear should score 90% or higher. If you only get 60%, you have poor speech discrimination. This is common with age-related hearing loss or nerve damage. It means your ears hear the sound, but your brain can’t process the words clearly. Hearing aids can help with volume, but they won’t fix this. You might need auditory training or cochlear implants.
Tympanometry and ABR: The Hidden Pieces
A full hearing assessment isn’t just about what you hear. It’s about what’s blocking the sound. That’s where typanometry comes in. A small probe is placed in your ear canal, and air pressure changes while a tone plays. It measures how well your eardrum moves. A flat line (Type B) means fluid is behind the eardrum-common in ear infections or allergies. A peak in the wrong place might mean a stiff joint in the middle ear.
For babies, toddlers, or people who can’t respond reliably, doctors use auditory brainstem response (ABR). Electrodes on your scalp detect tiny electrical signals from your auditory nerve when sound plays. It doesn’t require you to press a button. It’s how newborns are screened before leaving the hospital. The CDC requires all U.S. babies to get this screening before one month old. If they fail, they get a full diagnostic test by three months. Early intervention can prevent lifelong speech delays.
Who Needs Audiometry Testing?
You don’t have to be old to need this test. Here’s who should get one:
- Anyone over 50-age-related hearing loss affects half of people over 75
- People exposed to loud noise-construction workers, musicians, factory staff
- Those with ringing in the ears (tinnitus) or dizziness
- People with a family history of hearing loss
- Anyone who says, “I hear fine, I just don’t understand what people are saying”
- Children who don’t respond to their name or seem to ignore speech
Occupational safety rules require annual hearing tests for workers in noisy environments. The OSHA standards are strict because noise-induced hearing loss is permanent and preventable.
What to Expect During the Test
The whole process takes 20-45 minutes. You’ll sit in a soundproof booth, wear earphones, and press a button every time you hear a tone. You’ll listen to words, feel a vibration behind your ear, and have a tiny probe inserted into your ear canal. It’s not painful. It’s quiet. You might feel a little odd with the bone oscillator on your head, especially if you wear glasses.
Some people get frustrated because they don’t hear every tone. That’s normal. The test is designed to find your limit-not your best performance. If you miss a few, the audiologist will adjust. The goal isn’t perfection. It’s accuracy.
Common Misconceptions
Many think hearing loss is just about volume. It’s not. It’s about clarity. You might hear your wife’s voice but miss the word “not” in “I didn’t say that.” That’s a high-frequency loss. You might hear the TV but not the doorbell. That’s a low-frequency issue.
Another myth: “I’ll know when I need hearing aids.” No, you won’t. Hearing loss creeps in slowly. Your brain adapts. You start avoiding conversations. You stop going to family dinners. By the time you notice, you’ve lost years of connection.
And no, over-the-counter hearing aids aren’t a substitute for a full audiometry test. Without knowing your exact thresholds and speech discrimination, you might buy a device that amplifies the wrong frequencies-or makes background noise louder than speech.
What Happens After the Test?
A good audiologist doesn’t just hand you a chart and say, “You have a loss.” They explain what it means. They show you your audiogram. They tell you if it’s noise-induced, age-related, or due to something treatable-like earwax or an infection. They’ll discuss options: hearing aids, assistive devices, or referrals to an ENT if surgery might help.
For most people, hearing aids are the next step. Modern ones can connect to your phone, reduce background noise, and even adjust automatically when you walk into a noisy room. But they only work if they’re programmed to your exact hearing profile. That’s why the audiogram matters.
And if you’re a parent? If your child failed a school screening, don’t wait. Get a full diagnostic test. Early intervention with hearing aids or cochlear implants can change a child’s entire future.
Why This Test Can’t Be Skipped
Hearing loss isn’t just about missing the news or music. It’s linked to dementia, depression, social isolation, and falls. The brain works harder to understand speech when hearing is poor. That mental strain drains energy and accelerates cognitive decline. Studies show people with untreated hearing loss are 24% more likely to develop dementia.
Audiometry testing is the first step to taking control. It’s not scary. It’s not expensive. Most insurance plans cover it. And it’s the only way to know exactly what’s going on inside your ears.
If you’ve been avoiding this test because you think it’s “just part of getting older,” think again. Your hearing is part of your quality of life. And it’s not too late to fix it-if you know what’s wrong.
Is audiometry testing painful?
No, audiometry testing is completely painless. You’ll wear earphones, hear tones, and press a button when you hear them. Bone conduction involves a small vibrator behind your ear, which might feel odd or slightly uncomfortable if you wear glasses, but it doesn’t hurt. Tympanometry feels like a gentle pressure change in your ear. There’s no needles, no probes inside your ear canal beyond a small, soft tip.
How long does an audiometry test take?
A full diagnostic test usually takes 20 to 45 minutes. Screening tests, like those at pharmacies or schools, take only 2-5 minutes but don’t give detailed results. A full assessment includes pure-tone testing, speech testing, and tympanometry. If you’re getting ABR testing for a child, it may take longer-up to an hour-because it’s done while they sleep or rest.
Can I do audiometry testing at home?
Some apps and online tools claim to test your hearing, but they’re not reliable. Background noise, poor headphones, and uncalibrated speakers make results inaccurate. The FDA allows remote audiometry using certified equipment like the KUDUwave booth, but even those require professional oversight. For accurate diagnosis, especially if you’re considering hearing aids, a clinical test with a licensed audiologist is necessary.
What does 25 dB HL mean on an audiogram?
25 dB HL is the upper limit of normal hearing. If your thresholds are at or below 25 dB across all frequencies, your hearing is considered normal. If you need a tone to be 30 dB or louder before you hear it, that’s a mild hearing loss. The zero point on the audiogram isn’t silence-it’s the average hearing level of healthy young adults. Anything above 25 dB means you need more volume to hear the same sound.
Do I need a referral to get an audiometry test?
In most cases, no. You can schedule a hearing test directly with an audiologist without a doctor’s referral. Many insurance plans, including Medicare Advantage, cover annual hearing evaluations. If you’re part of a workplace hearing conservation program, your employer may arrange testing. If you’re unsure, call a local audiology clinic-they’ll tell you what you need.
Can audiometry detect tinnitus?
Audiometry doesn’t directly measure tinnitus-the ringing or buzzing in your ears-but it helps identify its cause. Most people with tinnitus also have hearing loss, especially in high frequencies. The audiogram can show if your hearing loss matches the pitch of your tinnitus. It also rules out other conditions like ear infections or tumors that might be causing it. Treating the underlying hearing loss often reduces tinnitus symptoms.
Why do I need both air and bone conduction tests?
Air conduction tests your entire hearing system-from ear canal to brain. Bone conduction skips the outer and middle ear and tests only the inner ear and nerve. If air conduction is worse than bone conduction, there’s a blockage in the outer or middle ear (like wax, fluid, or a broken bone). If both are equally poor, the problem is in the inner ear or nerve. This distinction is critical for deciding whether you need surgery, medication, or hearing aids.

Comments (14)
Trevor Davis
January 15, 2026 AT 00:49
I used to think my hearing was fine until I missed my kid saying 'I love you' three times in a row. Turns out, I had a mild high-frequency loss. Got tested last year-best decision ever. Now I hear birds again. Weird how something so quiet can change everything.
Also, hearing aids aren't ugly anymore. Mine look like AirPods. My wife says I look 'techy.' I say I look like I'm not missing out on life.
John Tran
January 15, 2026 AT 07:31
Listen, man. Hearing loss isn't just a medical issue-it's a metaphysical one. We live in a world saturated with noise, yet we're starved for true sound. The audiogram? It's not just a graph-it's a soul-map. Every dB HL is a silent scream from your inner ear begging to be heard. And yet society tells us to just turn up the TV. We've forgotten what silence sounds like. We've forgotten what connection feels like. When you finally hear your own heartbeat through bone conduction... you realize you've been living in a muted dream. The real tragedy? Most people never even wake up.
Also, I once heard a moth flap its wings at 12,000 Hz. That's the sound of the universe whispering. You can't get that from a hearing aid. You can only get it when you stop trying to hear and start listening.
mike swinchoski
January 15, 2026 AT 12:31
Why do people even bother with all this fancy testing? Just go to the store, buy a $50 hearing aid, and be done with it. You think you need a PhD to hear your grandkids? Nah. You just need to stop being lazy. I’ve been wearing mine for two years. I hear everything. Even my neighbor’s dog barking at 3 a.m. You don’t need a chart. You need to care.
And stop calling it ‘hearing loss.’ It’s just volume control. Like your TV remote. You wouldn’t blame the TV for being too quiet-you’d just turn it up.
Gregory Parschauer
January 16, 2026 AT 16:36
Let me cut through the corporate audiologist BS. You think they care about your hearing? No. They care about selling you $3,000 devices with Bluetooth and AI noise-canceling that you’ll never use. The real issue? Noise pollution. Cities are killing our ears. Factories. Traffic. Airplanes. Phones. We’ve turned our auditory cortex into a spam filter. Audiometry doesn’t fix that. It just quantifies the damage.
And don’t get me started on OSHA. They force workers to get tested so they can say they ‘complied’ while still letting factories run at 90 dB. It’s not healthcare-it’s liability management. Your hearing is a commodity. And they’re pricing it at $2,999 per ear.
Real solution? Silence. Go sit in a forest. For an hour. No headphones. No apps. Just you and the wind. That’s the only audiometry that matters.
Trevor Whipple
January 17, 2026 AT 02:01
Wait so if I hear a tone at 30 dB but my friend hears it at 25, does that mean he’s better than me? Like, is my hearing score a reflection of my worth? I feel like I’m being graded on my ears now. Also, I think I have a 20 dB loss but I just ignore it. My dog hears better than me anyway. He barks at the microwave. I just stare at it.
Also, bone conduction? That’s just a fancy way of saying ‘vibrate your skull.’ I tried it once with my phone on my forehead. Got a headache. And my neighbor called the cops. Not worth it.
Milla Masliy
January 17, 2026 AT 21:02
My mom got tested after she kept asking if the cat was meowing or the fridge humming. Turns out, she had a 40 dB loss. Got hearing aids, now she’s the loudest person at family dinners. ‘I HEAR YOU, DARLING!’ she yells across the table. I miss the quiet.
But honestly? The audiogram made her feel seen. Like someone finally understood why she kept missing the punchlines. So I get it. It’s not just about volume. It’s about belonging. Even if now she yells at the TV like she’s leading a rally.
Clay .Haeber
January 18, 2026 AT 19:21
Oh wow, another article about how ‘hearing loss is silent’ and ‘you don’t know you’re losing it.’ Newsflash: we all know. We just don’t care. I’ve been saying ‘what?’ for 12 years. I just nod and laugh. It’s easier than admitting I can’t hear the difference between ‘cat’ and ‘cap.’
And yes, I’ve bought three ‘budget’ hearing aids off Amazon. Two broke. One made my voice sound like a robot on helium. I’m just waiting for the AI to start whispering my thoughts back to me. That’ll be the next upgrade.
Avneet Singh
January 20, 2026 AT 08:54
As a professional in audiological diagnostics, I must point out the fundamental flaw in the Hughson-Westlake method: it assumes perfect subject compliance and cognitive consistency. In reality, attentional drift, fatigue, and cognitive load drastically skew thresholds, especially in elderly populations. The 50% criterion is statistically arbitrary and lacks ecological validity. Modern approaches using adaptive psychophysics or machine learning-based threshold estimation are far superior-yet still underutilized in clinical settings due to cost and training barriers.
Also, tympanometry is not a ‘probe.’ It’s a pressure-based impedance analyzer. Terminology matters.
Lance Nickie
January 20, 2026 AT 13:14
Got tested. 35 dB loss. Bought hearing aids. Still can’t hear my wife when she says ‘we need to talk.’
Worth it.
Damario Brown
January 20, 2026 AT 16:14
Let’s be real-this whole thing is a scam. You think your audiogram means something? It’s just a number. Your brain fills in the gaps. That’s why you think you’re hearing fine. You’re not. You’re just good at guessing. And those hearing aids? They don’t fix your brain. They just make the noise louder. You’re still missing the meaning.
And the CDC? They push newborn screening because they want to lock kids into the system early. You think that’s for their benefit? It’s for the industry’s profit margin. 91+ dB HL? That’s not hearing loss. That’s capitalism.
sam abas
January 21, 2026 AT 16:08
I read the whole thing. Twice. Then I went back and re-read the part about bone conduction. I think I understand it now. But I’m still confused why they use brackets and angled brackets. Why not just use different colors? Or emojis? 🟢 for right ear, 🔵 for left? Why the math symbols? It feels like they’re trying to impress us with their PhDs instead of helping us.
Also, I’m 32. I don’t need this test. I’m fine. I just need my wife to stop talking so fast. And turn down the TV. And not whisper when she’s mad. And not say ‘I said’ like 12 times. But that’s not a hearing issue. That’s a marriage issue.
Still. I’m gonna book the appointment. Just to prove I’m not the problem.
John Pope
January 22, 2026 AT 15:37
Here’s the truth no one says: hearing loss isn’t about decibels. It’s about grief. You don’t lose the sound-you lose the moments. The laugh your dad used to have when he told that one joke. The way your mom hummed off-key in the kitchen. The quiet rustle of your kid falling asleep.
That’s the real audiogram. The one with the silent peaks. The ones where you didn’t press the button because you were too busy pretending you heard.
And when you finally get tested? You don’t just get a number. You get a mirror. And it’s ugly. Because you realize you’ve been avoiding the truth for years.
So yeah. Go get tested. But don’t be surprised when the test doesn’t just measure your ears-it measures your courage.
Priyanka Kumari
January 24, 2026 AT 09:29
As someone who grew up in a household where hearing loss ran in the family, I’m so glad this post exists. My grandmother waited until she couldn’t hear her own grandchildren say ‘I love you’ before she got help. Don’t wait. Get tested. It’s not about age-it’s about connection.
And if you’re worried about hearing aids? Talk to someone who’s worn them for years. They’ll tell you it’s like putting on glasses for the first time. Everything comes alive. The birds. The rain. The quiet sigh of someone you love falling asleep next to you.
You don’t need to be brave. You just need to be ready to listen again.
Adam Vella
January 25, 2026 AT 02:30
While the article provides a comprehensive overview of audiometric procedures, it fails to address the critical limitation of pure-tone audiometry in differentiating between cochlear and retrocochlear pathologies without additional electrophysiological testing. Furthermore, the reliance on subjective responses introduces significant variability, particularly in populations with cognitive impairments or language barriers. The article's omission of the role of otoacoustic emissions (OAEs) as a non-invasive screening tool for outer hair cell function represents a notable gap in clinical context.
Additionally, the classification of hearing loss by degree is overly simplistic and does not account for the psychoacoustic impact of slope configuration-e.g., a steeply sloping high-frequency loss has a far greater communicative impact than a flat loss of equal average dB HL.
While well-intentioned, this piece reads more like a marketing brochure for hearing aid manufacturers than a rigorous clinical primer.