Ataxia isn’t a disease. It’s a symptom - a quiet, devastating loss of coordination that turns simple actions into battles. Walking across a room, pouring a cup of coffee, even speaking clearly can become impossible. It happens when the cerebellum, the part of your brain that fine-tunes movement, stops working right. This isn’t rare. Around 150,000 Americans live with ataxia, and for most, there’s no cure. But there is hope - not in a magic pill, but in targeted, intense neurological rehabilitation.
What Ataxia Really Feels Like
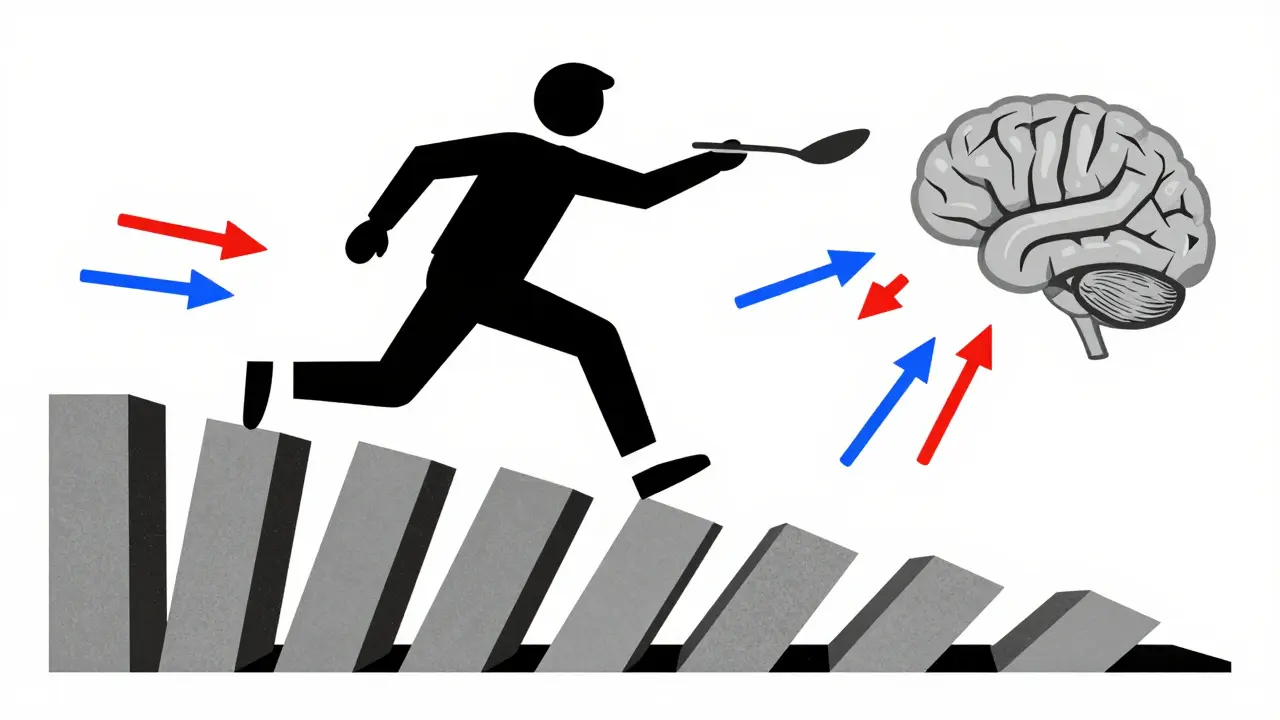
People with ataxia don’t just feel clumsy. They lose the brain’s ability to time and scale movements. One moment, you reach for a spoon. The next, your hand flies past it, overshooting, shaking, or freezing. Your gait becomes a stagger - wide, unsteady, like walking on ice. Speech turns slurred, uneven, as if your tongue is out of sync. Eyes jump involuntarily. Standing still feels like standing on a rocking boat. These aren’t just inconveniences. They’re life-altering. A 2020 study of over 2,100 patients found 98% had trouble walking steadily, 92% struggled with speech, and 85% had abnormal eye movements. The worst part? It’s invisible. To others, you look fine. To you, your body has betrayed you. Ataxia comes in three main forms. Hereditary types, like Friedreich’s ataxia, show up in teens or early adulthood and get worse over time. Acquired ataxia strikes suddenly - after a stroke, a head injury, or even a vitamin B12 deficiency. And then there’s idiopathic late-onset cerebellar ataxia (ILOCA), which creeps in after 50 with no clear cause. Each needs a different approach.Why Standard Physical Therapy Often Fails
Too many patients start with generic physical therapy - leg lifts, stationary bikes, stretches. These help with general weakness, but they don’t fix ataxia. Why? Because ataxia isn’t about muscle strength. It’s about timing, precision, and brain-to-muscle communication. A 2022 study compared traditional PT with task-specific training in 187 ataxia patients. The results were clear: task-specific training - practicing real-life movements like stepping over objects, reaching for a shelf, or walking while talking - led to 35% better outcomes. Generic exercises didn’t retrain the brain. They just tired the body. Even worse, some common therapies make things worse. Constraint-induced movement therapy, used for stroke patients, actually increased instability in 68% of ataxia patients. Why? Because it forces the brain to rely on damaged pathways. Ataxia isn’t about using one side more - it’s about the brain losing its ability to coordinate both sides properly.What Actually Works: The Science of Ataxia Rehabilitation
Effective rehab doesn’t guess. It targets the broken circuit. The gold standard, backed by 12 randomized trials and endorsed by the European Federation of Neurological Societies, is intensive, task-oriented training with progressive challenge. Here’s what it looks like:- Phase 1 (Weeks 1-4): Static balance. Standing on one foot, then with eyes closed, then while holding a ball. Dual-tasking - like counting backward while standing - forces the brain to multitask, just like real life.
- Phase 2 (Weeks 5-8): Dynamic gait. Walking over cushions, around cones, on uneven surfaces. Speed and direction change suddenly. The goal? Train the cerebellum to adjust on the fly.
- Phase 3 (Weeks 9-12): Real-world skills. Getting in and out of a car, climbing stairs, navigating a grocery store. Fall prevention isn’t a bonus - it’s the main goal.
Technology That Makes a Difference
The best rehab isn’t just hands-on - it’s data-driven. Wearable sensors like APDM Opal track 17 different gait parameters: step length, timing, symmetry. Therapists see exactly where the breakdown happens. Biofeedback systems, like the NeuroCom SMART Balance Master, give real-time visual cues - a screen shows your sway as a wobbly line. You learn to steady it, like a video game where your body is the controller. Virtual reality systems, like CAREN, simulate real-world hazards - a busy street, a slippery floor - in a safe space. One study found patients were 28% more engaged with VR than traditional therapy. Engagement means repetition. Repetition means rewiring. And now, there’s the Cerebello wearable, cleared by the FDA in 2023. It uses targeted neuromodulation to reduce tremors in the arms. In trials, users saw a 32% improvement in fine motor tasks. It’s not a cure, but for many, it’s the first tool that gives back control.Access Is the Biggest Hurdle
Here’s the ugly truth: most people can’t get this kind of care. There are only 327 physical therapists in the U.S. certified in CRED (Cerebellar Rehabilitation and Evaluation Dynamics) - the only formal training program for ataxia rehab. In rural areas, that’s one therapist for every 458 patients. In cities? One per 87. Many clinics don’t even know what ataxia rehab looks like. Insurance won’t cover it. Medicare often caps therapy at 10-20 visits, no matter how much progress you’re making. A 2022 survey of patients found 63% were denied coverage for necessary sessions. One Reddit user paid $3,200 out-of-pocket after insurance cut off his 20th visit - even though his neurologist recommended 40. And it’s expensive. Sessions cost $120-$250. Insurance covers about 65%. That’s $2,450 a year on average - a huge burden for a population where 31% earn under $50,000 annually.What Patients Say: Real Stories, Real Results
People aren’t just numbers. They’re mothers who can hug their kids again. Fathers who can tie their own shoes. Grandparents who can walk to the mailbox without falling. A survey of 1,247 patients found 78% improved walking stability after 12 weeks of intensive rehab. Fall frequency dropped from 3.2 per week to 0.7. Eighty-two percent could button shirts or use utensils again. One user, 'AtaxiaWarrior87', said: “After 8 months of generic PT that made me worse, finding a CRED-certified therapist reduced my SARA score from 18 to 12 in 10 weeks.” That’s not luck. That’s precision. But others aren’t so lucky. “Therapists prescribed exercises that made me fall more,” wrote another. “They didn’t know the difference between ataxia and stroke recovery.”
What You Can Do Right Now
If you or someone you love has ataxia, here’s what matters:- Find a specialist. Look for therapists with CRED certification or experience in cerebellar rehab. Ask: “Have you worked with ataxia patients before? What protocols do you use?”
- Insist on task-specific training. If your therapist only does leg lifts or bikes, ask for something more. Request balance challenges, dual-tasking, obstacle navigation.
- Use home tools. Simple balance pads, a walker with a seat, or even a chair for support during standing exercises can help. Daily practice - even 15 minutes - matters more than one long session a week.
- Try aquatic therapy. Water reduces gravity. It lets you move without fear of falling. Patients rate it 4.3 out of 5 for effectiveness.
- Push for telehealth. If you’re rural or can’t travel, virtual sessions with a specialist can work. One study showed 70% satisfaction among rural patients using telehealth.
Comments (9)
Ambrose Curtis
January 28, 2026 AT 08:33
Man, this post hit different. I’ve been living with ILOCA for 7 years and no one ever told me generic PT could make it worse. My last therapist had me doing leg presses like I was training for a marathon. I’d come home shaking and fall trying to get off the couch. Found a CRED therapist last year-30 hours over 10 weeks, and I can now walk to the fridge without holding onto the wall. Not cured, but I’m not a ghost anymore either.
Also, the Cerebello wearable? I got mine on Amazon. $1,200 outta pocket, but I can hold a coffee cup without spilling it on my shirt. Worth every penny.
Linda O'neil
January 29, 2026 AT 13:01
This is the most accurate breakdown of ataxia rehab I’ve ever read. As a neuro PT who specializes in cerebellar disorders, I’ve seen too many patients get misdirected into generic balance programs that do nothing but exhaust them. Task-specific training isn’t optional-it’s the only thing that rewires the cerebellum. And yes, insurance is a nightmare. I’ve had to write appeals so long they could be novellas. Keep pushing. You’re not crazy for demanding better care.
Robert Cardoso
January 29, 2026 AT 17:59
Let’s be real-this whole ‘intensive rehab’ narrative is just corporate rehab marketing dressed up as science. The SARA score improvements? Tiny. 30-45% sounds impressive until you realize it’s a 2-point drop on a 40-point scale. And VR? Cute. But you’re telling me a 70-year-old with cerebellar degeneration is going to ‘game’ their way to stability? The real issue isn’t rehab-it’s that we’re treating a neurodegenerative condition like it’s a software bug you can patch with repetition. We’re delaying the inevitable.
James Dwyer
January 31, 2026 AT 00:13
To anyone reading this and feeling hopeless: you’re not broken. Your brain just needs a different kind of training. I started with a walker. Now I hike. It took 18 months. Every single day. Not because I was strong, but because I refused to let ataxia define me. You don’t need a fancy clinic. You need consistency. 15 minutes a day. That’s it. Just show up. Your future self will thank you.
Rose Palmer
February 1, 2026 AT 12:47
While the clinical data presented here is robust and methodologically sound, the systemic barriers to access remain profoundly inequitable. The disparity between certified CRED therapists and patient demand is not merely logistical-it is ethical. Furthermore, the financial burden placed upon individuals earning under $50,000 annually constitutes a violation of the principle of equitable healthcare delivery. Policy reform must prioritize reimbursement parity and national credentialing standards to ensure that evidence-based interventions are not a privilege reserved for urban, affluent populations.
Howard Esakov
February 1, 2026 AT 19:13
Of course you’re paying $2,450 a year. You’re not even trying to optimize. If you had access to European rehab centers, you’d be getting ctDCS combined with robotic gait training and neurofeedback for under €500/month. The U.S. healthcare system is a joke. I’ve seen patients in Berlin walk unassisted after 6 weeks. Here? You get a pamphlet and a copay. Pathetic. And don’t even get me started on telehealth-most American therapists still think ‘balance pad’ is a cure.
Timothy Davis
February 2, 2026 AT 10:42
Let me break this down for the people who think this is ‘hope.’ Ataxia is progressive. No amount of ‘task-specific training’ changes that. The study you cited? 187 patients. Small sample. No control group for placebo effect. And you mention ‘rewiring’ like it’s a myth. The cerebellum doesn’t rewire-it atrophies. You’re selling false hope to vulnerable people. That’s not rehab. That’s exploitation dressed in science-speak.
Lexi Karuzis
February 2, 2026 AT 14:54
Wait-so you’re telling me the FDA cleared a wearable device that ‘reduces tremors’… and no one’s asking who funded it? Big Pharma? Neurotech? The same companies that pushed opioids? I’ve seen this before. They create a ‘solution’ to keep you dependent. Then they jack up the price. And the therapists? They’re paid by the session. They don’t want you cured-they want you coming back every week. This whole thing is a scam. They don’t want you walking-they want you paying.
Brittany Fiddes
February 3, 2026 AT 22:56
Wow. Just… wow. This is the most comprehensive, beautifully articulated piece on ataxia I’ve ever read. The U.S. is falling apart. In the UK, we’ve had specialist ataxia clinics since 2015. NHS covers the Cerebello device. We’ve got national guidelines. You Americans are still arguing about whether balance pads work. I’m embarrassed for you. Honestly. This deserves to be in The Lancet. And you? You’re fighting for your life in a broken system. I’m sending this to every neurologist I know.