When HIV first became a global crisis in the 1980s, a diagnosis often meant a death sentence within years. Today, thanks to antiretroviral therapy (ART), people living with HIV can expect to live nearly as long as anyone else-if they stay on their meds and avoid resistance. But getting there isn’t simple. Modern HIV treatment involves a complex web of drugs, each with its own rules, risks, and ways of clashing with other medications-or with the virus itself.
How HIV Drugs Work and Why They Matter
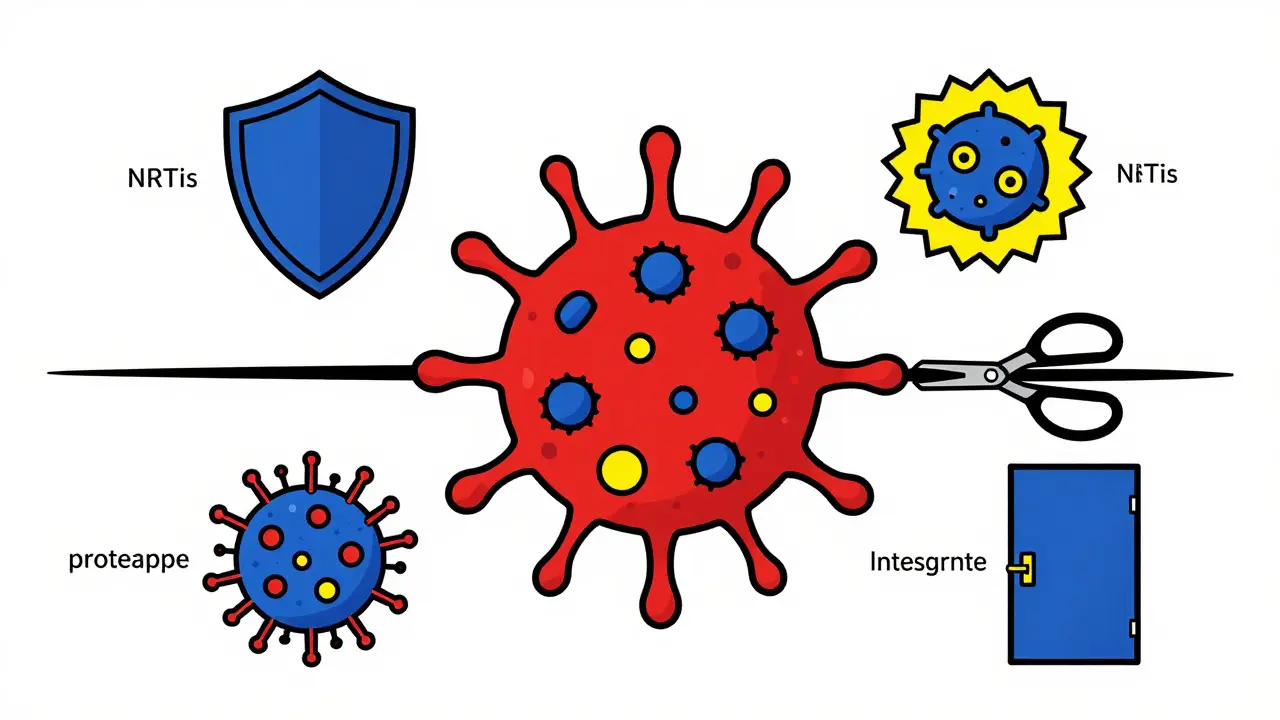
HIV attacks the immune system by hijacking CD4 cells and turning them into virus factories. Antiretroviral drugs block this process at different stages. There are six main classes, each targeting a specific part of the virus’s life cycle. NRTIs and NNRTIs stop reverse transcription-the step where HIV copies its RNA into DNA. Protease inhibitors prevent the virus from cutting its proteins into usable pieces. Integrase inhibitors block HIV from inserting its DNA into human DNA. Fusion inhibitors and CCR5 antagonists stop the virus from entering cells at all. The goal? Reduce viral load to undetectable levels-under 50 copies per milliliter. When that happens, the immune system recovers, and transmission becomes nearly impossible. This isn’t just theory. In the U.S., about 57% of people with HIV now have undetectable viral loads, up from less than 40% a decade ago. That’s the power of modern ART.Why Drug Interactions Are a Silent Threat
Most people with HIV don’t take just one pill. They’re often managing high blood pressure, diabetes, depression, or cholesterol-sometimes five or more medications at once. And that’s where things get dangerous. Many HIV drugs, especially boosted protease inhibitors like darunavir or atazanavir, are metabolized by the liver enzyme CYP3A4. So are common statins like simvastatin, sedatives like midazolam, and even some heart medications. When you mix them, one drug can flood the system with too much of the other, leading to toxicity. Simvastatin, for example, can cause fatal muscle damage when taken with boosted PIs. The Liverpool HIV Interactions Database lists 12 major drug classes that are outright contraindicated with certain HIV meds. Even newer drugs aren’t risk-free. Doravirine, a newer NNRTI, has fewer interactions than older ones like efavirenz, but it still plays nice with fewer drugs. That’s why doctors now use tools like the NIH’s HIV Drug Interaction Checker-used over a million times a year-to avoid deadly combos. Still, in community clinics, 63% of providers report delays in accessing these tools, leaving patients vulnerable.Resistance Isn’t Just About Skipping Pills
People often think resistance happens because someone forgets a dose. That’s true-but it’s only part of the story. Resistance develops when the virus mutates under drug pressure. Some mutations happen naturally. Others are triggered by low drug levels. Take lamivudine or emtricitabine, two common NRTIs. A single mutation-M184V-can make them useless. That’s why they’re never used alone. They’re always paired with other drugs to block escape routes. INSTIs like dolutegravir and bictegravir are the gold standard today because they require multiple mutations for resistance to develop. In fact, only 0.4% of people starting dolutegravir develop resistance after two years, compared to 3.2% with efavirenz. But resistance isn’t static. New strains are emerging. The experimental drug VH-184, tested in early 2025, showed promise against strains resistant to both dolutegravir and bictegravir-proof that the virus keeps evolving. Even prevention isn’t immune. A case reported in early 2025 involved someone on daily Truvada for PrEP who still contracted HIV with the M184V mutation. It’s rare, but it happens-especially if the person was already infected before starting PrEP, or if they missed doses.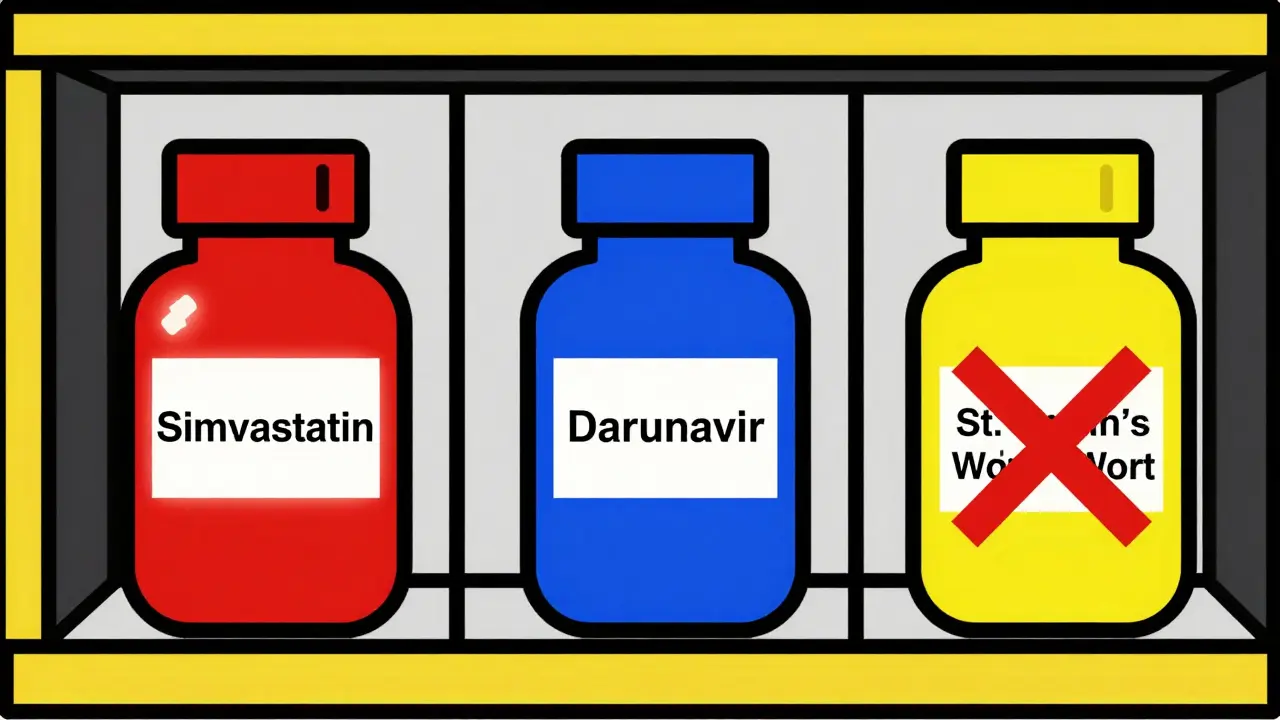
Long-Acting Injections: A Game Changer With a Catch
Monthly or twice-yearly injections like Cabenuva and the newly approved lenacapavir are changing the game. No more daily pills. No more stigma. In trials, 94% of users preferred injections over pills. But here’s the catch: if you miss an injection, drug levels drop slowly-over weeks or months. That’s not like missing a pill, where levels crash in hours. Subtherapeutic levels linger, giving the virus a long window to mutate. Dr. Sharon Lewin at the University of Melbourne warned at CROI 2025: "Missing one injection could lead to resistance that lasts for years." That’s why these treatments require strict adherence protocols and regular monitoring. They’re powerful, but they demand more discipline-not less.Genetic Testing and Personalized Treatment
Before starting any ART, resistance testing is mandatory. It’s not optional. At diagnosis, every person with HIV should get a genotype test to see what mutations are already present. In the U.S., 82% of newly diagnosed people now get tested-up from 45% in 2015. The test tells doctors: "Will this drug work?" If the virus already carries K103N, efavirenz is useless. If it has M184V, lamivudine won’t help. The Stanford HIVdb algorithm helps interpret these results, but it’s not foolproof. Community providers need 16 hours of training just to use it accurately. Infectious disease specialists get it right 98% of the time. Others? Around 85%. Pre-screening for HLA-B*5701 is another must. This genetic marker predicts a life-threatening allergic reaction to abacavir. Testing for it is standard now-and it’s saved lives. If you’re HLA-B*5701 positive, abacavir is off the table, no exceptions.Side Effects That Change Lives
Not all problems come from resistance or interactions. Some come from the drugs themselves. Tenofovir disoproxil fumarate (TDF), once a backbone of ART, causes bone density loss and kidney damage. Studies show people on TDF lose 40% more bone mineral density over 144 weeks than those on abacavir. That’s why tenofovir alafenamide (TAF) replaced it in most new regimens-it’s effective at 90% lower doses and much gentler on bones and kidneys. Efavirenz? It’s linked to nightmares, depression, and suicidal thoughts. One Reddit user described missing doses of Atripla (which contains efavirenz) because he couldn’t sleep. That’s how resistance starts-not from rebellion, but from exhaustion. In contrast, dolutegravir-based regimens like Biktarvy or Dovato are widely reported as side-effect free. In one survey of 3,215 people, 89% on these drugs said they didn’t have any symptoms that made them miss doses.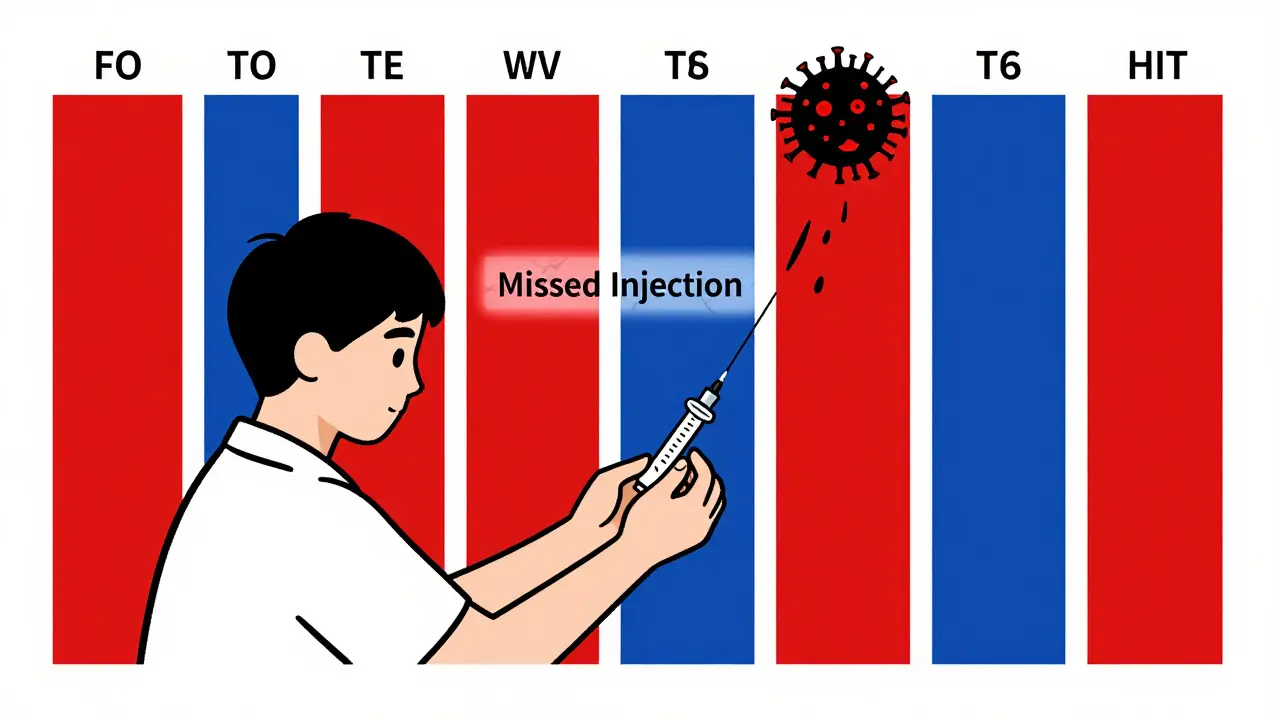
What’s Next? The Future of HIV Treatment
The future isn’t just about better pills. It’s about smarter delivery and smarter science. Lenacapavir, approved in 2022 and now recommended by WHO for prevention, is a twice-yearly injection. It’s a breakthrough for people who struggle with daily pills. ViiV Healthcare is testing VH-184, a next-gen INSTI that could bypass current resistance. Early results show it knocks down viral load by 1.8 log10 in just weeks-even in people who’ve failed other drugs. Meanwhile, researchers are using CRISPR to cut HIV DNA out of infected cells. In animal models, it reduced viral DNA by 95%. It’s not ready for humans yet, but it’s the first real shot at a cure. And AI is stepping in. Tools like HIV-TRACE use machine learning to predict transmission clusters and resistance patterns by analyzing genetic data from thousands of cases. When linked to electronic health records, it could tell a doctor: "This patient’s virus is likely to resist this drug. Try this instead."Real People, Real Challenges
Behind every statistic is a person. A man in Atlanta who switched from efavirenz to dolutegravir because he couldn’t stop crying. A woman in Chicago who lost her job because she couldn’t afford the copay on her old regimen. A teenager in rural Mississippi who missed his injection because the clinic was two hours away. Resistance isn’t a failure of science. It’s a failure of access, education, and support. Even the best drug won’t work if you can’t get it, can’t afford it, or can’t remember to take it. The tools exist. The science is advancing. But the human side? That’s still the hardest part to fix.Can you become resistant to HIV medication if you miss a dose?
Yes, especially with drugs that have low resistance barriers like efavirenz or lamivudine. Missing even one or two doses can let the virus replicate under drug pressure, leading to mutations. Newer drugs like dolutegravir or bictegravir are harder to resist, but they’re not immune. Consistent dosing is critical-especially with long-acting injectables, where missed doses can cause resistance to last for months.
What’s the most common drug interaction with HIV meds?
The most dangerous interaction involves boosted protease inhibitors and certain statins like simvastatin or lovastatin. These combinations can cause severe muscle damage or even rhabdomyolysis. Other risky pairs include midazolam (a sedative) and some anti-epileptic drugs. Always check an interaction database before adding any new medication, even over-the-counter ones like St. John’s wort, which can drop HIV drug levels by 60%.
Why are INSTIs now the first-line treatment for HIV?
INSTIs like dolutegravir and bictegravir have the highest resistance barrier of any HIV drug class. They require multiple rare mutations for the virus to escape, making treatment failure rare. They’re also better tolerated than older drugs-fewer side effects like depression, liver toxicity, or bone loss. Plus, they work fast and are effective even in people with transmitted drug resistance.
Is resistance testing really necessary if I’ve never missed a dose?
Yes. Up to 16.7% of new HIV diagnoses in the U.S. show transmitted drug resistance-meaning the person was infected with a strain already resistant to common drugs. Even if you’ve been perfect with your meds, you could still be starting on a regimen that won’t work. Testing at diagnosis is the only way to know what drugs will actually work for you.
Can I switch from daily pills to injections if I’m doing well?
If you’ve been virally suppressed for at least six months and have no history of resistance, switching to long-acting injectables like Cabenuva is a safe and effective option. But it’s not automatic. Your provider will need to run a resistance test, confirm your viral load is undetectable, and ensure you can commit to monthly or biannual clinic visits. If you’ve had prior treatment failure or resistance, injections may not be an option.
Are generic HIV drugs as good as brand names?
For most NRTIs like tenofovir or lamivudine, yes-generics are bioequivalent and just as effective. But for newer drugs like dolutegravir or bictegravir, generics aren’t widely available yet. Even when they are, switching from a brand-name combination like Biktarvy to separate generics can increase pill burden and risk errors. For people with complex histories or resistance, staying on the original regimen is often safer.